- (2013) Volume 14, Issue 3
Cornelia Then1*, Yun-Chung Nam-Apostolopoulos2, Jochen Seissler1 and Andreas Lechner1
1Diabetes Center, Clinic and Polyclinic IV, “Ludwig-Maximilians” University
2Institute of Pathology, Munich University. Munich, Germany
*Corresponding Author:
Cornelia Then
Medizinische Klinik und Poliklinik IV
University Hospital Munich; Ziemssenstrasse 1
D-80336 Munich; Germany
Phone: +49-89.5160.2111
Fax: +49-89.5160.4405
E-mail: cornelia.then@med.uni-muenchen.de
Received December 6th, 2012 – Accepted January 30th, 2013
Context Non-insulinoma pancreatogenous hypoglycemia is a rare cause of spontaneous hypoglycemia in adults. The idealdiagnostic and therapeutic approach is still controversial, not least because most reported cases lack long-term follow-up. Case report We describe the case of a 58-year-old woman, who was diagnosed with idiopathic non-insulinoma pancreatogenous hypoglycemia in 2001. After resection of 75% of the distal pancreas, she initially experienced no additional hypoglycemic episodes and did not suffer from diabetes mellitus. However, after one month, recurrent hypoglycemia occurred. After resection of the larger part of the remaining pancreatic tissue, the patient suffered from hypoglycemic as well as hyperglycemic episodes. Octreotide and diazoxide were not successful in preventing the hypoglycemic attacks, whereas continuous insulin therapy with an insulin pump helped to stabilize the blood glucose level temporarily. Finally, all remaining pancreatic tissue had to be removed. Conclusion This long-term follow-up of non-insulinoma pancreatogenous hypoglycemia treatment in an adult patient indicates that lateral pancreatectomy may not be sufficient for permanent blood glucose control and emphasizes the need of follow-up data after subtotal pancreatectomy.
Keywords
Hypoglycemia; Insulin-Secreting Cells; Islets of Langerhans; Nesidioblastosis; Pancreas
Abbreviations
NIPH: non-insulinoma pancreatogenous hypoglycemia; SACVS: selective arterial calcium stimulation with hepatic venous sampling
INTRODUCTION
Non-insulinoma pancreatogenous hypoglycemia (NIPH) is an important differential diagnosis to the insulin autoantibody syndrome and the more frequent insulinoma. In infants, NIPH is a well-recognized disorder, mainly caused by mutations of genes encoding subunits of the pancreatic ATP-sensitive potassium channel [1, 2, 3]. The cause of adult NIPH is still unknown and may be related to unidentified genetic changes [4, 5]. The majority of cases is associated with preceding bariatric surgery, suggesting that a reactive process, possibly involving glucagonlike peptide 1-induced islet cell proliferation [6], promotes or unmasks a beta-cell defect leading to its hyperplasia [5, 6, 7, 8, 9, 10]. For example, increased expression of insulin-like growth factor 2, insulin-like growth factor receptor 1 receptor alpha and transforming growth factor beta receptor 3 was found in islets from 36 NIPH patients [5] and in three of five patients with NIPH, islet neogenesis-associated protein, a cytokine expressed in the presence of islet neogenesis in rodents, was abnormally expressed [11]. It is estimated that NIPH causes 0.5 to 5% of cases of organic hyperinsulinemia in adults [4, 12, 13, 14]. The incidence of reported NIPH cases increased during the last years [13], which is possibly due to an updated awareness of this syndrome and an elevated frequency of bariatric surgery.
CASE REPORT
A 47-year-old woman was referred to our hospital in 2001 with recurrent symptoms of hypoglycemia, including loss of consciousness. The hypoglycemic symptoms occurred mainly several hours after eating, but also during fasting and had started in 2000. The previous medical history of the patient was unremarkable; in particular she had not undergone bariatric surgery, was not overweight and did not suffer from neoplastic disease.
