- (2006) Volume 7, Issue 1
Giovanni Boz1, Antonino De Paoli1, Roberto Innocente1, Carlo Rossi2, Gian Carlo Tosolini3, Claudio Bassi4, Massimo Falconi4, Paolo Pederzoli4, Mauro G Trovò1
Departments of 1Radiotherapy and 2Surgery, CRO. Aviano (PN), Italy.
3Surgery Department, General Hospital. Pordenone, Italy. 4Surgery Department, Verona University. Verona, Italy
Drug Therapy; Pancreatic Neoplasms; Radiotherapy
AIRO: Italian Association of Oncologic Radiotherapy; cDDP: cis-platinum; EBRT: external beam radiation therapy; ECOG: Eastern Cooperative Oncology Group; EORTC: European Organisation for Research and Treatment of Cancer; ESPAC: European Study Group for Pancreatic Cancer;
Pancreatic cancer is one of the top five causes of cancer death in the Western world and long term survival remains poor with less than 5% of patients alive 5 years after diagnosis [1]. In 1996, the age-adjusted incidence and mortality rates were 12.6 and 12.4 per 100,000 inhabitants for men, and 7.4 and 7.2 per 100,000 inhabitants for women, respectively. The high mortality rate of pancreatic cancer is due to the high incidence of metastatic disease at the time of diagnosis and the lack of adequate systemic therapies. At present, surgery offers the only means of cure. Unfortunately, only 5-25% of patients present with resectable tumors. Patients who undergo radical resection for localized pancreatic cancer have a long-term survival rate of approximately 20% and a median survival time of 11 to 20 months. A much higher percentage (40% to 45%) of patients present with metastatic disease, which carries a shorter median survival of 3 to 6 months [2]. Patients with locally advanced carcinoma of the pancreas constitute an intermediate group. These patients have pancreatic tumors which are defined as surgically unresectable, but have no evidence of distant metastases. A tumor without metastatic disease is considered unresectable if it has one of the following features: extensive peripancreatic lymph node involvement; encasement or occlusion of the superior mesenteric vein or portal vein confluence; direct involvement of the superior mesenteric artery, celiac axis, inferior vena cava or aorta. Combined treatment with radiation and chemotherapy increases median survival for patients with locally advanced cancer of approximately 9 to 13 months, but rarely results in long term survival [2].
The therapeutic options for patients with locally advanced pancreatic cancer include external beam radiation therapy (EBRT) with 5-fluorouracil (5-FU) or gemcitabine (GEM) chemotherapy, intraoperative radiation therapy (IORT) and EBRT with novel chemotherapeutic and targeted agents [3]. Starting from an early randomized trial undertaken at the Mayo Clinic, Rochester, MN, USA in the 1960s, conventional EBRT for locally advanced pancreatic cancer has been shown to improve survival when combined with 5-FU as compared to EBRT alone or chemotherapy alone [4].
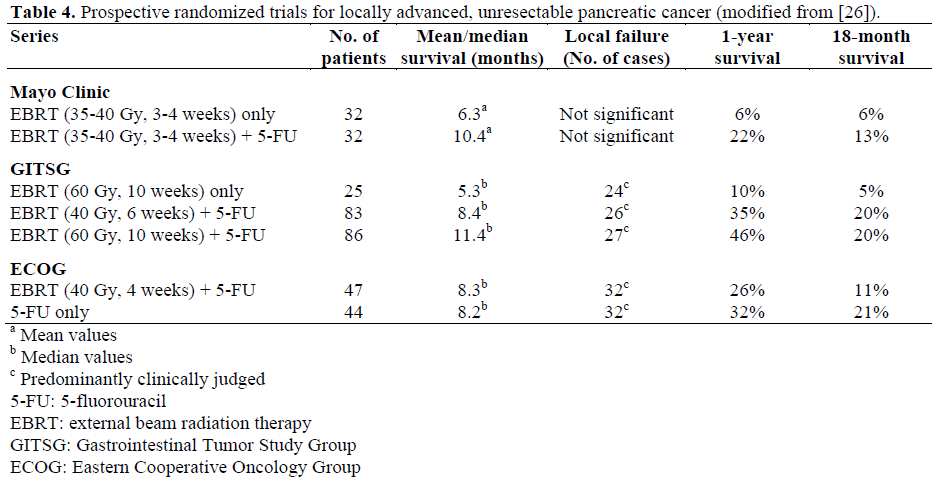
The Gastrointestinal Tumor Study Group (GITSG) followed with a similar study. One hundred and ninety-four eligible patients with locally advanced pancreatic cancer were randomly assigned to receive 60 Gy of splitcourse EBRT alone, 40 Gy of split-course EBRT with bolus 5-FU or 60 Gy split-course EBRT combined with the same 5-FU regimen. The estimated 1-year survival rate in the two combined modality therapy groups was 35% and 46%, respectively, compared with 10% in the EBRT alone group [5, 6].
