- (2014) Volume 15, Issue 4
Preethi K John, Muhammad Wasif Saif
Tufts Medical Center. Boston, MA, USA
Pancreatic neuroendocrine tumors (pNET) are a rare malignancy. Many patients will present with metastatic disease most commonly to the liver. Currently the standard of care for treatment of liver metastases from neuroendocrine tumors (NETs) is surgical resection. However, only few patients are candidates for surgical resection and require alternative options. Given the rarity of this disease, data regarding treatment options are minimal. In this paper, we will review data presented at the annual meeting of ASCO 2014 about the Survival following Y90 radioembolization for neuroendocrine tumor liver metastases (abstract #e15166). This abstract shows evidence for survival benefit with the use of radioembolization in the treatment of metastatic neuroendocrine tumors to the liver.
Embolization, Therapeutic; Liver; Neuroendocrine Tumors; Yttrium Radioisotopes
NETs are a group of rare hormone secreting malignancies that were thought to originate from pluripotent stem cells [1]. The most common NET is carcinoid which occurs at a rate of about 2-3 per 100,000 people [2]. The majority of carcinoid tumors originate in the midgut (40-70%) [2]. However, there are some NETs that originate in the pancreas (pNET) previously known as islet tumor cells [1]. pNET occurs in about 1-2% of pancreatic neoplasms and 7% of all NETs [1]. Autopsy studies have suggested a prevalence rate of about 3-10% [1]. pNETs are comprised of non-functional and functional tumors. Functional tumors secrete active hormones that cause clinical syndromes such as carcinoid syndrome and Cushing syndrome [1]. According to SEER database about 90% of pNETs are nonfunctional [1].The remaining functional tumors consist of gastrinomas, insulinomas, VIPomas, glucagonomas, and somatostatinomas [3]. pNET functions differently from other NETs in regards to their growth rates, malignant potential, and prognosis [1, 3]. Insulinomas have a lower malignant potential compared to the other pNETs only occurring about 5-15% of the time while the rest are malignant 50-90% of the time [3]. Approximately 60-70% of pNETs present with metastases most commonly in regional lymph nodes followed by the liver [1].
The current standard of care for treatment of metastatic NET to the liver is surgical resection which is the only curative therapy [1]. Overall survival of patients after surgical resection is approximately 114 months compared to 25 months [1]. 5-year survival rates following surgical resection have been shown to be up to 60% [1]. However, less than 10% of patients with metastatic liver disease from NETs have resectable disease while being optimal surgical candidates [2]. Additionally, alternative therapies such as chemotherapy have been limited by high toxicities and low response rates ranging from 0-38% for carcinoid tumors [2]. For these patients, radioembolization has become a viable treatment option. Radioembolization is a procedure that involves injecting hepatic vessels with chemotherapeutic agents, embolic products that induce ischemia, and radioactive material aimed to destroy tumor cells [4]. Radioembolization has been found to be effective in symptomatic control of hypersecreted hormones as well as tumor debulking [4]. One retrospective study by Paprottka et al. included 42 patients with unresectable liver metastases from NET who underwent Y90 radioembolization resulting in a median decrease in tumor marker by 55% (chromogranin A) and 37% (serotonin) at 3 months. They also found that 36 out of the 38 symptomatic patients had improvement in clinical symptoms at 3 months [2]. Although it is evident that there is a role for radioembolization in palliative care for symptomatic control, data regarding survival benefit is scarce.
In the following section, we will summarize the data of Y90 radioembolization use in unresectable liver metastases secondary to NETs, which was presented in the 2014 ASCO Annual Meeting.
The 2014 ASCO Annual Meeting presented an abstract that showed survival benefit of Y90 radioembolization for the treatment of metastatic NETs in the liver.