The 72-hour fasting test revealed symptomatic hypoglycemia with a blood glucose level of 2.0 mmol/L after a fasting time of 40 hours (reference range: more than 2.22 mmol/L with a simultaneous insulin value less than 108.2 pmol/L). The oral glucose tolerance test provoked hypoglycemia with a blood glucose of 1.39 mmol/L 210 minutes after glucose challenge and a maximum insulin level of 12,350 pmol/L and proinsulin level of 5,724 pmol/L (there is no reference range in our laboratory for proinsulin during the fasting test; the determination of proinsulin was primarily of scientific interest). Endosonography, CT and MRI scan, angiography and octreotide scintigraphy revealed no tumor. Selective arterial calcium stimulation with hepatic venous sampling (SACVS) demonstrated no lateralization of the excessive insulin production. Insulin autoantibodies were negative and sulfonylurea intake was toxicologically excluded. Diazoxide and octreotide were not effective in preventing hypoglycemia. Finally, surgical exploration was performed. Neither careful palpation nor intraoperative ultrasonography revealed any pancreatic mass lesion. Distal pancreatectomy (75%) was carried out. The histological examination displayed islets that were normal in structure, but increased in number and size and with slight variations in nuclear size (Figure 1bc). Immunohistochemical analysis confirmed an increased proportion of insulin secreting beta-cells compared to glucagon secreting cells (Figure 1d) and revealed small groups of insulin secreting cells scattered periductularly, which is in line with a previous notice, that islet cell hyperplasia often occurs admixed with nesidioblastosis [15]. ATPbinding cassette transporter sub-family C member 8, glutamate dehydrogenase 1, potassium inwardlyrectifying channel, subfamily J, member 11 (KCNJ11) and glucokinase mutations were not detectable.
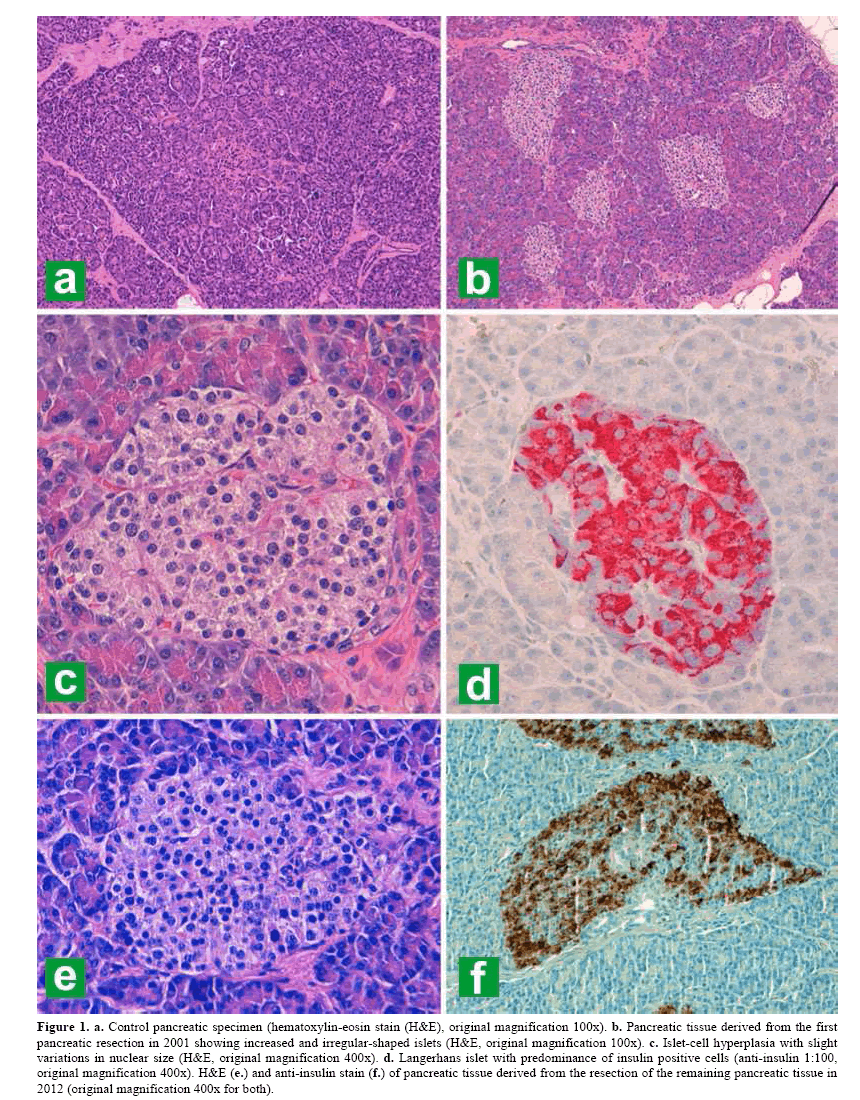
Figure 1. a. Control pancreatic specimen (hematoxylin-eosin stain (H&E), original magnification 100x). b. Pancreatic tissue derived from the first pancreatic resection in 2001 showing increased and irregular-shaped islets (H&E, original magnification 100x). c. Islet-cell hyperplasia with slight variations in nuclear size (H&E, original magnification 400x). d. Langerhans islet with predominance of insulin positive cells (anti-insulin 1:100, original magnification 400x). H&E (e.) and anti-insulin stain (f.) of pancreatic tissue derived from the resection of the remaining pancreatic tissue in 2012 (original magnification 400x for both).
