Keywords
Inequity in healthcare; Treaty of Waitangi; Institutional racism; Interpersonal racism; Internalized racism; Indigenous people.
Introduction
Racial inequities in cardiovascular disease in New Zealand
Worldwide, cardiovascular disease (CVD) is the topmost cause of death and equally one of the most preventable causes of mortality. Coincident with rapid economic development across the world CVD is a considerable burden on healthcare resources in both the developed and rapidly developing countries [1]. CVD is the leading cause of death in Aotearoa/New Zealand, that annually accounts for 40% of all deaths, with proportionally more deaths per 100 000 occurring in MÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâÃÂori [2]. Diminished life expectancy is one example of racial inequity in healthcare between MÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâÃÂori and PÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâà(the non-indigenous population). Ischaemic heart disease (IHD), a major cause of CVD deaths, accounts for 40.2% of MÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâÃÂori deaths from this condition in those aged less than 65 years, compared to 10.5% of PÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÂÂÃâàdeaths [3].
The literature is replete with studies pertaining to ethnic inequities in healthcare. A thorny subject that has been described for decades and yet has few remedial solutions. The pattern of ethnic inequities in healthcare is a global phenomenon that is not confined to any specific race or culture. The socio-economic, cultural and environmental conditions in which people live greatly influence their chances of being healthy.
“Indeed factors such as poverty, social exclusion and discrimination, poor housing, unhealthy early childhood conditions and low occupational status are important determinants of most diseases, deaths and health inequities between and within countries” [4].
The main determinants of health have been conceptualised as a complex, layered spectrum of factors generated by the macropolicy environment such as neo-liberal economic growth strategies that have widened the gap between the rich and the poor [5]. Suggest four interdependent factors that can be grouped together as spheres of influence that impact health and which may form the basis of a health policy intervention (Figure 1). The main influences that affect health can be described as; promoting health; protecting health; and threatening health.
Dahlgren and Whitehead warn that all too often strategies are aimed at correcting a single level of influence, whereas interventions that address several levels may be more effective [5]. Equally evident is that positive actions at one level may be offset by negative actions at other levels; e.g. health education for young people being nullified by insufficient funds for school lunches [5]. Surviving and living a healthy life remain closely related to the socioeconomic background of individuals and families that are reflected in substantial and ever increasing social inequities in health [6]. However, very few countries have developed strategies for the integration of equityoriented health policies into economic and social legislation. The reduction of inequities in the health status between less privileged socioeconomic groups and their more privileged counterparts, Dahlgren and Whitehead suggest should be key to all international, national and local health policies [6].
Race is a social construct not a biological reality typically used in a mechanical and uncritical manner as a proxy for immeasurable biological, socioeconomic and/or sociocultural factors [7-9]. Jones in an invited commentary uses an example that is true to MÃâ€Å¾Ã‚ÂÂÂÂÂÃâÃÂori and PÃâ€Å¾Ã‚ÂÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÂÃâàin New Zealand today; “Black” in the US is over-represented in poverty, but the majority of poor people are “White,” as not all Black people are poor [7]. She continues by suggesting there is no single Black culture just as there is no single White, Hispanic or Asian culture. Genetically, “races” are a heterogeneous mixture of geographic stock from many parts of the world. Race is a social classification in our race-conscious society that conditions many aspects of our lives; which then result in profound differences in life opportunities [7]. Whereas ethnicity is a reflection of our genetic and cultural heritage, race is a measure of identity imposed by society that results in the consequent societal constraints associated with that identity. The race label assigned by an investigator or volunteered by a study participant, Jones suggests, is an “excellent measure of exposure to racism” (p. 300) and that it is this aspect of race that impacts health and results in race-associated inequities that are large, occur throughout a life span and involve many different organ systems [7]. Indeed being classified as “White” by others has been shown to produce statistically significant advantages in health status, irrespective of how a person selfidentifies [15]. Associations of observer-ascribed skin colour found a significant gradient in self-rated health by skin colour; those with darker skin colour reported poorer health [16]. Perreira and Telles concluded that darker skin colouration influences self-rated health primarily by an increased exposure to class discrimination and low socio-economic status [16]. In New Zealand reported that skin colour perceived as white was advantageous and health-protective whereas the socialassignment of being MÃâ€Å¾Ã‚ÂÂÂÂÂÃâÃÂori was associated with being at risk of differential and discriminatory healthcare [17]. The routine documentation of race-associated inequities in health, without adequate explanation is not benign as it impedes the advancement of scientific knowledge, limits efforts at primary prevention, and contributes to ideas of biologic determinism [7].
