Key words
cultural competence, cultural perceptions
and attitudes, diversity, drug and alcohol
misuse, ethnic groups
Introduction
This article reports the findings of a rapid needs
assessment carried out to explore gaps in service
provision, identify training needs for staff and make
recommendations on how to provide services that are
culturally competent in dealing with people from
different cultures and backgrounds. The findings of
this needs assessment informed the development of a
module in cultural competence in dealing with people
with drug and alcohol problems, which is currently
being delivered and evaluated.
Background
Alcohol and drug use amongst minority ethnic groups
has increasingly become a concern for communities
as well as for planners of health, social services and
the criminal justice system (Sangster et al, 2001;
Fountain et al, 2003; National Treatment Agency
(NTA) 2003a,b). The extent of the drug and alcohol
problem within minority ethnic groups is far from
clear. There is an ongoing debate about whether the
low uptake of services by minority ethnic groups
reflects the real need for services, or whether the
high barriers to services prevent people from seeking
help. A number of publications have highlighted the
particular vulnerability of minority ethnic groups to
ABSTRACT
Policy makers and service providers have recognised
the need for culturally sensitive service provision
for people from ethnic minority backgrounds.
This paper reports on the findings of a study
undertaken to inform policy makers and service
providers of the needs of service users from minority
ethnic groups with drug and alcohol problems,
and issues related to access and utilisation of services.
A rapid needs assessment was carried out in
a London borough. One-to-one and focus group
interviews were carried out with service users,
family members, and representatives of voluntary
and statutory service providers. Interviews were
recorded and transcribed for content analysis. The
findings showed differences in access to services by
people from minority ethnic groups, and varying
perceptions of underlying factors and attitudes to
drug and alcohol misuse. The need for culturally
competent services was expressed. The implications
for service provision for a multiculturally diverse
population, and the need for a programme of
education in cultural competence are discussed.
Keywords: cultural competence, cultural perceptions
and attitudes, diversity, drug and alcohol
misuse, ethnic groups developing problems with drug and alcohol use (see,
for example, Westermeyer, 1995; Patel, 1997; Pearson
et al, 1998; Fountain et al, 2003; NTA 2003a,b) and
highlighted the low uptake of services by people from
minority ethnic groups (see, for example, Abdulrahim
et al, 1994; Johnson and Carroll, 1995; Perera, 1998;
Sangster et al, 2001). The reasons were found to be
complex, and included denial and lack of awareness
that there is a problem, stigma within the family and
community, a lack of knowledge about where to go for
help, and a lack of services accessible to clients from
minority ethnic cultures. Healthcare services that had
been planned for the majority population are not
always appropriate to the needs of people from minority
cultures (Smaje, 1995; Sangster et al, 2001; Fountain
et al, 2003). The perception persists that drug treatment
services are run for and by white people (Awaih
et al, 1992; Perera et al, 1998; Sangster et al, 2001). Few
members of staff are members of minority groups, and
consequently there is little empathy and understanding
of culturally based needs or patterns of drug use
(Perera, 1998; Sangster et al, 2001; Fountain et al,
2003). Additional factors that prevented minority ethnic
groups from approaching services included general
mistrust because of the service’s closeness to theHome
Office with its responsibilities for immigration and
policing (Abdulrahim et al, 1994; Sheikh et al, 2001).
Other issues included languages and communication
problems, and worries about possible breaches of confidentiality
(Khan and Ditton, 1999; Fountain et al,
2003).
Disparities in access and treatment are probably not
due to any racial bias among staff but to constraints
such as time pressure and the complexity of the job
(Geiger, 2001). Moreover, while service providers may
be keen to develop their services to include clients
from minority ethnic groups, they may lack the experience,
expertise and clear guidance necessary to make
their service more culturally appropriate to attract
clients from diverse cultural backgrounds (Johnson
and Carroll, 1995; NTA, 2003a,b; Fountain et al, 2003).
People from minority ethnic backgrounds do not
have the same access to appropriate drug education,
treatment and care. Service providers and members of
minority ethnic communities acknowledge that both
cultural competence and specialist knowledge on substance
misuse problems are needed to provide a highquality
service to drug- and alcohol-using individuals
from minority ethnic groups. The need for more and
better quality services for people from minority ethnic
groups has also been recognised in recent government
policies (Department of Health, 1998, 2001; Home
Office, 2000).
Against this background, the Ealing Drug Reference
Group commissioned the Substance Use and Misuse
Team at Thames Valley University to develop training
in cultural competence targeted at professionals from a range of services working with people who have drug
and alcohol problems. As part of this exercise a rapid
needs assessment was carried out in the multicultural
London Borough of Ealing, with the intention of:
• providing an overview of the extent of alcohol and
drug misuse within minority ethnic groups in Ealing
• identifying underlying factors of drug and alcohol
use within these communities
• recognising gaps in service provision
• identifying specific training needs of staff in general
and specialist services.