The postoperative course was initially favorable with resolution of hypoglycemia, but was complicated by intra-abdominal abscess formation and recurrent hypoglycemic episodes after one month, which required resection of most of the remaining pancreatic tissue, leaving four centimeters of the pancreatic head in situ. Subsequently, the patient experienced exocrine and endocrine pancreas insufficiency and required insulin therapy. The C-peptide level ranged below 0.99 nmol/L (reference range: 0.9-1.9 nmol/L). However, blood glucose control turned out to be difficult. The patient had plasma glucose peaks of up to 22.2 mmol/L, but also often experienced hypoglycemia several hours after eating. After conventional insulin therapy had been tried unsuccessfully, continuous insulin therapy with an insulin pump was initiated to prevent strong increases of the blood glucose level with subsequent hypoglycemias. The basal insulin requirement was low and variable with a basal rate of two to nine units per day and occasionally elevated postprandial values had to be tolerated. The HbA1c value remained between 31 and 42 mmol/mol (range 29-42 mmol/mol). Nevertheless, recurrent hypoglycemic episodes could not be completely avoided, at times including unconsciousness. In 2006, the C-peptide level began to rise and was 1.98 nmol/L in 2011. The frequency of hypoglycemic episodes slowly increased, resulting in ten to twenty events in 2010 and 2011, respectively. A biopsy from the remaining pancreatic tissue revealed hyperplastic islets, but no sign of progression. A 72- hour fast in 2011 led to a blood sugar value of 2.94 mmol/L, a C-peptide of 0.132 nmol/L (there is no reference range in our laboratory for C-peptide during the fasting test; the determination of C-peptide was primarily of scientific interest) and an insulin level of 45.5 pmol/L after 49 hours. Efforts to readjust the insulin dose remained ineffective and after occurrence of several severe hypoglycemias, resection of the remaining pancreatic tissue was performed in 2012. Similar to the previous operations, the resection was followed by a long and complicated postoperative course. Histological imaging revealed a similar feature compared to the initially resected tissue (Figure 1ef). C-peptide was furthermore not traceable and no more hypoglycemias occurred.