In contrast to the results of prior studies, the Eastern Cooperative Oncology Group (ECOG) reported no benefit to chemoradiotherapy versus chemotherapy alone [7] (Table 1). Other trials have shown an increased survival rate using more conventional EBRT with modern techniques in the planning and delivery of radiation treatment and continuous 5-FU infusion. Continuous 5-FU infusion allows an increased cumulative drug dose with a greater radiosensitization effect without any significant increase in toxicity. 5-FU was widely investigated and was considered the standard therapy in pancreatic cancer. To improve the clinical outcome of locally advanced pancreatic cancer, GEM was also widely investigated and, since it is a potential radiosensitizer, it may achieve local control when combined with EBRT. To date, only a few studies have compared GEM-based chemoradiotherapy with 5-FU-based chemoradiotherapy and the results seem more favorable for the GEM-based treatment. Based on these results, GEM has become the standard first-line agent in patients with advanced pancreatic cancer. GEM has also been studied in combination with 5-FU and EBRT, although gains in survival benefit are modest. At present, paclitaxel and EBRT were evaluated in phase I and phase II studies. Treatment was well-tolerated and these data provided the basis for further trials [8, 9, 10].

Normal tissues in the upper abdomen (liver, kidney, spinal cord and bowel) have limited tolerance to EBRT. Total doses of 45 to 60 Gy in 1.8 to 2 Gy fractions seem to be inadequate and the local failure rate is as high as 70-80%. Because of poor local control with conventional EBRT and chemotherapy, specialized radiation therapy techniques were studied to improve local tumor control without increasing normal tissue morbidity, such as IORT with electrons or with 125iodineimplants. IORT is a dose-escalation technique in combination with external-beam irradiation and chemotherapy.
To date, in pancreatic cancer, IORT, with doses ranging from 10 to 25 Gy, can achieve a significant increase in local control in resectable disease without any increase in operatory morbidity and mortality. However, there seems to be no benefit in non-resectable disease. The intraoperative radiation study group of the Italian Association of Oncologic Radiotherapy (AIRO), has included IORT as an evidence-based treatment for pancreatic cancer [11].
Despite novel treatment programs, survival benefits for patients with locally advanced pancreatic cancer are still modest almost all patients will die of the disease and their median survival time is rarely greater than 13 months. Despite this, although the palliative benefit of EBRT has not yet been extensively studied, it seems to provide pain relief. Pain is the most common symptom in these patients and using EBRT, with or without chemotherapy, approximately 35% to 65% of patients experience an improvement in pain control.