Methods
The use of a rapid needs assessment as the methodological
tool was chosen for a variety of reasons. A
rapid needs assessment is a methodology that quickly
collects locally relevant data. It is designed to shorten
the time gap between research and the implementation
of intervention strategies, in particular for local
conditions (Needle et al, 2003). Rapid needs assessment
procedures have been shown to be effective as a
pragmatic research tool in examining social, cultural
and economic issues, especially when only limited data
exist (Ball et al, 1998; Rhodes et al, 1999; Needle et al,
2003). This is particularly the case in the context of
drug taking within minority ethnic groups, among
whom treatment uptake is low, and drug use remains
hidden because of its illicit nature and the stigma
within the community. Rapid needs assessment procedures
are preferable to conventional researchmethods
as they enable the delivery of a quick response to
inform policy or decision making in time (Manderson
et al, 1992; Needle et al, 2003). This is of particular
relevance in the constantly changing field of substance
misuse. As rapid needs assessments are undertaken
with the aim of developing interventions and not
merely to generate knowledge, they can be perceived
as an integral part of the response and development
process of an intervention (Rhodes et al, 1999). Rapid
needs assessments have also evolved as a tool for
community development (Manderson et al, 1992;
Needle et al, 2003). Interventions developed in response
to an assessment not only depend on knowledge
of the local situations and practices, but also
require the active participation of the targeted local
communities for whom these interventions are intended,
in the assessment and the design of interventions.
The development of a bottom-up community
response rather than an outside-expert view is likely
to increase the community’s adherence and commitment
to change, to encourage participation and collaboration
and eventually to enhance the success of the
intervention.
Although rapid needs assessment procedures may
have their limitations regarding the depth, quality and
quantity of data which longer-termneeds assessments
can deliver, they offer a quick way of obtaining an
initial snapshot. It was therefore chosen as the appropriate
tool for the purpose of this research and to
inform the development of a training pack and module.
The rapid needs assessment was carried out between
July and September 2001. The review of the literature
drew on a variety of sources including electronic databases,
such as Medline and PubMed,Home Office and
Department of Health websites, government guidelines
and reports. Further database and library research
included the libraries of DrugScope, King’s Fund and
Thames Valley University, where unpublished literature
on examples of good practice was found and
included. The literature review informed the background
of the rapid needs assessment and guided the
design of the questionnaire and the data analysis.
Data collection included documentary analysis of
the annual attendance data in selected treatment centres,
and demographic statistics from the local borough of
Ealing. Of the four Ealing treatment centres, two were
alcohol services and two catered for drug users. Treatment
uptake data were also selected from an alcohol
treatment centre in the neighbouring borough of
Hammersmith, to compare uptake by different ethnic
groups.
Ethics committee approval was not sought. A multidisciplinary
and multicultural steering group guided
the study. This group included representatives from
the local drug reference group, who commissioned the
research, as well as local service providers. The drug
reference group consisted of local professionals from
health, social and specialist drug and alcohol services,
schools, youth, homeless, the criminal justice system
and community services, and from the statutory and
non-statutory sectors. Its members recommended individuals
and services as key informants for interviews
from a broad range of settings, that included health,
social, educational and community areas. The criteria
for inclusion were that the participants needed to be
well informed and knowledgeable about the specific
area of the focus of the study. For example, service
providers who were directly involved in a caseload of
patients with drug and alcohol problems were invited
to participate. The recommended individuals or services
were approached. They were informed about the
aims and outline of the study. They were asked about
their willingness to take part and their availability.
Frequently, those initially approached recommended
other individuals or services for inclusion. Those approached
expressed a genuine interest in the study.
However, two declined to take part for reasons of time
constraints. The distribution of the key informants