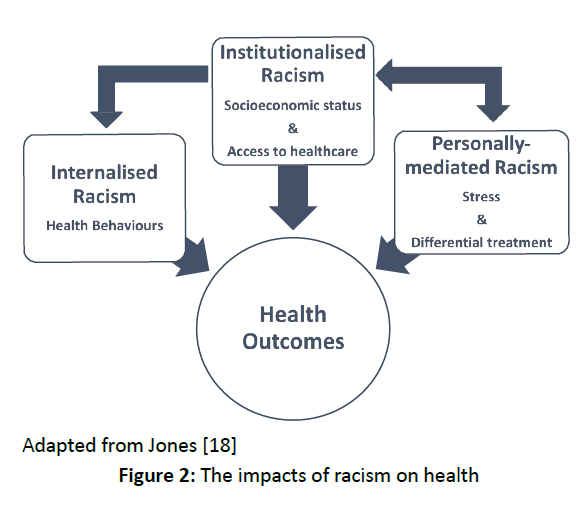
In 2000, Jones published a 3 level framework for understanding racism that included: institutionalized, personally mediated, and internalized racism. The concept of the levels that she suggested which form the basis of race-related influences in poor health outcomes [18] (Figure 2). Institutionalised racism manifests itself in differential access to material conditions, (e.g. quality education and housing) and access to political influence. Personally mediated racism is defined as prejudice and discrimination, where prejudice means differential assumptions about the abilities, motives and intentions of others according to their race and discrimination means differential actions toward others according to their race. Internalized racism is defined as acceptance by members of the stigmatized races of negative messages about their own abilities and intrinsic worth. It is characterized by them not believing in others who look like them, and not believing in themselves [18].
Figure 2:The impacts of racism on health.
The framework devised by can be superimposed upon the determinants of health stratified by [5,18]. Racism affects health partly because indigenous, minority populations often experience less favourable social and economic circumstances that allows access to healthcare, (institutionalised racism) and partly because of direct psychosocial stress caused by personally mediated racism [12,18-20]. Within New Zealand and internationally, racism is recognised as an important determinant of health [10]. Rata and Zubaran warn that it is low socioeconomic status that is the cause of MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori health disadvantages not ethnicity [21]. They argue that ethnic labelling itself may contribute to negative stereotypes that produce racism, which in turn feed the cycles of discrimination for ethnic minority groups. They suggest that public healthcare20 policies based on ethnic distinctions should be abandoned in favour of “a more tenable approach that recognizes a series of other causal factors in social disadvantage” [21]. As the current strategies are failing MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori, new initiatives addressing social disadvantage and poverty are urgently needed to redress the inequities in healthcare.
The health of indigenous people is significantly less than the non-indigenous in communities where traditional ways of life, environment and livelihoods have been taken over by the worst of Western culture e.g. unemployment, poor housing, alcoholism and drug use [22]. In Aotearoa/New Zealand from the formation of our bicultural society (MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori the indigenous peoples of New Zealand and PÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÃâànon-indigenous people) with the signing of the Treaty of Waitangi in 1840, MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori were immediately marginalised. The fabric of MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori society; tribal laws, languages, dress, sacred ceremonies, rituals, healers and native remedies were suppressed by colonial laws and regulations [23]. The dispossession of lands and subsequent poverty meant MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori could not compete equally within the imposed and dominant western culture to obtain the benefits of healthcare, education and employment. For a more detailed account of the effect of colonisation of New Zealand MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori [24-26].