From 1985 to 1989, 22 patients with unresectable pancreatic cancer entered a study to receive EBRT with chemotherapy. EBRT consisted of 60 Gy in 3 courses (20 Gy each course) delivered over a period of 2 weeks, with a 2-week rest between the courses. Chemotherapy consisted of 5-FU 500 mg/m2 and cis-platinum (cDDP) 20 mg/m2 administered on days 1, 2, and 3 of each EBRT course. After treatment, 12 partial remissions (55%) and 10 no changes (45%) were reported. At the start of treatment, abdominal pain was the most important symptom in 17 patients (77%); after treatment, improvement of abdominal pain was observed in 10 of these patients (59%) and lasted for a median of 5 months. Median survival time was 7.5 months, and median time to progression was 6.2 months. In 2 cases (9%), persistent hematological toxicity did not allow completion of therapy and, in another 3 cases (14%), grade II hematological toxicity required a 2-week rest period in the normal split-course program. In another 4 cases (18%), grade I hematological toxicity did not require any delay in the therapy program. No toxicity was observed in the remaining 13 patients (59%). In this experience, the combination of EBRT plus 5- FU and cis-platinum does not seem to offer any advantage over EBRT and 5-FU alone [12].
To further investigate EBRT and 5-FU interactions, Rich et al. [13] treated a variety of gastrointestinal tumors, including pancreatic cancer, with protracted 5-FU infusion given with EBRT, and demonstrated the feasibility and a possible advantage of concurrent EBRT and 5-FU protracted infusion for operable and locally advanced pancreatic cancer. On the basis of the results of previous trials, we started a study of concurrent EBRT and protracted continuous 5-FU infusion. Forty-two patients with locally advanced pancreatic cancer were enrolled in a prospective clinical trial. Using a four-field technique, EBRT was administered at a total dose of 54.0-59.4 Gy in 30-33 fractions. 5-FU was given through a central venous catheter at a dose of 300 mg/m2 day throughout the entire course of EBRT. All patients completed the EBRT as planned and 33 (79%) completed the chemotherapy program. Ten patients (24%) had a partial response and 32 (76%) had stable disease. Out of the 32 patients with stable disease, two (6%) had a subjective complete response and 24 (75%) had partial remission of symptoms. The median time to progression was 6.2 months and the median survival time was 9.1 months. The results of our study compare well with other studies of EBRT and 5-FU. The palliation of symptoms achieved in our experience may be regarded as a positive result [14].
GEM and 5-FU are active systemic agents in human pancreatic cancer and both are potent radiation sensitizers. Preclinical and clinical studies have confirmed the radiation sensitizing activity of low-dose GEM. Other data indicate that the twice-weekly GEM schedule may result in increased sensitization compared with the once-weekly schedule. Based upon these observations, we initiated a study to determine the feasibility and effectiveness of EBRT combined with GEM and continuous 5-FU infusion in locally advanced pancreatic cancer. Twenty-six patients with locally advanced pancreatic cancer were enrolled in the study in 1998. EBRT was delivered using a 4-field technique at a total dose of 54.0-59.4 Gy. GEM was given weekly on Tuesdays and Fridays at a daily dose of 30 mg/m2, and 5-FU was administered in continuous infusion at a daily dose of 200 mg/m2 throughout the entire course of EBRT. If hematological toxicity greater than grade I occurred, GEM administration was stopped and then resumed at hematological recovery. Median survival time was 11 months and median time to progression 8 months. The radiologically confirmed response was: complete remission in 1 patient (4%), partial remission in 7 (27%), and no change in 18 (69%). A hematological toxicity of grade III was reported in 2 patients (8%), grade II in 9 (35%) and grade I in 8 (31%). No toxicity was observed in the remaining 7 patients (27%). Only 5 patients (19%) completed the GEM scheduled treatment. The number of median GEM cycles was 7 (range 4-12 cycles). 5-FU infusion was stopped in 4 patients (15%) because of toxicity. Our experience with twice-weekly GEM, 5-FU and concurrent EBRT may be considered satisfactory in terms of local control and survival. However, 5-FU and GEM administered concurrently with EBRT have a synergistic effect which increases toxicity as compared to more conventional treatments [15] (Table 2).

