Review Article - (2017) Volume 3, Issue 1
Sowunmi OA, Onifade PO and Ogunwale A
Neuropsychiatric Hospital, Aro Abeokuta, Nigeria
*Corresponding Author:
Onifade Olutunde Peter, Ogunwale Adegboyega
Neuropsychiatric Hospital Aro Abeokuta, Nigeria
Tel: +2348035061082
Email: oniffpo@yahoo.com
Received date: April 18, 2017; Accepted date: May 5, 2017; Published date: May 3, 2017
Citation: Sowunmi OA, Onifade PO, Ogunwale A. Psychological Disorders and Its Relationship with Job Dis-Satisfaction among Correctional Officers. Clin Psychiatry 2017, 3:1. doi: 10.21767/2471-9854.100039
Copyright: © 2017 Sowunmi OA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Workers who reported satisfaction with their work have been found to be healthier than those who were not satisfied and job satisfaction correlates with global measures of mental health stability as documented by the World Health Organization. The aim of the study was to determine the prevalence of psychiatric morbidity and their relationship with job dissatisfaction among prison officials in Abeokuta.
Methods: A census of all correctional officers was conducted at the first stage during which they were screened for ‘probable psychiatric morbidity’ and Job satisfaction. Those with a probable psychiatric morbidity and 15% of those who were GHQ-negative were evaluated for definite psychiatric morbidity.
Result: The result showed that 26.7% of respondents had probable psychiatric morbidity with a weighted prevalence of psychiatric morbidity of 46.1%. Dissatisfied correctional officers were five times more likely to have a psychiatric disorder.
Conclusions: Correctional officers are at risk of experiencing psychiatry morbidity like any other occupational group. Mental health strategies including education and screening should be integrated into the health management culture of the prison organization for the purpose of preventative and early intervention.
Keywords
Psychological disorder; Satisfaction; Relationship; Mental health
Introduction
The role of occupation in the dynamics of health and diseases has long been recognized [1-4] and workers who reported satisfaction with their work have been found to be healthier than those who were not satisfied [5,6].
New work-practice and rapid technological advances have changed the nature of many jobs and employees are regularly being required to work well beyond their contracted hours, often unwillingly, while organizations struggle to meet tight deadlines and targets [7,8].
These demands have negative impact on job satisfaction and, by extension, damaging effect on the mental health of employees [9,10].
Prison is one of those work place where [11] prison officials, among others, are expected to identifying the causes of the prisoners’ anti-social dispositions, setting in motion mechanisms for their treatment and training for eventual reintegration into society as normal law- abiding citizens after their release from prison. These seemingly conflicting roles of custody and rehabilitation of prison inmates have been suggested to impact negatively on the mental health of prison officers [7]. Although several studies have examined prisoners, only a few published studies are known to have been conducted among correctional officers in Nigeria and even the few reported ones were carried out by social scientists who could not consider the effect of psychiatric disorders in their studies. The aim of the study was to determine the prevalence of psychiatric morbidity and their relationship with job dissatisfaction among prison officials in Abeokuta.
Methods
The study was done in two stages. The first stage involved eliciting participants’ socio-demographic data and screening of participants for psychiatric morbidity using the 28-item version of the General Health Questionnaire (GHQ-28) and their level of job satisfaction using Minnesota Satisfaction Questionnaire (short version) (MSQ). The instruments were numbered against the name of individual participant, in order to enable the investigator to identify those that would be included in the second stage of the study. The second stage involved clinical interview of all the participants who are GHQ-positive and randomly selected 15% (in order to minimize observational bias) of those who were GHQ-negative, using the M.I.N.I International Neuropsychiatry Interview-Plus.
The duration of the study was three (3) months. In the first stage, a total of one hundred and ninety one (191) participants were recruited.
Out of these 191 Correctional officers that were surveyed, 51 (26.7%) participants who were GHQ-positive were interviewed in the second stage of the study with the Mini International Neuropsychiatric Interview (M.I.N.I PLUS). In addition to those that were GHQ positive, fifteen percent (n=21) of participants who were GHQ negative were randomly selected and interviewed in the second stage in order to minimize observation bias. Hence, a total of 72 participants were interviewed with the M.I.N.I PLUS in the second stage of this study.