Survival Following Y90 Radioembolization for Neuroendocrine Tumor (NET) Liver Metastases: A Retrospective, Single-Center Analysis
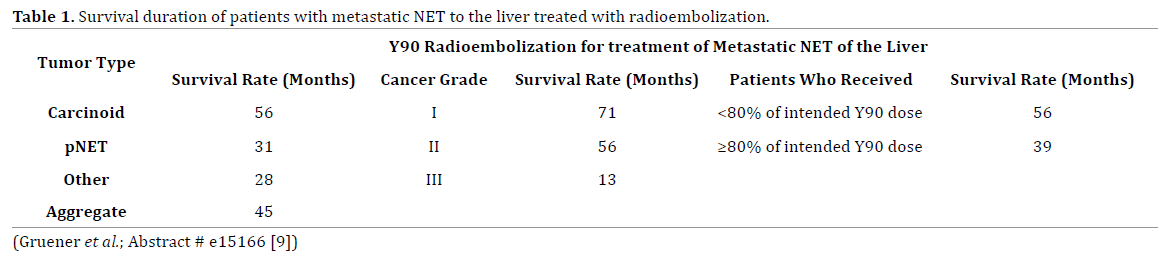
Gruener et al. presented a retrospective study of 111 patients with metastatic hepatic NET who underwent Y90 radioembolization [9]. This pool of patients was taken from a single institution from 2004 to 2012 that did not have prior chemoembolization treatments. Of the 111 patients, 76 had carcinoid tumors, 25 had pancreatic NETs (pNET), and 10 had unclassified NETs. Most of the patients had grade 1 or grade II tumors. Of the 111 patients, 24 patients had <80% of the total Y90 dose. The results of this study are listed in Table 1 below. The overall median survival was 45 months from the date of procedure but differed based on the type of NET as well as tumor grade. Carcinoid tumors had the highest median survival at 56 months compared to 31 months in the pNET group and 28 months in the unclassified NET group. Grade 1 tumors had median survival of 71 months compared to grade II with 56 months, and grade III with 13 months. It was also found that patients who received <80% of the intended Y90 dose had a higher medial survival at 56 months compared to 39months.
The management of NET is evolving as it is for other malignancies given the ongoing research dedicated to new treatment options. However, there is limited data in the literature regarding use of radioembolization for unresectable metastatic liver disease. The abstract reviewed here demonstrates a survival benefit with the use of Y90 radioembolization in patients with unresectable metastatic NETs to the liver. This current study has several limitations. The main limitation in this study is in that it was designed as a retrospective study with a small sample size. It would be beneficial if the study was a prospective trial with a larger cohort. Also, the study did not include a comparison to patients who did not receive Y90. Direct comparison would have provided a means to evaluate statistically significant differences of survival time between the two groups. Additionally, the study was conducted at a single institution which limits the variability of the patient population. However, despite these limitations, one can infer from this abstract that radioembolization does provide some benefit in survival for patients with unresectable metastatic NETs in the liver, especially carcinoid tumors.
The data revealed here is similar to other studies in the literature in regards to demonstrating a survival benefit of Y90 radioembolization. There have been numerous small nonrandomized retrospective trials showing varying survival benefit [4]. Eriksson et al. designed a retrospective study of 41 patients with unresectable metastatic liver disease from NET with median survival of 80 months for carcinoid tumor compared to 20 months for pNET [5]. Another retrospective study by Gupta et al. with 125 patients showed an overall survival time of 33.8 months for carcinoid compared to 23.2 months for pNET [6]. There has been one prospective trial with a total of 9 patients with unresectable liver disease that underwent Y90 with 100% survival rate at 1 year and 57% at 3 years [7]. It is a challenge to truly delineate tumor response to radioembolization given the many prognostic variables. Treatment response depends on several factors including the type of NET, tumor burden, grade of tumor, and history of previous treatments [8]. One retrospective study by Shaheen et al. assessed predictors of response to Y90 radioembolization. It was found that previous surgical therapy was a predictor of response and high tumor burden with large metastatic lesions were inversely related to response [8].
Further studies are required to not only assess survival benefit but also to determine the specific patient population that would most benefit from radioembolization. Expanding research in this area could have a major impact on the management of unresectable metastatic NET of the liver.
The authors have no potential conflicts of interest.