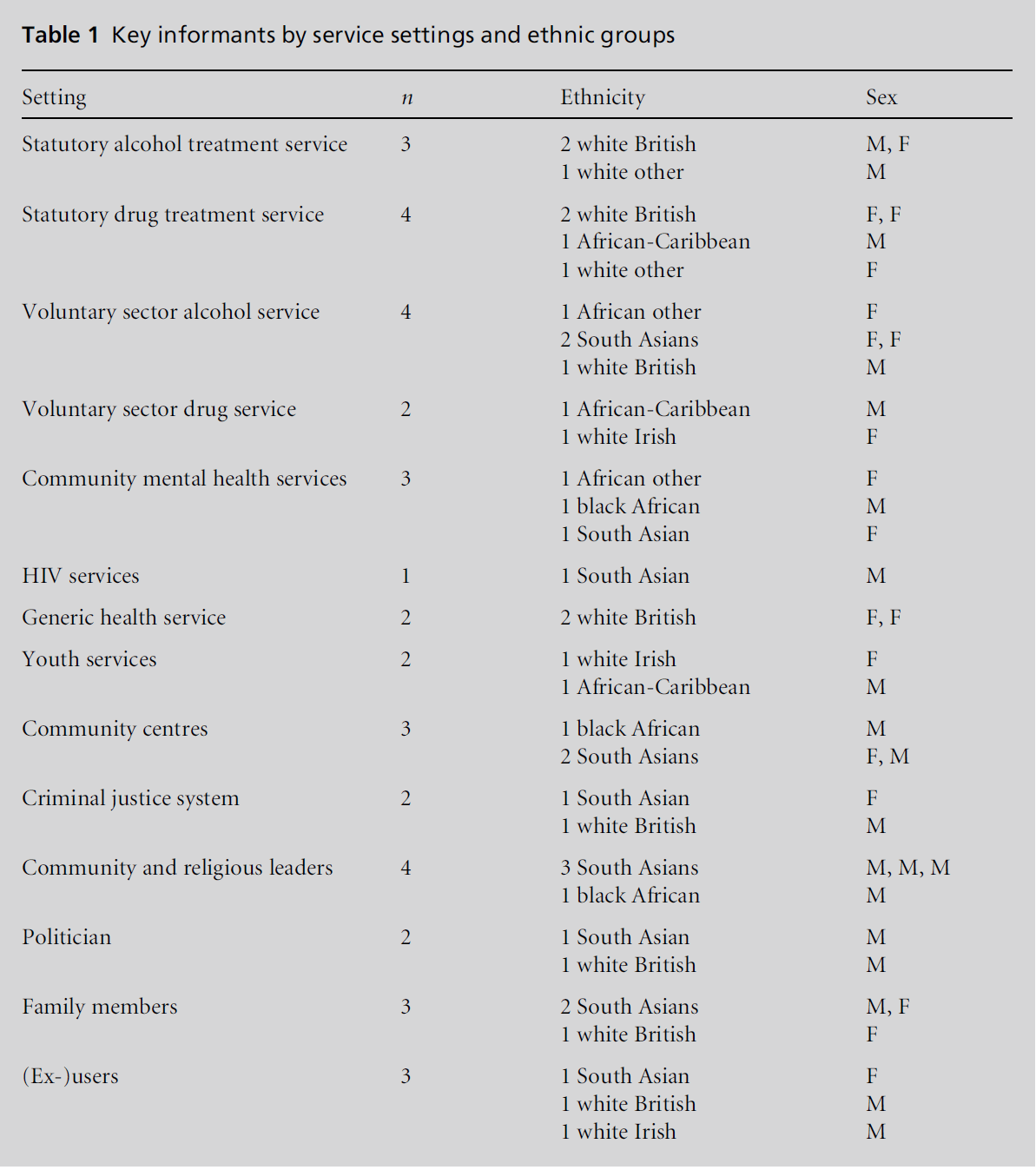
was mixed in terms of their sex, age and ethnicity (see Table 1).
Thirty-eight semi-structured one-to-one interviews
were conductedwith key informants within the borough
(see Table 1). In addition, a focus group was conducted
with parents (n = 12) of drug-using young people
in Ealing. The focus group consisted of a mix of
ethnicities, genders and ages: five were females, seven
were males, ten came from minority ethnic background,
two were white British. The age range was
40–60 years. Interview and focus group data were
recorded as written notes on paper rather than being
tape recorded. As a substantial number of participants,
particularly from minority ethnic groups, had
expressed their wish not to be tape recorded, we adapted
this approach to all interviews. Notes were taken in
each interview and anonymised using a coding system,
as were the notes from the focus group. In order to
ensure confidentiality of data, only the researchers had
access to the personal details of the participants.
An interview frame was developed from an understanding
of the issues raised in the literature, from
policy guidelines and unobtrusive observation in shops
and parks in the borough. The interview frame and key
questions were discussed and approved by the steering
group. Questions focused on participants’ perceptions
and possible explanation of what were the underlying
factors within the cultural context of drug and alcohol
use within minority ethnic groups, and how this would
impact on help-seeking behaviour. Participants were
also asked what they thought of the current practice in
services, if they identified any gaps, and what makes a
service culturally competent.
Data analysis consisted of a constant comparison
analysis of interview notes from both the one-to-one
interviews and focus group (Strauss and Corbin, 1998).
Content analysis of the interview notes and the notes
from experimental field work (observation where people
from the local community were met and geographical
factors were explored in shopping centres, public parks,
local off licences and local shops) was carried out. The
one-to-one interview data were read. Key themes and
patterns were identified by coding and segmenting the
data. Initial codes were attached to words, phrases and
sentences. Similarly coded responses in interview notes
of each case were given a corresponding number.
Similar codes assisted in generating categories through
comparison of data from each case. A reiterative process
was utilised in deriving categories to ensure that these
were in synchrony with the questions asked, and to
transform data into meaningful concepts (Richards,
2005). Categories were collated into particular concepts
or ideas explored. Concepts were scrutinised to
identify their relationships with each other.
Analysis of the focus group data adopted the same
processes of coding words, phrases and sentences, and
deriving of categories. These were then collated into
concepts. The findings are presented in statements
with actual data as quotes from interview notes.
Table 1: Key informants by service settings and ethnic groups
Findings
Demographic and treatment uptake
data
Multicultural Ealing
Analysis of the demography of the London Borough of
Ealing showed that it is a highly multicultural area
with a large minority ethnic population (41.3% of the
total population – 9.1% in England and Wales). It also
has a high proportion of young people; 19.8% of Ealing’s
population is under the age of 16 years (census data 2001; Neighbourhood statistics, 2001). According to
census figures the largest minority ethnic group in
Ealing is of Asian origin (24.6%), of which the Indian
population is the largest group (16.5%) with other
Asian 3.9%, Pakistani 3.8% and Bangladeshi 0.4%
forming the remainder of the Asian population. People
of black origin form the next largest group (8.8%), of
which Caribbean people form the largest proportion
(4.5%). Africans 3.7% and other black people 0.6%
make up the remainder of the black population (London
Borough of Ealing, 2001). The Irish population is the
only white ethnic minority category listed in the
census. Irish people form 4.8% of the minority ethnic population in Ealing.According to theOfficeof National
Statistics Mid-Year Estimate (2000), the minority ethnic
population in Ealing is increasing, particularly in
those areas with an already high proportion of minority
ethnic groups. Black Africans and other ethnic
communities are those groups with the most rapid
growth.
These demographic data illustrate the diversity of
Ealing’s minority ethnic communities, which is expressed
in a range of lifestyles, religions, cultural norms
and values. This diversity is also shown in a range of
views on the use of substances, knowledge of treatment
services and expectations upon these services.