On the basis of our previous data, in 2000 we started a study to determine the toxicity and efficacy of twice-weekly GEM administered concurrently with EBRT in locally advanced pancreatic cancer. Forty-two patients entered the study to receive EBRT at a dose of 54.0- 59.4 Gy. GEM was given weekly on Tuesdays and Fridays at a daily dose of 40 mg/m2 throughout the entire course of EBRT. If toxicity greater than grade I occurred, GEM administration was stopped and then resumed at hematological recovery. All patients completed the EBRT program whereas the scheduled GEM treatment was completed by only 5 patients (12%). Median survival time was 15 months and disease-free survival was 12 months. The radiologically confirmed response was: partial remission in 16 patients (38%) and no change in 26 (62%). The objective response was complete remission in 1 (2%) patient, partial remission in 21 (50%) and no change in 20 (48%). Hematological toxicity of grade III was observed in 2 patients (5%), grade II in 12 (29%) and grade I in 18 (43%). No toxicity was observed in the remaining 10 patients (24%). Twice-weekly GEM administered concurrently with EBRT is well-tolerated when compared to our previous study with GEM, 5-FU and EBRT. This combination achieves good local control and survival, and is satisfactory when compared to the data from the literature. The control of distant metastatic disease remains an open issue.
With the aim of achieving good local control and increasing the control of distant metastases, we started a study in 2004 using neo-adjuvant chemotherapy with irinotecan (CPT 11) 100 mg/m2 and GEM 1,000 mg/m2 on days 1 and 8 for two cycles followed by EBRT and GEM biweekly. The treatment seems to be feasible in terms of toxicity and there seems to be good control of disease.
The “generally realistic” neo-adjuvant targets are: 1) a higher rate of patients receiving the treatment; 2) no delay in treatment; 3) total time of treatment is reduced; 4) patients with aggressive disease progression will avoid “non-curative” surgery; 5) downstaging with an increased R0 resection rate; 6) peritoneal implantation prevention; 7) fewer side effects of neo vs. adjuvant.
Since surgical resection remains the only potentially curative treatment for pancreatic cancer, preoperative irradiation has been studied to assess its ability to convert locally unresectable pancreatic cancer to resectable disease. Studies from New England Deaconess Hospital (Boston, USA) [16], Duke University (Durham, NC, USA) [16], the Memorial Sloan-Kettering (New York, NY, USA) [16], MD Anderson (Houston, TX, USA) [16], S. Raffaele Hospital (Milan, Italy) [17], and other studies indicate that the currently utilized neo-adjuvant EBRT and chemotherapy can convert unresectable lesions to resectable in only 8-13% of cases. The feasibility of short course preoperative EBRT and chemotherapy, at a dose of 30 Gy in 3 Gy fractions instead of the more conventional 45.0-50.4 Gy in 1.8 fractions, was also evaluated, and the survival curve was similar for the two treatments. With regard to the influence of EBRT and chemotherapy on surgical procedures, it appears that EBRT plus chemotherapy does not significantly increase surgical morbidity or mortality [16] (Table 3). To increase the radiation dose according to tumor volume, IORT can be used in association with EBRT, CT, and surgery. A lower incidence of local failure and improved median survival have been reported in some series. These results support further studies of selected patients with unresectable tumors regarding innovative protocols employing IORT. At present, IORT is recommended by evidence based medicine [11].