However, after 176 years it is unhelpful to ascribe current inequities to intergenerational psychological trauma caused by the impact of a cataclysmic event such as colonisation rhetoric such as: “If MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori are getting less, non-MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori are getting more” [21,26,27]. If as Jackson suggests, MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori health needs arise as a consequence of their indigenous rights being breached, will MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori health improve with the reinstatement of such rights? Likewise it is naïve to argue that genetic differences are not likely to be part of the complex contributory factors for racial inequities in New Zealand when, for example, this is clearly untrue in the light of research that shows melanocortin-3 receptor gene variants in MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori are linked to obesity and the early onset of type 2 diabetes [28-32]. When seeking the reason why health inequity exists in New Zealand today it is not helpful to pound the colonisation drum. Modern health inequity requires an up-to-date reason as to why MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori have increasing rates of CVD when those for PÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÃâàare decreasing. Rata and Zubaran dismiss post-colonial trauma as the root of MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori inequities in healthcare and suggest that sociocultural factors, with or without an ethnic dimension are more likely the cause of poor outcomes in health [21]. When reviewing risk factors why are 40% of MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori males and 50% of MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori females, aged 15-64 years, continuing to smoke when only 20-21% of PÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÃâàare? Why 26% of adult MÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂori are obese compared to only 18% of PÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÂÂÃâÃÂ? Using face-to-face interview techniques of 12 500 people. Harris et al. [11] reported an association between experiencing racial discrimination and socioeconomic deprivation with smoking and CVD. Is racial discrimination and socioeconomic deprivation the cause of CVD or is CVD the result of exposure to risk factors such as smoking and obesity? It is dangerous to deflect attention away from the risk factors of CVD and blame post-colonial trauma. Likewise it is inappropriate to blame racism for the voluntary disregard of CVD risk factors such as smoking and obesity; as such factors hold the same proportion of risk for all ethnicities.
Of the many papers that outline health inequities for MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori, very few actually outline what MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori require. An exception to this is the work of who suggests that in New Zealand the availability of care is inversely proportional to the need of the population served, where those who need healthcare the most, receive the least; the inverse care law first suggested by Curtis suggest that three key factors must be addressed in order to invoke changes in health equity; a) acknowledging the role of society, b) understanding the policy imperatives, and c) exploring the clinician’s role. This approach they conclude is consistent with the human rights of MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori as tangata whenua, the rights of MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori as outlined within the Treaty of Waitangi and New Zealand health policy [33,34]. A recurrent theme in the understanding of health inequities is the way society distributes health resources, of material wealth, housing, education and employment [35]. Redressing inequities in power, money and resources should be viewed as restorative actions outlined by the Treaty of Waitangi.
Racial inequities in New Zealand and the increased risk of CVD
Although the causes of CVD in minority ethnic groups are not completely understood, researchers agree that socioeconomic factors are important. Although the classic risk factors associated with CVD vary significantly between minority ethnic groups, morbidity and mortality are much higher in these groups than in Caucasian and Asian populations [36]. The prevention of CVD across all ethnic groups relies on; identifying associated risks, establishing a safe threshold for such risks and reducing the risk factors that may precipitate the disease. The Framingham study identified 7 major risk factors; age, sex, blood pressure (BP), glucose intolerance, total and high-density cholesterol, smoking and left ventricular hypertrophy, that may be used to calculate the probability of developing CVD [37]. In addition to these risk factors the study by added; apolipoproteins B:A ratio, history of hypertension, history of diabetes, diet, inactivity, alcohol use, psychosocial stress, and abdominal obesity (which was better than BMI as a predictor of myocardial infarction in all ethnic groups) [38,39]. Population screening using risk factor analysis requires the application of a validated and reliable tool which is currently insensitive and not specific enough to apply to ethnically heterogeneous populations [36]. Other risk prediction instruments include; PREDICT, FINRISK [40], SCORE [41] and ETHRISK [42]. More controversial risk factors have been proposed and include; metabolic syndrome, micro albuminuria, waist circumference, haemostatic factors, and homo-cysteine levels [36]. In New Zealand the national guidelines for the prevention of CVD contain an age stratification which make screening very cost effective and lists: personal history of CVD; age; sex; smoking status; apolipoprotein imbalance; hypertension and diabetes as the principal risk factors [43]. The guidelines also list other well established determinants of CVD risk: atrial fibrillation; obesity; impaired carbohydrate metabolism; metabolic syndrome; nutrition and dietary patterns; physical inactivity; family history of premature CVD; socioeconomic position; depression, social isolation and social support. When using the Framingham Risk Equation the guidelines list adjustments that include ethnicity. However, evaluating the guidelines and appropriateness for screening in primary care suggests they would be more effective if they incorporated U.S. recommendations on the use of aspirin and initial antihypertensive treatment rather than on achieving blood pressure targets [44].