Given the predominant South Asian population in
this borough, what is reported here isweighted heavily
towards a South Asian perspective.
Treatment uptake
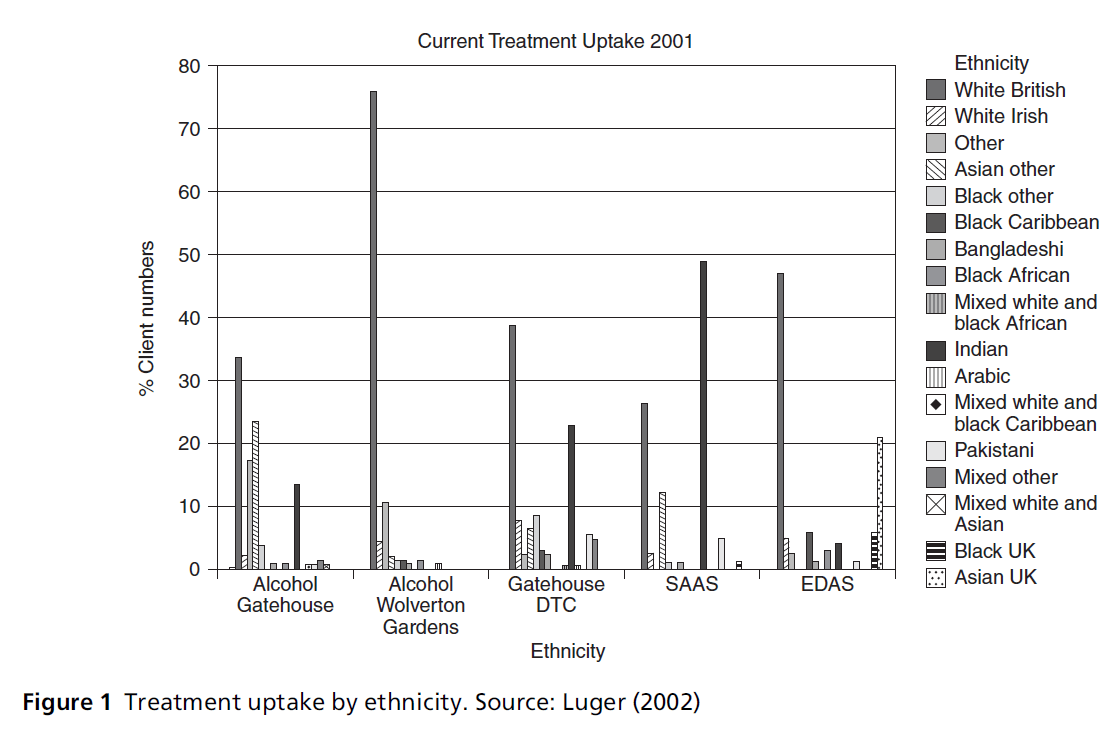
Review of the treatment uptake data of five participating
statutory and non-statutory treatment providers
revealed that people from minority ethnic groups
are approaching drug and alcohol services for help,
but to a lesser degree than the indigenous white British
population. The treatment uptake data (see Figure 1)
reflect the ethnicity profile of the borough. The highest
proportion of clientswithin most of the services under
study was ‘white British’, followed by either ‘white
Irish’ (Alcohol Gatehouse 16.8%), ‘Indian’ (23.2%
Gatehouse Drug Treatment Centre (DTC) and 49%
Southall Alcohol Advisory Service (SAAS)), or ‘Asian
UK’ (21% Ealing Drug and Alcohol Service (EDAS)).
Compared to data from a treatment centre in the
neighbouring borough of Hammersmith, an area with
apredominantlywhite British population, the treatment uptake clearly shows a reflection of the ethnicity
profile (The Wolverton Gardens Centre: 75.8% ‘white
British’, 10.9% ‘white Irish’ and 4.7% ‘white others’
followed by 2.3% ‘others’). Local treatment data also
indicated differences in the uptake of services with
regard to sex and age. Drug treatment services have
been taken up to a higher extent by young white
British individuals, and declined with age (under 20
years 68%, 20–29 years 58%, 30–39 years 50%). The
reverse is true for minority ethnic groups who accessed
services at an older age group (40–49 years 57%, 50–59
years 70%, 60+ years 78%). Analysis of the sex distribution
showed a higher proportion of white British
females in all services, for example, 62% white British,
followed by 8% white other, 8% Indian, 6% mixed
other at the Gatehouse DTC.
Treatment uptake data show that members of
minority ethnic groups use some services more than
others. The findings indicate that those services with a
cultural mix of staff were more likely to be visited by
minority ethnic groups than those with only white
members of staff. However, the data on the uptake of
treatment do not give information about client satisfaction
or the quality and success of interventions, nor
do they indicate whether these services met the needs
of their clients.
Findings from the one-to-one
interviews with key informants
Underlying factors
Figure 1 :Treatment uptake by ethnicity. Source: Luger (2002)
When asked about what factors they thought influenced
substance use, 90% of participants thought that the clash between traditional and western culture had
a huge impact as to why people drank and took drugs.
It was suggested that while first-generation immigrants
might use drugs and alcohol to overcome their
isolation and anxiety because they lived in a foreign
society, young Asian or black people born in Britain
tend to drink or use drugs to fitwith their white British
peers from school or work. The issues are complex but
it was simply stated thus:
‘Being South Asian in Britain – everything changes.’