The response rate in the second stage of the study was 64% (n=46). Thirteen (6.8%) participants could not be traced, 7 (3.7%) declined the interview and 6 (3.1%) (n=6) had been transferred outside Abeokuta prison formation. A research assistant was employed to assist in the administration and analyzing of the first stage of the study. Participants who required more attention based on the interview were referred to appropriate consultants for treatment.
Results
Socio-demographic variable
Table 1 shows the socio-demographic characteristics of the participants. The ages of the participants ranged between 24 to 60 years, with a mean of 40.27 years (± 7.73). The majority 106 (55.5%) of participants were young adults, males (77%), married (91.1%), had one wife/husband (91.1%), had two children or less (48.2%), had five or more dependents (36.6%). The minimum length of service of participants was 1 year, the maximum was 35 years. The mean length of service was 14.95 years (S.D 9.92) and ordinary or higher national diplomas accounted for 53.9% of participants.
| Characteristic | n | (%) |
| Age (Years) | ||
| ≤ 40 | 47 | (24.6) |
| >40 | 59 | (30.9) |
| Means(S.D.)year | 40.27 | (7.73) |
| Gender | ||
| Male | 147 | (77.0) |
| Female | 44 | (23.0) |
| Marital Status | ||
| Married | 174 | (91.1) |
| Divorced/separated/widowed/Never married | 17 | (8.9) |
| Number of Wives/Husband | ||
| 0 | 11 | (5.8) |
| 1 | 174 | (91.1) |
| 2 | 6 | (3.1) |
| Number of Children | ||
| 0-2 | 92 | (48.2) |
| 3-7 | 99 | (51.8) |
| Number of Dependents | ||
| 0-2 | 69 | (36.1) |
| 3-4 | 52 | (27.2) |
| 5-10 | 70 | (36.6) |
| Length of Service (Years) | ||
| 0-10 | 82 | (42.9) |
| 11-20 | 46 | (24.1) |
| 21-35 | 63 | (33.0) |
| Mean (S.D.)years | 14.95 | (9.92) |
| Monthly Salary (Naira) | ||
| <60000 | 62 | (32.5) |
| 61000-140000 | 83 | (43.5) |
| 141000-270000 | 46 | (24.1) |
| Level of Education | ||
| Primary and secondary education | 19 | (9.9) |
| Diplomas (OND and HND)* | 103 | (53.9) |
| Degree and other higher education | 69 | (36.1) |
| Rank | ||
| Assistant cadre | 62 | (32.5) |
| Inspectorate/superintendent cadre | 83 | (43.5) |
| Controller cadre | 46 | (24.1) |
| ** No social activity excluded, OND=Ordinary National Diploma, HND=Higher National Diploma, SD=standard deviation. | ||
Table 1: Sociodemographiccharacteristics of participants.
Job dissatisfaction and satisfaction
Table 2 shows the level and frequency of job dissatisfaction and satisfaction among correctional officers. The minimum score on the Minnesota Satisfaction Questionnaire (short version) was 20, the maximum score was 100. The mean score was 70.81 with a standard deviation of ±14.9. The median value was 73.
| Levels | n | (%) |
| Dissatisfied | 48 | (25.1) |
| Average satisfaction | 100 | (52.4) |
| High satisfaction | 43 | (22.5) |
Table 2: The level and frequency of job satisfaction.
The scores of the job satisfaction were categorized into low (dissatisfied), high levels of satisfaction (satisfied), using the ≤ 25th and > 25th percentiles. The cut of scores were ≤ 61 and >61 respectively for the different percentiles. Forty eight (25.1%) were dissatisfied and 143 (74.9%) were satisfied.
