- (2006) Volume 7, Issue 1
Ajith K Siriwardena
Hepatobiliary Surgical Unit, Manchester Royal Infirmary. Manchester, United Kingdom
Catheter Ablation; Pancreas; Pancreatic Neoplasms; Surgery /instrumentation
RFA: radiofrequency ablation
Radiofrequency ablation (RFA) for locally advanced cancer of the pancreas appears an attractive proposition. Many Hepatobiliary Surgical Units currently have the equipment and technical expertise for ablation of nonresectable liver tumours and as RFA becomes established in this setting [1], so the concept of thermal ablation for non-resectable tumours is increasingly an accepted component of hepatobiliary practice.
In any given cohort of patients with pancreatic cancer, only a minority are suitable for surgical resection [2, 3]. These individuals with operable disease should undergo surgical resection. An appreciable proportion will be unsuitable for any form of surgical therapy either because of co-morbidity or extent of disease but a small subset will have locally advanced, unresectable cancer without evidence of major co-morbidity or metastatic disease. It is this cohort for whom there is a consideration for the use of RFA.
However, there are critical differences between the role of RFA in non-resectable lesions of the liver and a parallel application in pancreatic cancer. These can be considered in three categories: anatomical considerations, factors relating to the tumour biology of pancreas cancer and those relating to the physical properties of pancreatic parenchyma. First, anatomical considerations: liver tumours are surrounded by areas of normal hepatic parenchyma and extension of the zone of ablation beyond the tumour will usually not have adverse consequences. In contrast, lesions in the head of the pancreas will be traversed by the distal common bile duct and be closely related to the duodenum, stomach, transverse colon and portal vein - the risks of inadvertent thermal injury are considerable and made more dangerous when understood in the context of an un-resectable tumour. In this setting, inadvertent thermal necrosis of the duodenum cannot then be retrieved by resection. The second group of considerations relate to tumour biology: hepatic metastases are usually discrete lesions whereas locally advanced pancreatic cancer can be physically diffuse and encase the superior mesenteric artery, extend retroperitoneally or proximally rendering direct ablation of all tumour bulk impractical. The third group of considerations relate to the efficacy of thermal ablation of pancreatic parenchyma. Given the dearth of available information in this area, our group established and validated an ex-vivo porcine model of radiofrequency ablation of the pancreas [4]. In this model, we were able to demonstrate a reproducible, temperaturedependent ablation. As haematoxylin and eosin preparations are inadequate for assessment of ablation, we used the method described by Scudamore [5] relying on loss of tissue oxidative enzyme activity as measured by depletion in nicotinamide adenine dinucleotide (NADH) after thermal destruction. Computerised digital image reconstruction techniques confirmed that precise ablation was technically feasible [4]. Extension of the model by the use of a modified cardiac bypass pump device connected to the superior mesenteric/portal vein confirmed the heat-sink effect of thermal conduction [6]. Thermal injury to the intrapancreatic common bile duct was a corollary of ablation of lesions in the head of the pancreas.
The technique was then adapted for use in the clinical situation [7]. In the first instance, surgical ablation by laparotomy was selected. After careful consideration, ethics committee approval was sought to use this procedure only in those patients undergoing trial dissection for pancreaticoduodenectomy and who had been found to have unresectable disease at surgery (usually because of locally advanced disease). Thus, no patient was subjected to laparotomy simply for ablation. In the surgical technique, the duodenum was kocherised and the gastrocolic omentum divided. These steps allowed bi-manual control of the head of the pancreas and effectively isolated it from the stomach, colon and inferior vena cava. RFA was then delivered to the tumour, usually with multiple passes of the probe. It was accepted that the intra-pancreatic distal common bile duct would be likely to be injured by ablation and to circumvent the effects of this a Roux hepaticojejunostomy was performed (as a standard biliary bypass in inoperable cancer) after transecting the common duct and ligating the distal end. In practice, vascular inflow control was unfeasible - large adherent tumours prevented easy access to the splenic vein and considerable additional dissection would have been required to sling the infrapancreatic superior mesenteric vein. Thus the heat-sink effect was accepted. This technique was carried out in two patients. There were no immediate technical complications. One patient developed transient post-operative diabetes insipidus. The relation between ablation and this complication was not conclusively established. Although both patients showed objective evidence of tumour ablation, they are both now dead of disseminated malignancy (at 9 and 11 months respectively).