(South Asian community drug worker and mother)
Furthermore, the stigma of drug use, shame and guilt,
and the pressure of keeping up appearances within the
community were found to have a huge impact on their
ability to seek professional help. For example, one
respondent suggested that:
‘If you have a good reputation as a hard working man/
woman, who goes to the temple and your family is OK,
you have obviously done well, then society treats you
well.’ (South-Asian community alcohol worker)
Respondents also believed that it is often difficult to
live up to the public image, especially when the traditional
values and beliefs disintegrate with the increasing
influence of western culture.
‘It’s a shame when your husband is drinking or if the son is
taking drugs. It’s your fault. Blame yourself!!’ (South
Asian community worker and mother)
Private behaviour, be it extramarital affairs, drinking
alcohol and taking drugs or domestic violence, was
accepted by the family, as long as no one outside the
family got to know about it. In the event of private
behaviour becoming public, the family was overcome
by shame and guilt. As a result drug and alcohol
problems tended to remain behind closed doors.
The overwhelming majority of respondents (90%)
reported that a variety of issues were found to be vital
in a family’s perceptions of alcohol and drug use, and
their knowledge and attitude to treatment. These included
lifestyle, family structure, religion and socioeconomic
background, approaches to solving problems
and giving support within the family and community.
While it was believed that Islam, Sikhism and Hinduism
prohibit the consumption of alcohol, it was thought
culturally acceptable for male Sikhs and Hindus to
drink. Male behaviour was associated with drinking:
‘Sikh and Hindu bring about macho masculine behaviour.
Drink alcohol to progress to being a man, a masculine
man!’ (Male South Asian sexual health worker)
A belief commonly held by participants (about 60%)
was that adherence to religious and cultural taboos
was slowly being eroded.One example given suggested
that young South Asian women did not seem to care
about the old taboos but wanted to go out and enjoy
life just like their white British friends did. Nevertheless, views were expressed that the influence of religion and
culture is still very strong and that its impact on the
individual should not be underestimated. Breaking
taboos and violating the rules and social conventions
of one’s community was still perceived as a source of
considerable guilt and shame.
Ten percent of the respondents made reference to
the role of religious or community leaders in the
context of drug and alcohol taking. They felt that
while some understand the problems their community
members are facing, others ignored the existence
of drugs and alcohol:
‘They don’t even want to have leaflets about drugs in the
temple.’ (South Asian drugs worker)
Community leaders were seen as protecting or defending
their community and not admitting to the existence
of drug and alcohol problems.
‘Community leaders are often defending their race and do
not admit that there are drugs and alcohol problems. But
they need to see the reality of their people.’ (South Asian
drugs worker)
Participants reported that ignorance of the problem,
and lack of knowledge concerning what to do and
where to go, were reasons for not accessing services.
Families with a drug user often took drastic measures
such as locking the drug user into the bedroomto keep
him/her away from the bad influence of friends. The
family might act in good faith, hoping that the person
will get better, without being aware of the dangers and
effects of withdrawal without appropriate medical
treatment and supervision.
Another measure was to send the drug user back
home to the subcontinent. Families believed that removing
the person from the environment would help
in changing behaviour.
‘They hope to get them away from western influence,
from drugs and their drug-using friends.’ (South Asian
drug prevention worker)
Professionals from drug treatment centres highlighted
the frequent use of private detoxification units by
South Asian families who believed that detoxification
would solve the drug problem.
‘Families try to get their kids in private detox. They pay up
to £3000 per week and think everything is fine afterwards.
But things don’t go like this. As soon as the kid is back,
he gets addicted again.’ (South Asian drug worker in
statutory service)
Current practice in services
In order to highlight current practice in services, the
participants were asked what they saw to be the key
challenges for the provision of services for clients from
different ethnic groups. Seventy per cent of staff from a
white British background admitted that they often felt uncomfortable because they were aware that their
white clients and those from minority ethnic backgrounds
had different needs.
‘I am comfortable talking about drug issues with someone
from a minority ethnic group, but when it comes to
cultural issues then I feel I am sort of stuck, because I do
not know exactly what it is that they need.’ (White drug
worker)
However, many white drug and alcohol workers said
they were not able to identify exactly what these needs
were. Service staff reported feeling comfortable talking
about drug issues with someone from another ethnic
group, but did not feel competent in relating to the
cultural issues of their clients. Twenty per cent of staff
stated that they treated all people equally, regardless of
their cultural background. Only about 10% of staff
stated that they felt comfortable in dealing with clients
from all other cultures. These staff mainly came from
a minority ethnic background themselves and were,
therefore, socialised into a multicultural environment.
Staff and community members identified a number
of issues that needed to be addressed when providing a
service for clients from different cultural backgrounds.
In their view, staff needed a knowledge base about
other cultures that included knowing how to pronounce
names, the meaning of titles, dietary requests,
lifestyles, religious rules and dress code. People from
minority ethnic cultures might be reluctant to access
what they perceived as ‘white’ services. Possible reasons
for this were not feeling respected and understood,
and maybe mistrust of service providers from other
cultural backgrounds. White staff who were unaware
of cultural differences might fail to recognise their
needs. Clients were more likely to approach a service
when someone from a minority culture was working
there. Even if clients chose not to consult someone from
their own culture, a mixed cultured service would
demonstrate more openness.
Gender differences in treatment uptake were explained
with reference to cultural norms and restrictions.