In North America, adjuvant EBRT and chemotherapy were adopted as the standard approach in resected pancreatic cancer based on the positive results of a GITSG study (GI9173) [18]. Other evidence support the use of adjuvant EBRT and chemotherapy. In contrast, a European Organisation for Research and Treatment of Cancer (EORTC) randomized study, comparing split-course chemoradiotherapy with observation, found no significant improvement in median survival [19]. The results of the Radiation Therapy Oncology Group (RTOG) are awaited. This study, which has accrued more than 525 patients, has treated all patients with 5-FU-based chemoradiotherapy. In addition, the patients were randomly assigned to receive either GEM or 5-FU. Chemotherapy alone, as an adjuvant treatment, was demonstrated to be effective versus observation alone. The result of the European Study Group for Pancreatic Cancer study (ESPAC-1) has helped to clarify the respective roles of adjuvant chemoradiotherapy and chemotherapy. The ESPAC- 1 is the largest randomized study of adjuvant treatment in resected pancreatic cancer to date [20, 21]. The study was initially designed with a 2x2 factorial design in which patients could be randomly assigned to treatment with chemoradiotherapy, chemotherapy, chemoradiotherapy followed by chemotherapy or chemoradiotherapy followed by observation. The results of the meta-analysis are consistent with the conclusions of the ESPAC-1 study, namely, they indicate that adjuvant chemotherapy significantly benefits patients with resected pancreatic cancer. On the other hand, no benefit from adjuvant chemoradiotherapy could be shown, and indeed, patients who received chemoradiotherapy may even do worse. This study has been criticized because a substantial proportion of patients did not complete the full number of cycles of the treatment protocol and also for the lack of quality control of the EBRT administered. A common feature of the ESPAC-1 and the other chemoradiotherapy studies included in the meta-analysis is the use of split- course EBRT, which is no longer favored by modern radiotherapy practitioners (Table 4). The apparent lack of benefit from chemoradiotherapy may therefore be the result of a treatment which is now considered suboptimal. The potential role of chemoradiotherapy should not be dismissed from further clinical trials. Future studies should, however, at least explore the potential role of adjuvant chemoradiotherapy in certain subgroups of patients, such as those with marginally positive disease, in whom a trend towards benefit was observed in the metaanalysis. Measures which may improve the quality of the data obtained in future studies of adjuvant therapy include more accurate pretreatment staging and pathologic assessment, carefully defined inclusion criteria, and better quality control of treatment administered.
Three-dimensional conformal radiation therapy is integrated into the treatment of a variety of malignancies, including intraabdominal tumors. This CT-based treatment allows coverage of the target volume with reductions in irradiation of non-target tissues compared with conventional techniques. A further refinement of this approach is now obtained by the use of intensity-modulated radiation therapy (IMRT). With this new technology, inverse treatment planning can be performed, permitting computer-based treatment optimization versus a standard planning approach. In fact, a computercontrolled, non-uniform radiation treatment can be delivered to the target, with a more precise and conformal dose pattern and further reduction in normal tissue irradiation. Evolution of these techniques will result in improved treatment tolerance and reduction of late morbidity so that EBRT can be delivered concurrently with chemotherapy with an acceptable level of tolerance [22, 23].
Recent advances in molecular biology have provided a detailed understanding of the molecular events in pancreatic carcinogenesis and may now offer new approaches to the treatment of pancreatic cancer. The development, progression, and metastases of pancreatic cancer are determined by the accumulation of multiple genetic and epigenetic changes, including inactivation of tumor-suppressor genes and activation or overexpression of proto-oncogenes. Molecular defects correlating with tumor growth, resistance, invasion and angiogenesis have been elucidated. When molecular targets are identified, interventions with specific agents might be targeted to improve tumor control. Trials of several biological agents for pancreatic cancer have been carried out. Promising examples of this strategy include inhibition of members of the ErbB family of receptors, ErbB-1 (epidermal growth factor receptor) and ErbB-2 (HER2) with monoclonal antibodies. Cetuximab, a humanized monoclonal antibody for the epidermal growth factor receptor, and transtuzumab, an antibody for HER2, have been combined with gemcitabine in patients with advanced disease. Early results suggest increased activity with these two drugs and a longer period of disease stabilization with cetuximab [24, 25]. The development of these and other novel agents alone and in combination with chemotherapy continues to be a high priority.
Pancreatic cancer will remain a challenging problem well into the 21st century. However, improvement in the early detection, screening, and staging of patients is expected to facilitate progress in the management of this disease. Also, the quality of life should be considered as an end point in the care and protocol design of these patients.
Additional progress in understanding the nature and sequence of molecular events in the development of pancreatic carcinoma will ultimately permit the development of an array of treatments inhibiting specific pathways which mediate the aggressive biology of pancreatic cancer.