Probable psychiatric disorder
The administration of GHQ-28 showed that 51 (26.7%) of participants were found to have a score of 5 and above: These individuals were classified as having probable psychiatric morbidity (i.e. GHQ-positive). They were subsequently interviewed for definite psychiatric disorder(s). However, 140 (73.3%) participants had a score of 4 and below, these participants were classified as having no psychiatric morbidity. Therefore, the prevalence of probable psychiatric disorder among Correctional officers was 26.7% (Figure 1).
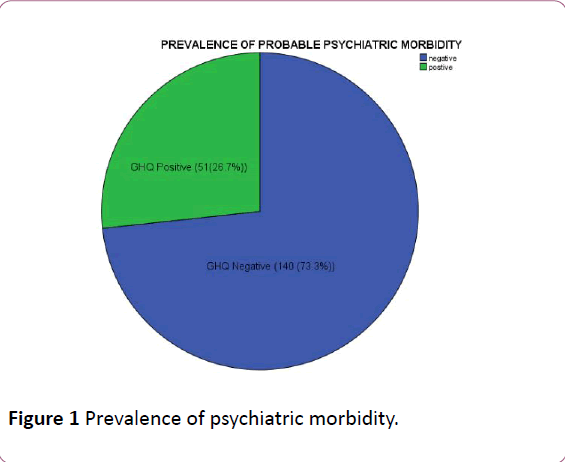
Figure 1: Prevalence of psychiatric morbidity.
The prevalence was calculated using the Horvitz-Thompson estimator [12]. The frequency of respondents who were GHQ positive was 51. Out of this number, seventeen were excluded because they were lost to follow-up and could not be reached for stage 2 (n=34).
Thus, thirty-four (34) participants representing all those eligible for the second stage were successfully recruited for the MINI-PLUS interview. The sampling weight of the 34 participants at the second stage was thus 34/34 which was equal to 1. The frequency of respondents who were GHQ negative was 140. Out of this number, nine were excluded because they were lost to follow-up (n=131). Twelve respondents who were GHQ-negative were thus eligible for inclusion in the second stage of the study. The sampling weight of the 12 participants was 131/12 which was equal to 10.92. This is illustrated in Table 3.
| Respondent Status | n | Sampling Weight, wi | nwi | wiyi | ∑wiyi | ∑wiyi/ ∑ wi |
| GHQ +ve | 34 | 1.00 | 34 | 21 | 76 | 0.4606 |
| MINI-PLUS +ve (yi) | 21 | |||||
| MINI-PLUS -ve | 13 | |||||
| GHQ -ve | 12 | 10.92 | 131 | 55* | ||
| MINI-PLUS +ve (yi) | 5 | |||||
| MINI-PLUS -ve | 7 | |||||
| *approximated to the nearest whole number; -ve=negative; +ve=positive | ||||||
Table 3: The weighted prevalence of psychiatric morbidity.
Discussion
The level of job dissatisfaction/satisfaction
In this study, a quarter of the participants were dissatisfied, although more than half of the participants experienced average satisfaction. The level of job dissatisfaction is similar to the findings in studies done among teachers in Abeokuta [13] and among civil servants from Singapore [14], where 25.7% and 22% of participants were dissatisfied respectively. Studies have identified different levels of job dissatisfaction among other occupational groups in Nigeria which include studies among police officers, teachers, doctors and psychiatrists [15,16,6]. The figures reported in these studies are comparable to what was found in this study except in health workers among whom the level of dissatisfaction was much higher (more than half of the participants). This difference may be explained by the observation that the conceptualization of job dissatisfaction may be different in various occupational groups or it may be due to the differential demands of jobs [17].
