Research Article - (2015) Volume 23, Issue 5
Honorary Research Fellow, Cochrane Institute Cardiff University, United Kingdom
Secretary to Hywel Dda University Health Board sensory loss group
In this paper, experience of delivering the Welsh sensory loss standards for visually impaired patients in 8 General Practices in mid Wales is reported. In September and October 2013, 8 General Practices in a locality cluster called north Ceredigion were contacted with a short briefing paper and questionnaire. In addition, a questionnaire survey was undertaken a Visually Impaired Club in the same area, with 14 responses received. Taking the 2 sets of results together, there appears to be a need to improve staff awareness, which can only help improve the service quality and dignity in care of all patients with sensory loss. The potential context of the work in future is co-production, with possibly extension to other primary care contractors and also to patients with hearing impairment. The experience reported in this paper, however, does have methodological limitations, for example sample size and statistical robustness, although it still provides a useful insight to help drive quality improvements.
visual impairment, Wales, primary care, standards
Visual impairment affects a significant proportion of the population. For example, a Medical Research Council study found approximately [1] in 10 of the population over the age of 75 are affected (12.4%, 95% confidence intervals 10.8% to 13.9%). Furthermore, evidence suggests that patients with visual impairment have more physical and mental health conditions compared to those individuals without visual impairment.[1,2] The implications of this are far reaching, for example screening for hearing loss or depression in eye care services.[2]
Wales is one of the countries of the United Kingdom. Since 1999, it has had a devolved Welsh Government with powers over healthcare. In December 2013, the Welsh Government Minister for Health launched the 'Sensory Loss Standards for Wales'.[3] The standards were broad and set out a challenge to the Welsh National Health Service (NHS) to improve the way that patients with sensory loss receive care in three service settings, namely primary, secondary and unscheduled care.
The Welsh standards reflect the Equality Act 2010 in which needs are to be anticipated and reasonable adjustments made. There are five standards that need to be taken into account, namely identifying patients with sensory loss, communicating with them, training of staff, environmental considerations such as signage and raising concerns or complaints. Similar initiatives are being progressed elsewhere, such as the Accessible Information Standard in England.
In Wales, 7 Health Boards provide integrated NHS services while [3] Trusts provide ambulance services, public health functions and cancer care. The area of mid and west Wales is served by Hywel Dda University Health Board (HDUHB) with a resident population of about 375,000 people. HDUHB also provides some services to patients in central and north-west Wales on behalf of two other Health Boards.
The service configurations and opportunities for Wales have been presented elsewhere.[4] In this paper, experience of delivering the sensory loss standards with respect to visually impaired patients in 8 General Practices in mid Wales is reported. The experience is set in the area including and surrounding the University town of Aberystwyth on the coast of the local government county of Ceredigion. This setting was selected partly because a regional eye clinic is also located in the town.
During September and October 2013, 8 General Practices in a locality cluster known as north Ceredigion were contacted with a short briefing paper and questionnaire as shown in Box 1. The names of the 8 practices included are: Borth, Church Street, Llanilar, Oxford Street, Padarn, Tanyfron, Tregaron and Ystwyth. Four of these practices (Church Street, Llanilar, Padarn, Ystwyth) are located within or near to Aberystwyth with the other 4 located in surrounding districts.

Box 1: Questions put to 8 general practices in north Ceredigion
The questions within Box 1 were developed as follows. Within the standards, a number of requirements were presented and these fomed the basis of the questions with respect to accessible policy. This allowed a focal point for the interviews with the practices, rather than engaging too broadly across too many issues. Each question was considered equally important so was therefore given a score of 1 point and given the number of questions posed, a maximum score of 7 was possible. In addition to this, open ended questions were asked to allow the collection of qualitative information.
In addition, to help develop a sensory loss action plan, a questionnaire survey was undertaken by HDUHB with a wide range of groups in the summer of 2014. This included national Charities, such as Action on Hearing Loss and Wales Council for the Blind, local authority partners and patient groups such as Deaf Clubs. They were approached through an overarching steering committee called the Sensory Loss Standards Implementation Group via email with an invitation to circulate widely. Through this, another group responded, namely Aberystwyth and District Visually Impaired Club (ADVIC).
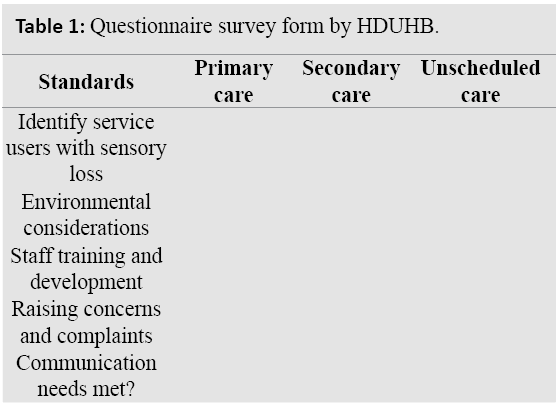
The questionnaire asked for comments and improvement ideas about the experience of services within primary, secondary and unscheduled care. Table 1 presents a summary of the questionnaire. From this summary, it is possible to see that there are 15 permutations, namely 5 standards and 3 service settings.