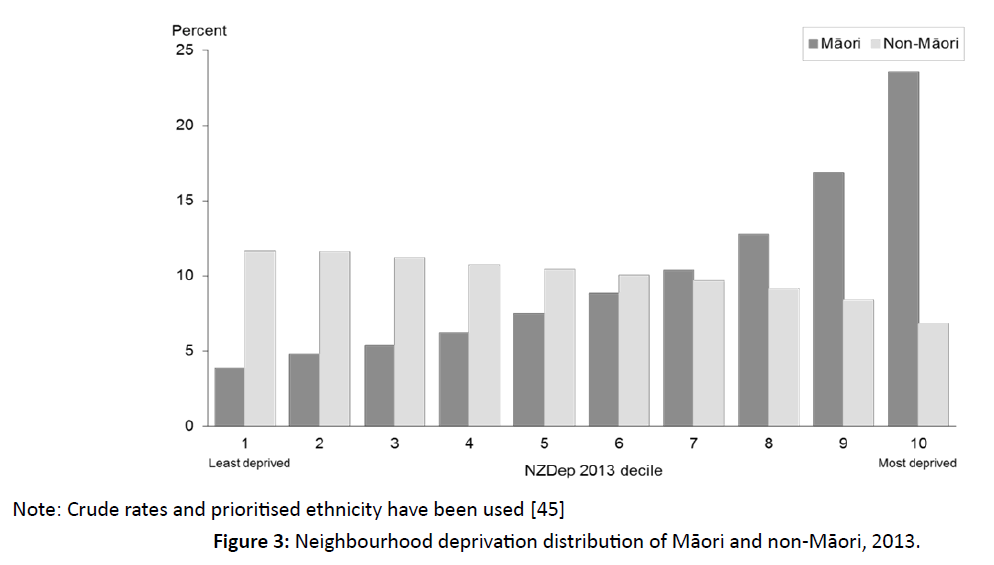
Higher proportions of MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori live in more deprived areas than non-MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori (Figure 3). In 2013, 23.5% of MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori lived in decile 10 areas compared with 6.8 percent of non-MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori. Only 3.8% lived in decile 1 areas as compared to 11.6% of non-MÃâ€Å¾Ã‚ÂÂÂÃâÃÂori).