Prevalence of probable psychiatric morbidity
It was observed that more than a quarter of participants were GHQ positive, with this implying probable psychiatric morbidity. This finding is quite comparable with that obtained by Badru [18] in a study of prison officers in Agodi prison, Oyo state in which a prevalence rate of 33.1% for probable psychiatric morbidity was observed. Morrison et al in another prison study found probable psychiatric morbidity in 37.4% of male prison officers and 30.2% in female officers. Fitzgerald et al. in Australia reported that over 33% of Correctional officers had probable psychiatric disorder. Compared to other occupational groups, the prevalence of probable psychiatric morbidity among doctors at the university of Benin teaching hospital was reported to be 14% [6]. Yussuf et al. conducted a number of studies on psychiatric morbidity among workers and found that two out of ten tertiary hospital consultants had probable psychiatric morbidity; about the same proportion was observed to have probable psychiatric morbidity among bank workers in a northern Nigerian setting [19,20]. Interestingly, a similar proportion of nursing staff of a Nigerian university teaching hospital reported probable psychiatric morbidity [21]. In a comparative study also conducted by the same authors, they however reported that resident doctors had a higher prevalence of probable psychiatric morbidity than nurses and consultants [22].
Broadly speaking, it would appear that the prevalence rate of probable psychiatric morbidity among prison officers is higher than what is found in some other occupational groups. One plausible reason for this higher rate among prison officers is the impact of working under pressure within the correctional settings with its attendant characteristic of exposure to various forms of danger such as threat to life, risk of being held hostage during prison riots or frank jail breaks, etc. In addition, correctional officers work for long hours [23] with no guarantee of safety. Furthermore, the paramilitary work environment does not easily accommodate complaints related to long hours of work or worries about merely perceived threats from a dangerous population. Against this back drop, it is not impossible that a form of learned helplessness on the part of the prison officer could develop which may then present as psychological disturbance and thus account for the higher prevalence observed in this study. This is in keeping with the study by Lennart [24] on learned helplessness at work where he opined that work characteristic associated with little control, influence, learning and development imply risks of helplessness learning and these characteristics are readily observed in the prisons as a work environment. The custodial work environment being a ‘closed circuit’ setting has been observed to be associated with viral and respiratory problems among correctional officers [25] and such illnesses have been hypothesized to increase susceptibility to the development of psychological disorders and thus account for the higher prevalence in this occupational group. In addition to workrelated factors, it is also possible that response bias could have played a part in the higher prevalence rate observed among prison officers. Morrison, et al. [25] noted that correctional officers have a bias for reporting psychological distress when compared to physical distress. This may explain the higher prevalence of probable psychiatric morbidity (which may be broadly regarded as ‘psychological distress) observed in this study.
Prevalence of psychiatric morbidity
This study found a prevalence rate of 46.1% for definite psychiatric morbidity in prison officers. This rate applied to any form of definite psychiatric morbidity. This finding is similar to what was reported (38-47%) by Bourbonnas [26,27] in two different studies among correctional officers in Canada. A similar prevalence rate (40%) was also reported by Goldberg, et al. [28] among correctional officers in France. The prevalence rate observed in this study is within the 27 - 80% previously reported in studies of other occupational groups [28-31,32]. While still within the range reported, Bourbonnas opined that correctional officers reported relatively higher rates when compared to other occupational groups [26]. This he observed could be related to low decision latitude and lack of social support from supervisors which is commonly experienced among correctional officers at their place of work. Social support from supervisors was opined to be perceived by correctional officers as autonomy at work and associated with a sense of involvement in decision making process which when present may serve as a protective factor. Also, research has suggested that ‘idiom of distress in the context of psychological disorders tend to vary among cultures [33]. It is quite possible that the prison environment as a subculture could be such that correctional officers tend to manifest emotional distress in different forms of psychological disorders. Furthermore, in addition to fairly general ‘threats’ in everyday life, correctional officers are likely to experience more threatening stimuli in the prison environment. This becomes more relevant with the possibility of their re-deployment to prisons located in states facing the recent waves of insurgency and religious fundamentalism in Nigeria. The possibility of jail breaks, the increased perceived need for personal safety and the prevailing political climate may be associated with pervasive state of anxiety which may have contributed to the rate found in this study. Moreover, the need to ensure safety within the prison by double checking and counting prisoners and locks may be associated with traits related to obsessive compulsive disorder [23] which is a specific psychiatric disorder present with the rubric of any psychiatric disorder utilized in this study. Furthermore, in order to ameliorate the possible effect of anxiety, pervasive uncertainty, threat to life and traumatic events, correctional officers have been reported to use psychoactive substance [34]. This may have contributed to the higher rates observed in this study. Another possibility that could account for the higher prevalence is the failure of correctional officers to go on vacation possibly due to the security challenges in recent times in the country. This lack of vacation might have prolonged their exposure to adverse psychosocial work environment [27] which probably led to the higher prevalence of psychiatric morbidity among them.