Societal stigma often made it difficult for women
to admit an alcohol or drug problem. Respondents
from the minority ethnic communities highlighted
that women might be prohibited from leaving their
homes without a male companion, or might be uncomfortable
accessing mixed-gender services. It was,
therefore, suggested that service providers needed to
ensure that their serviceswere confidential and safe for
women.
Language-related problems formed one of the overriding
concerns about service provision to minority
ethnic clients. Linguistic differences could lead to misunderstandings
or evenmisdiagnosis, and prevent people
from accessing services. While most young Britishborn
individuals were fluent in the English language,
first-generation immigrants, especially females, might not be able to converse effectively with staff in services.
Language was not the only issue here. Poor communication
between services and communities was likely to
lead to mistrust in services.
What makes a service culturally
competent?
Participants were asked what they believed made a
service culturally competent. A number of issues were
raised, including awareness of the cultural mix of the
potential client group, the implementation of race
equality policies and non-discriminatory practices.
The concept of a culturally competent service should
become the norm for working with all clients. A
cultural needs assessment should be conducted in
order to tailor the service to an individual’s particular
needs. A cultural mix of staff would signal that services
were more accessible and open to the needs of minority
ethnic groups.
Most participants felt it was important that services
made contact with the communities they worked for,
through outreach work in the community and the
training of peer educators. Further suggestions included
more key workers, frontline staff from minority
ethnic groups, and partnerships between services
and the community.
A number of training needs were identified in
relation to knowledge and understanding of the
underlying factors of drug and alcohol use within
different cultures. Skills were needed to enable staff
to identify and meet the needs of drug and alcohol
problemusers from these population groups and their
families.
There was a common view that the development of
culturally competent services is not just an educational
issue. Education must go hand in hand with
a range of structural adjustments and government
policies that support the development of culturally
competent organisations and services. Examples given
included:
• increasing funding for drug and alcohol treatment
to decrease waiting times and to increase the
capabilities of staff to reach out to hidden populations
in need of services
• creating opportunities for clients to choose white-,
mixed-culture- or ethnic-specific services
• ensuring that culturally specific services did not
become isolated ghetto services, vulnerable to marginalisation
and closure in time of resource constraints.
Findings of the focus group with
parents of drug users
The participants in the focus group estimated that
approximately 30–40% of the families in Ealing of all ethnicities were facing problems with their offspring’s
drug use. Yet, they stated that there were few local
services that young drug users and their parents could
access. Those that existed were not open in the evenings
when working parents were able to attend. In the
opinion of the parents, the waiting time for accessing
drug treatment was too long. The limited number of
rehabilitation centres, and the time between detoxification
and rehabilitation was also too long to be
effective. Some families reported trying detoxification
at home, but were not given any advice on how to deal
with withdrawal symptoms. It was commonly felt that
the staff in services did not understand young people’s
needs and the cultural background they were coming
from. In particular, parents from South Asian backgrounds
criticised staff who did not understand the
importance of the role that families play in their culture,
or that the head of the family needed to be involved in
the decisions on treatment issues. These parents admitted
that they found it very hard to be excluded
from the treatment for reasons of confidentiality.
All participants agreed that the treatment needed to
include the parents and their drug-using offspring.
Parents needed help because they did not know what
to do or how to support a drug-using child. They were
often not informed about the impact of drug use and
possible treatment options. They did not understand
and were frequently scared because they felt left alone
with their problem. A significant number of parents
(40%) reported that they had received little understanding
and help from their general practitioner
(GP), while others (30%) felt their GP was very helpful.
Some (20%) admitted they were too ashamed and
frightened to ask their GP for help.
‘I thought that it would never happen to me and that my
kids would never take drugs. I was wrong. I ignored it for
too long because the thought of it was too frightening.’
(South Asian mother of a drug-using son and daughter)
‘Sadly, I had to realise that covering up for my son’s drug
use only worsened the problem.’ (Black Caribbean mother)
All participants in the focus group agreed that the
Families Anonymous Group was very useful to them.
The group had helped them to accept their son’s or
daughter’s drug use and to understand that family
conflicts were important factors in their children’s drug
use. The group helped them to change their different
attitudes and to understand that they couldn’t solve
their children’s problems.
‘Being in the Families Anonymous Group changed my
attitude to my son’s drug taking. I needed to accept that I
can’t solve the problem for him. No matter, if I lecture,
moralise, blame or argue with him, whether he is stoned
or sober, it does not help. It may make mefeel better, but it
makes the situation worse. Losing the temper with my son
will destroy our relationship and any possibility of me
helping him.’ (South Asian father)
‘My wife does not go to the meetings, which is sad. As a
consequence she does not have the same attitude towards
him as I have. She does not understand him and goes on
arguing. But when he is not willing to stop using drugs we
need to consider what we can do to avoid standing in the
way of his recovery.’ (South Asian father of a drug-using
son)
Finally, all participants expressed their great relief at
meeting others with similar experiences and problems.
The group helped them to learn more effective
ways of coping with the situation and, at the same
time, gain some peace of mind and hope for a better
way to live in the future.
Discussion
Comparing the treatment uptake figures was difficult
because the ethnicity categories vary between the
individual treatment centres. For example, only one
service used the category ‘UK Asians’, which referred
to young South Asians born in the UK. Furthermore,
the categories were not detailed enough to detect certain
ethnic groups, such as people from Iran, Poland or
Somalia. This may explain the high number of clients
in the category ‘others’ where clients probably could
not identify themselveswith any of the existing groupings.