In administering the questionnaire, participants were offered the opportunity to receive different formats, for example braille. They were also offered to opportunity to contribute in different ways, e.g. face to face or via telephone. The author also attended an ADVIC meeting.
Practices were assured that their scores and comments would be treated anonymously. Table 2 presents a summary of main results and scores. The table shows the variation of scores and experience but the common factor was that practices claimed to know their population and were committed to person-centred care for all sensory loss patients. This included hearing loss, hence the reference to portable hearing loop. In summary, the practices took pride in their work and sought to provide patient centred services, with an appetite for improvement.

Fourteen responses were received from Aberystwyth & District Visual Impaired Club (ADVIC). The qualitative responses are given below and ADVIC scored primary care highly with an average score of 74%. Unscheduled care and secondary care average results were similar at 66% and 63% respectively. It should be noted, however, that there was a wide variation of scores that ranged from not scored to 100%. This is why an average is presented although the wide range infers strong feelings from the respondents in that a poor experience could lead to a very low score while a positive experience a high score. Given these averages are comparing like with like, they do have internal validity from the sample.
Some of the comments received included the need for ‘help getting to consulting room’, ‘tactile marking…would be helpful’ and ‘lack of privacy’. Perhaps the overarching comment of most relevance is that ‘staff require more awareness training’, which has the potential to resolve the previous comments and future proof the services delivered.
With respect to a response rate, this was 100% for the practices but remains unknown for ADVIC. Members of ADVIC tend to vary in their attendance, due to many reasons such as competing personal commitments or current health circumstances. Given the response rate is unknown, the feedback provided must be taken as comments personal to the individual, hence the reason for presenting an aggregated score.
HDUHB had anticipated the launch of the standards and had convened a multi-disciplinary and multi-agency Sensory Loss Standards Implementation Group (SLSIG) as early as September 2013. This current project had two key drivers to it, namely as part of an Improving Quality Together (IQT) training programme attended by the author and also to help develop the SLSIG action plan for HDUHB.
Leaving aside statistical objections, taking the 2 sets of results together, it appears that the general practices have further needs to improve the services they deliver. Notwithstanding the methodological limitations behind the data collected, including subjective measures plus limited sample size, it is still possible to draw out some points with a reasonable degree of confidence. The first of these is the need to improve staff awareness, which can only help improve the service quality and dignity in care of all patients with sensory loss. This is a much needed initiative to build on prior work.[5] Contractual mechanisms, such as Quality and Outcome Framework, might also offer further levers to improve the services in this context.[6]
As well as plans to offer an awareness raising session to the 8 practices, there are also plans to provide the practices with a communication guide plus symbols on a poster. The combined impact of all of these is intended to provide an improved service for all patients with sensory loss, with ongoing discussion with ADVIC being the observatory for success or further intervention. Indeed, the relationship with ADVIC is an example of co-production that underpins NHS services in Wales. Co-production might be considered to be relationship building between patients, carers, NHS organisations and other partners to reach shared understanding on the design, delivery and monitoring of healthcare services. Co-production also implies a joint accountability on the effectiveness of services provided.[7]
There is also the possibility of extension to other primary care contractors and also to patients with hearing impairment. The former includes of pharmacists and dentists where potentially the experience reported by this paper could be repeated in these different situations. Furthermore, the focus of this paper has been on visual impairment so the expansion to hearing loss seems a logical next step, perhaps working with one of the local Deaf Clubs.
Other avenues of improvement might include the Low Vision Service Wales (LVSW), which is a nation wide initiative hosted by HDUHB. This is provided in community optometry practices and fortunately LVSW are a part of SLSIG and provide valuable input. There might be opportunities to work with LVSW to undertake similar improvements to those reported in this paper. Another productive line might also include Information Technology (IT) initiatives, such as ‘My health on line’. At a national level, work is being progressed on the role of IT via the National Wales Informatics Service (NWIS).
The experience reported in this paper, however, does have methodological limitations, for example sample size and statistical robustness, although it still provides a useful insight to help drive quality improvements. It is conceded that a larger sample size is needed and that combining two different metrics is not statistically valid. In balance to these objections, however, it can be noted that the driver was one of real time and real world improvement, which this study achieves.
The context of co-production with ADVIC has now been extended to examine the service model of the eye clinic, known locally as ‘North Road Eye Clinic’. This clinic directly provides a range services as a regional centre 'serving surrounding population'
The author would like to thank the north Ceredigion practices for their input, members of ADVIC and SLSIG for their support on the action plan and Jackie Hooper, Peter Llewellyn and Michelle Dunning in HDUHB for their invaluable advice, support and encouragement during this work.