The Relationship between Job dissatisfaction and psychiatric morbidity
The first hypothesis which stated that there is no association between the level of job dissatisfaction and psychiatric morbidity among prison officials in Abeokuta, Ogun State, Nigeria was rejected in this study. This finding is in keeping with the meta-analysis done by Faragher, et al. where they opined that job dissatisfaction was much more strongly associated with mental/psychosocial problems; strongest relationships were found for burnout (corrected r=0.478), self-esteem (r=0.429), depression (r=0.428), and anxiety (r=0.420). Faragher opined that workers with low levels of job satisfaction are most likely to experience emotional burn-out, to have reduced levels of selfesteem, and to have raised levels of both anxiety and depression. Most of respondents spend a considerable proportion of their waking hours at work and as a result dissatisfied worker may have prolonged hours of exposure to work-situation that predispose, precipitate or perpetuate psychiatric morbidity [7]. They opined that if their work is failing to provide adequate personal satisfaction or even causing actual dissatisfaction they are likely to be feeling unhappy or unfulfilled for long periods of each working day. It seems reasonable to hypothesize that such individuals are at increased risk of experiencing a lowering of general mood and feelings of selfworth while at work, cumulating in increased susceptibility to psychiatric morbidity and if these factors continued unresolved for any length of time, such emotions could eventually result to emotional exhaustion, particularly when the individual is unable to prevent their feelings from spilling over into their home/social life. This may explain why job dissatisfaction was predictive of psychiatric morbidity in this study.
The finding of a positive relationship between job dissatisfaction and psychiatric morbidity was also reported by karim, et al. [35]. They opined that problem with sleep may be observed in workers that are involved with shift work, these sleep problems may be associated with psychiatric morbidity. This can be explained by the fact that sleep problem (insomnia) itself is a primary psychiatric disorder, as well as a common associated feature of anxiety, depression and hostility. Insomnia has been reported to be associated with increased feelings of hostility and fatigue and decreased feelings of joviality and attentiveness, and to correlate negatively with job satisfaction [35]. Also, psychiatric morbidity associated with anxiety, depression or hostility has negative effects not only on quality of life and psychosocial competence, but also on the productivity and quality of job performance. This ultimately affects the perception of job satisfaction among employee in a work environment which ultimately may result in psychiatric morbidity.
Furthermore, Takuda, et al. [36] in their pathway model showing the pathways to burnout and mental ill-health from poor working conditions indicated that poor work control and heavy on-call duty are directly associated with job dissatisfaction and indirectly associated with burnout and poor mental health. One of the major problems in correctional work environment is the state of disrepair of the facilities correctional officers have to work in [23]. These unconducive work environment will most likely increase the burden of work and indirectly have increased the susceptibility of correctional officers to the development of psychiatric disorders as suggested by the pathway model. This is a possible reason why job dissatisfaction was predictive of psychiatric morbidity.
The findings in this study draw attention to relatively few studies addressing the nature of job dissatisfaction as it pertains to the occurrences of psychiatric morbidity among correctional officers in this environment and that job dissatisfaction is a predictor of psychiatric morbidity among correctional officers. Furthermore, there is a need to focus on knowledge that will help in the development of preventive strategies against mental ill health and provide treatment as well as rehabilitation for officers with psychiatric disorder in the work place. Finally, in order to build a positive work culture, mental health issues can be ameliorated by the development and implementation of mental health policy, active leadership and systems that identify psychological problems early and to regularly review as well as improve the strategies developed to address them. It is expected that reduction in the level of job dissatisfaction, as well as improvement in mental health should ensure a more productive workforce within the Nigerian correctional system.