This issue of JOP carries a further report of three cases of inoperable pancreatic cancer treated by radiofrequency ablation [8]. Again, there is no suggestion of any beneficial effect of treatment on survival.
This recent flurry of interest in RFA for pancreas cancer mandates an appraisal of the current position of this technique. It must be emphasised that to date there is a complete absence of any information that suggests that RFA for non-resectable cancer of the pancreas prolongs survival. The significance of this point cannot be over-emphasised: patients with locally advanced, un-resectable cancer are exceptionally vulnerable and clinicians have an absolute obligation to outline the lack of demonstrated survival advantage. Despite this, if the technique is to be contemplated, it is imperative to have a tissue diagnosis of malignancy either preoperatively or during the procedure (otherwise, survival data risk being skewed by RFA in patients with chronic pancreatitis). Operative ablation should only be used in patients undergoing laparotomy for trial dissection as this avoids patients being subjected to operations that would otherwise not be performed. After thermal ablation, it seems prudent to fashion a biliary drainage. It is clear then that at the present time, radiofrequency ablation is not a component of standard evidence-based management algorithms for pancreas cancer. Yet, for the reasons of availability of equipment it is likely that experience will continue to accrue. At present, there is insufficient knowledge of the side effect profile and the technique is at a developmental stage hence randomised trial is premature.
If clinicians wish to use the technique, it seems an ideal opportunity to pool worldwide experience. We have developed a simple proforma (Appendix) for use of radiofrequency ablation of the pancreas that records a minimum amount of clinical detail and information on operative technique and allows for assessment of survival. This proforma is universally available electronically as an appendix to this article and can be e-mailed or faxed to our unit. We will collate information on side-effect profile and survival and report a worldwide “RFA in pancreas cancer” collaborative experience. It remains to be seen whether radiofrequency ablation for locally advanced pancreas cancer is a treatment of any value and at present it must be regarded with extreme caution.
The probes used in the clinical study for evaluation of radiofrequency ablation were a gift from RITA systems Inc., Mountainview, CA, USA (Declaration of potential conflict of interest)
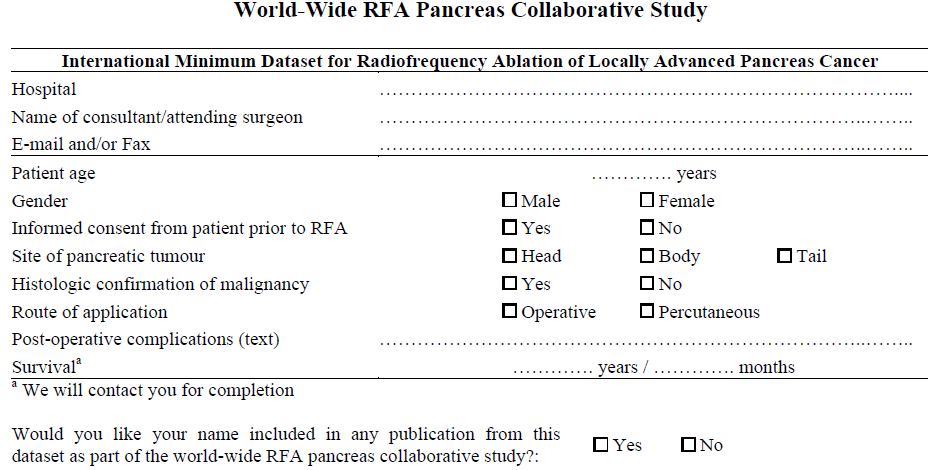
Simply e-mail the completed form to: ajith.siriwardena@cmmc.nhs.uk or fax to: +44-(0)161.276.4530
The Microsoft Word version of this form is available on-line in JOP at www.joplink.net/prev/200601/15_a.doc