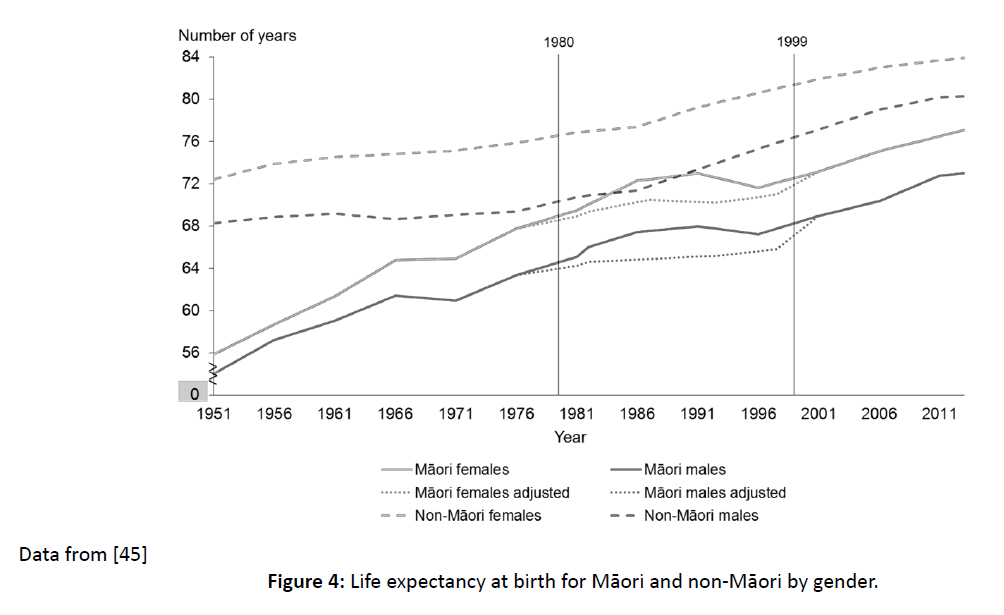
In New Zealand CVD and diminished life expectancy is one example of racial inequity in healthcare between MÃâ€Å¾Ã‚ÂÂÃâÃÂori and PÃâ€Å¾Ã‚ÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÃâà(Figure 4). Between 1951 and 2011 the life expectancy of PÃâ€Å¾Ã‚ÂÂÃâÃÂkehÃâ€Å¾Ã‚ÂÂÃâàat birth had increased steadily from 68 to 80 years for males and from 72 to 83 years for females. However, during the same period the life expectancy of MÃâ€Å¾Ã‚ÂÂÃâÃÂori males only increased from <56 to 72 years and from 68 to 76 for MÃâ€Å¾Ã‚ÂÂÃâÃÂori females [45].
Note: Crude rates and prioritised ethnicity have been used [45].
Figure 3:Neighbourhood deprivation distribution of MÃâ€Å¾Ã‚ÂÂÃâÃÂori and non-MÃâ€Å¾Ã‚ÂÂÃâÃÂori, 2013.
Figure 4:Life expectancy at birth for MÃâ€Å¾Ã‚ÂÂÃâÃÂori and non-MÃâ€Å¾Ã‚ÂÂÃâÃÂori by gender.
The standardised mortality rates for CVD in males and females are shown in Table 1. The data show that between 2010 and 2012 the total CVD mortality rate among MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori was more than twice as high as that among non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori (RR 2.17, CI 2.08-2.26). In 2012-14, MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori were more than one-and-a-half times as likely as non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori to be hospitalised for cardiovascular disease (RR 1.64, CI 1.61-1.67). The mortality rate for heart failure among MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori was more than twice that of non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori (RR 2.36, CI 1.76- 3.17), and MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori were about four times as likely as non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori to be hospitalised for heart failure (RR 4.01, CI 3.83-4.21). The inequity was greater for females where the heart failure hospitalisation rate among MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori females was nearly four-anda- half times that of non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori females (RR 4.49, CI 4.16-4.85). The mortality rate from rheumatic heart disease among MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori was more than five times that of non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori (RR 5.23, CI 3.99- 6.87) and the rheumatic heart disease hospitalisation rate for MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori was nearly five times that of non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori (RR 4.82, CI 4.23-5.51). The inequity for MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori females for rheumatic heart disease hospitalisation was greater than five times that of non- MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori females (RR 5.30, CI 4.47-6.29) [45].
In New Zealand childhood obesity is believed to be the major contributing factor in adult obesity and is associated with disease conditions such as hypertension, dyslipidaemia, type 2 diabetes and subsequent CVD. Childhood obesity is more prevalent in MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori children (11.8%) compared to those with Caucasian heritage (5.5%) [46]. Cardio metabolic health can be improved by reducing obesity and increasing cardiorespiratory fitness, however, it remains unclear whether fatness or fitness is crucial to improving cardio metabolic health and decreasing CVD risk in children [46]. In adults fitness is key to improving cardio metabolic health.