The category ‘white others’, for example, embraces
everyone who defines themselves as white. This
may include people from East, West, North or South
Europe, Turkey, Iran, the United States and Australia;
countries whose cultures differ widely from each other.
These findings show that the concept of ethnicity
is very complex, and ethnic categorisation does not
embrace the diversity within ethnic groups. There has
been much debate on the issue of ethnic identity and
the categorising of population groups (Bradby, 1995;
Aspinall, 1998). The usefulness of monitoring ethnicity
and conducting research into ethnicity and equity
in health has been questioned as to whether it is racist,
simplifying complex issues, blaming the victim or a
vital requirement in improving services (Bradby, 1995;
Bhopal, 1997; Kaplan, 2003). Furthermore, the longstanding
association between material deprivation,
minority ethnic status and the experience of racism
means that ethnicity and socio-economic group cannot
be treated as independent variables (Bradby, 2003;
Nazroo, 2003). Therefore, ethnicity on its own does
not seem meaningful, as it does not take into account
factors such as the socio-economic situation that may
impact on the vulnerability of particular population
groups with regard to health problems and their helpseeking
behaviour.
The findings of the study confirmed the complexity
of reasons for low treatment uptake that were highlighted
in the literature review. For example, the low uptake of these services by African or African-Caribbean
people may partly reflect their relatively low proportion
within the local population. It may also reflect
referral procedures based on misdiagnosis, stereotyping
or prejudices in GP practices or primary care
settings, which commonly referred black clients to
mental health units, and may be due to a lack of
understanding of minority ethnic culture by staff in
services (Sangster et al, 2001; Fountain et al, 2003). In
the case of black Africans, particularly Somalis, the low
treatment uptake appears to reflect participants’ perceptions
about the attitudes of service providers, and
results in a lack of trust in services. Again, this confirmed
earlier explanations which suggested that mistrust
may be the result of a number of factors,
including the perception that drug services are for
white people only, experience of discriminating attitude,
little empathy, and lack of understanding by
staff.
The findings also highlighted that a variety of
reasons may either hinder or facilitate access. These
include whether the location of the service is easily
accessible by tube or bus; the proportion of minority
ethnic groups within the local population; the degree
of staff mix in the service; whether the service is also
offered in the languages spoken within the community;
whether it is provided by a voluntary or statutory
treatment organisation; and whether the service is
known to the community or the referring GP. The
stigma attached to drug and alcohol problems may
cause people to access services in other boroughs, in
order to avoid meeting someone from their own
community. In addition, the feeling of guilt and shame
is not easily overcome and may even lead to more drug
and alcohol consumption or prevent the person from
accessing help.
Further findings pointed to the lack of awareness
about drug problems and the lack of knowledge about
what to do and where to go for help (Johnson et al,
1995; Perera, 1998; Sangster et al, 2001; Fountain et al,
2003). The well-meaning practice of South Asian
families sending their drug-using adolescent back
home in the hope that, once there and away from
their peers, they would recover and become drug free
is very often not successful. The young person may
develop a much heavier drug habit, as drugs, particularly
heroin, are purer, cheaper and more easily available
in South Asia than in Southall (Pearson and Patel,
1998). Alternatively, a young person may be drug free
on return to the UK, but may quickly revert back to
their old habits if no aftercare support is offered.
Similarly, the frequent use of private detoxification
units by South Asian families may be of limited success.
Families often underestimate the complexity of
drug dependence. Detoxification is only the first step
of a long hard road to recovery. In order for drug
treatment to work, the drug user needs to be motivated to stop using drugs. In addition, substance use is often
a means of coping with problems in a person’s life.
Unless these problems are addressed, drug treatment
may not be successful.
In summary, the findings of the study supported
many of the key issues highlighted in the literature
review. The findings demonstrated the seriousness of
the problem and the desperate need for support from
drug and alcohol services. Many of the problems
remain hidden because people do not access services
because of shame or guilt, lack of knowledge about
where to go for help, or because they feel the services
are not appropriate for them. On the other hand,
service providers often lack understanding of minority
ethnic cultures and time constraints, and the lack of
resources often makes it difficult for them to provide a
service that is culturally appropriate. There was agreement
among service providers and people from minority
ethnic groups that the education and training of
staff are vital in enabling the development of culturally
competent service provision. However, training alone
does not make a service culturally competent. Improving
the communication between healthcare staff
and clients from a different cultural background is as
important, as is improved networking between services
and communities.
Conclusion
In conclusion, the study showed that increasing the
knowledge and understanding of the underlying factors
of drug and alcohol misuse within minority ethnic
groups, and developing the skills of staff to deal
appropriately with the needs of their clients were vital
for the development of culturally competent services.
In addition, more emphasis needed to be placed on
working in partnership with communities and training
peer educators and key workers from within these
communities.More resources were needed to increase
the capacity of treatment services. Education needs to
go hand in hand with the implementation of recent
government policies that aim to minimise inequalities
and social exclusion, bringing into effect race equality
policies and non-discriminatory practice in all public
authorities, including health, social services, the criminal
justice system, education and employment. It needs
to be recognised that culturally competent services can
only be developed within a mutually symbiotic partnership
between the different cultures, characterised
by openness, trust and mutual respect. An educational
and training programme informed by the findings of
this study was developed and has been delivered. The
effectiveness of the programme is currently being
evaluated.
CONFLICTS OF INTEREST
None.