Cultures apart
A neoliberal perspective of the NZ health system has seen a shift away from a governmental health responsibility towards one of individualised lifestyle accountability. Rather than investment in the prerequisites of good health, that of income, housing and nutrition, healthcare promotion policies are cloaked in the political ideology of neoliberalism, whereby the fundamentals of health, unemployment, poverty, lack of education, all important social determinants of health are largely ignored and seen as poor personal choices made by a population who are able to rectify such social and economic conditions [47]. Such social determinants of health, once seen as a failure of the state are now viewed as a personal failure requiring personal accountability [48]. Health promotion messages of; “Five plus a day,” “Be healthy, be active”; “Eat healthy and lose weight” are widely publicised throughout Western societies, are hailed as panacea to modern day health concerns and chronic disease [47]. However, as social and economic conditions worsen the burden of treating chronic disease on national health expenditure increases exponentially [49]. Unable to afford healthy lifestyle options MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori are frequently subjected to negative stereotypes and deficit explanations that unfairly direct fault at MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori for being obese, unhealthy, and sedentary along with accusations that they make poor lifestyle choices [48,50]. Accusations such as these ignore genetic, contemporary socio-cultural and environmental factors that contribute to their unhealthy lifestyle. The imposition of neoliberal personal responsibility neglects the complexity inherent in this issue and the barriers that influence choices available to MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori [48].
| Indicator |
MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori |
Non-MÃâ€Ãâ¦Ã¾ÂÂÃâÃÂori |
| |
Males |
Females |
Total |
Males |
Females |
Total |
| Total cardiovascular disease mortality |
346.9
(328.6–365.9) |
232.3
(219.2–246.1) |
286.8
(275.7–298.3) |
168.2
(165.3–171.0) |
99.2
(97.6–100.8) |
132.4
(130.8–133.9) |
| Total cardiovascular disease hospitalization |
3725.6
(3660.3–3791.8) |
2710.2
(2658.6–2762.6) |
3186.4
(3145.3–3228.0) |
2537.2
(2522.1–2552.3) |
2552.3)
(1366.5–1385.7) |
1938.6
(1926.9–1947.4) |
| Stroke mortality, |
44.7
(38.3–51.9) |
50.6
(44.5–57.3) |
48.2
(43.7–53.0) |
30.9
(29.8–32.1) |
30.2
(29.3–31.0) |
30.9
(30.2–31.6) |
| Stroke hospitalization |
355.1
(335.3–375.8) |
374.2
(355.4–393.6) |
365.7
(352.1–379.8) |
245.1
(240.8–249.5) |
172.3
(169.2–175.4) |
207.6
(205.0–210.3) |
| Heart failure mortality, |
5.4
(3.3–8.3) |
4.9
(3.3–7.0) |
5.2
(3.9–6.9) |
2.2
(2.0–2.5) |
2.2
(2.0–2.4) |
2.2
(2.1–2.4) |
| Heart failure hospitalization |
676.1
(648.7–704.3) |
434.8
(414.3–456.0) |
547.5
(530.6–564.7) |
179.7
(176.4–183.0) |
96.8
(94.9–98.8) |
1.0
(0.9–1.2) |
| Rheumatic heart disease mortality, |
5.0
(3.6–6.9) |
5.7
(4.3–7.5) |
5.4
(4.4–6.7) |
0.9
(0.7–1.1) |
1.1
(1.0–1.3) |
1.0
(0.9–1.2) |
| Rheumatic heart disease mortality, |
27.6
(3.6–6.9) |
48.6
(43.4–54.1) |
38.7
(35.4–42.2) |
6.8
(6.2–7.4) |
9.2
(8.5–9.9) |
8.0
(7.6–8.5) |