References
- Abdulrahim DW, White D, Phillips K et al (1994) Ethnicity and Drug Use: towards the design of community interventions. Volume 4: Use of services. AR Unit. London: University of East London.
- Aspinall PJ (1998) Describing the ‘white’ ethnic group and its composition in medical research. Social Sciences and Medicine 47:1797–808.
- Awaih J, Butt S and Dorn N (1992) Race, Gender and Drug Services. ISDD Research Monographs 6. London: ISDD
- Ball A, Rana S and Dehne KL (1998) HIV prevention among injecting drug users: responses in developing and transitional countries. Public Health Research 113(Suppl 1): 170–81.
- Bhopal R (1997) Is research into ethnicity and health racist, unsound or important science? British Medical Journal 314:1751.
- Bradby H (1995) Ethnicity: not a black and white issue. A research note. Sociology of Health and Illness 17:405–17.
- Department of Health (1998) Tackling Drugs to Build a Better Britain. London: HMSO. Department of Health (2000) The NHS Plan. A plan for investment. A plan for reform. The Stationery Office. www.dh.gov.uk/assetRoot/04/05/57/83/04055783.pdf
- Fountain J, Bashford J, Winters M and Patel K (2003) Black and Minority Ethnic Communities in England: a review of the literature on drug use and related service provision. London: National Treatment Agency.
- Geiger HJ (2001) Racial stereotyping and medicine: the need for cultural competence. Canadian Medical Association Journal 164:1699–700.
- Home Office (2000) Race Relations (Amendment) Act 2000. The Stationery Office. www.opsi.gov.uk/acts/acts2000/ 20000034.htm
- Johnson M and Carroll M (1995) Dealing with Diversity: good practice in drug prevention work with racially and culturally diverse communities. Centre for Research in Ethnic Relations, Coventry: University of Warwick, for Home Office Drugs Prevention Initiative.
- Kaplan J (2003) Use of race and ethnicity in biomedical publication. JAMA 289:2709.
- Khan J and Ditton J (1999) Minority Ethnic Drug Use in Glasgow. Part two: special problems experienced and possible gaps in service provision. Glasgow: Glasgow Drugs Prevention Team.
- London Borough of Ealing (2001) Ealing in Figures – Fact sheet 2. London: London Borough of Ealing.
- Luger L (2002) Cultural Competence in Dealing with Drug and Alcohol Problems in Minority Ethnic Groups. Report to Drug Reference Group Ealing. London: Thames Valley University.
- Manderson L and Aaby P (1992) An epidemic in the field? Rapid assessment procedures and health research. Social Science and Medicine 35:839–50.
- National Treatment Agency (NTA) (2003a) Models of Care for the Treatment of Drug Users. Part 2. Full reference report. London:
- National Treatment Agency. National Treatment Agency (NTA) (2003b) Models of Care for Treatment of Adult Drug Misusers. Part 2. London: NHS,
- National Treatment Agency. www.nta.nhs.uk (accessed 25 October 2005).
- Nazroo JY (2003) The structuring of ethnic inequalities in health: economic position, racial discrimination and racism. American Journal of Public Health 93:277–85.
- Needle RH, Trotter RR, Singer Merrill B et al (2003) Rapid assessment of the HIV/AIDS crisis in racial and ethnic minority communities: an approach for timely community interventions. American Journal of Public Health 93(6):970–9.
- Office for National Statistics (2003a) Census April 2001. Office for National Statistics. https://www.statistics.gov. uk/census/default.asp.
- Office for National Statistics (2003b) Neighbourhood Statistics. Office for National Statistics. https://www.neighbourhood. statistics.gov.uk/dissemination/AreaProfile2.do?tab=2.
- Office for National Statistics (2003c) Mid-Year Estimates of the Population. Office for National Statistics. https://www. neighbourhood.statistics.gov.uk/dissemination/AreaProfile2. do?tab=2.
- Patel K (1997) Preliminary Assessment of Services Available for Drug Users from South East Asian Communities. Preston: University of Central Lancashire.
- Pearson G and Patel K (1998) Drugs, deprivation and ethnicity. Outreach among Asian drug users in a northern English city. Journal of Drug Issues 28:199–224.
- Perera J (1998) Assessing the Drugs Information Needs of Asian Parents in North Hertfordshire: a brief report to inform the planning of a drugs education programme. London: Action Research Consultancies.
- Rhodes T, Stimson GV, Fitch CH, Ball A and Renton A (1999) Rapid assessment, injecting drug use, and public health. The Lancet 354:65–8.
- Richards L (2005) Handling Qualitative Data. A practical guide. London: Sage Publications.
- Sangster DS, Shiner M, Patel K and Sheikh N (2001) Delivering Drug Services to Black and Minority Ethnic Communities. DPAS/P16. London: Home Office Drug Prevention and Advisory Service (DPAS).
- Sheikh NF, Fountain J, Bashford J and Patel K (2001) A Review of Current Drug Service Provision for Black and Minority Ethnic Communities in Bedfordshire. Final report to Bedfordshire Drug Action Team. Preston: Centre for Ethnicity and Health, Faculty of Health, University of Central Lancashire.
- Smaje D (1995) Health, ‘Race’ and Ethnicity. Making sense of the evidence. London: King’s Fund Institute.
- Strauss AL and Corbin J (1998) Basics of Qualitative Research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage.
- Westermeyer J (1995) Cultural aspects of substance abuse and alcoholism. Assessment and management. Cultural Psychiatry 18:589–605.