DISCUSSION
NIPH is mainly characterized as postprandial hypoglycemia with sometimes negative 72-hour fasts [6, 11], whereas in some cases, fasting hypoglycemia is an important symptom, making the differentiation against an insulinoma difficult [16]. However, due to the option of localized excision, insulinoma has to be excluded prior to treatment initiation, which often requires extensive diagnostic investigations as illustrated in Figure 2. SACVS is a debatable tool in the diagnosis of NIPH. Adult NIHP is usually pervasive with diffuse beta-cell atypia and islet hyperplasia. Whereas in one third of NIPH cases in infants, focal beta-cell hypertrophy and hyperplasia is observed [17]; this has been documented in only two adults [18, 19]. SACVS proved to be useful in demonstrating hyperactive beta-cell activity and guiding the pancreas resection in two small case series with a good short-term follow-up result in up to 70% of the operated patients [6, 13]. However, other case series found no correlation between preoperative SACVS findings and outcome and often, as in the present case, SACVS demonstrated no insulin secretion gradient [8, 9]. Ultimately, NIPH is a histological diagnosis. Criteria include beta-cell hypertrophy characterized by enlarged, hyperchromatic and pleomorphic beta-cell nuclei, an increased number of normal or enlarged islets in the centre of the lobules and an increased ratio of beta-cells compared to glucagon secreting cells within the islets [12, 4]. As in the present case, the attempt to identify an underlying genetic variation remains mostly unsuccessful [4, 5].
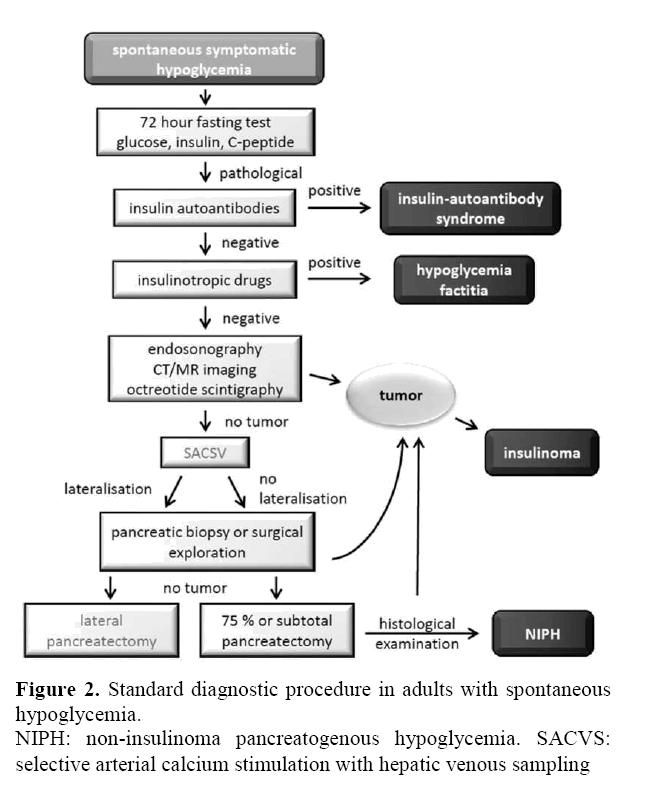
Figure 2. Standard diagnostic procedure in adults with spontaneous hypoglycemia.
NIPH: non-insulinoma pancreatogenous hypoglycemia. SACVS: selective arterial calcium stimulation with hepatic venous sampling
The optimal extent of pancreas resection in adult NIPH is still not firmly established. Distal pancreatectomy (75%) is a successful treatment for some patients and is currently considered as the treatment of choice [3, 6, 11]. However, though partial pancreatic resection often appears to be successful initially, symptoms were recurrent in 87% of patients after a median time of 16 months in a case series of 75 patients with NIPH. During the mean follow-up time of 43 months, the symptoms were mostly less severe than before the operation, but a longer follow-up is required to determine whether symptoms will remain mild or if they progress and become debilitating [9]. Up to 25% of patients had no long-term improvement or even an overall decline in health status after 75% pancreatectomy [9]. Other reports describe a cure of hypoglycemia in only about 50% of altogether 34 patients after 50% to 80% distal pancreatectomy [11, 16, 20, 21, 22]. In contrast, of 12 patients who had undergone subtotal pancreatectomy (more than 90% of the pancreatic tissue), 11 were cured from hypoglycemia, but 75% developed insulin-dependent diabetes mellitus with a high percentage of exocrine pancreas insufficiency [13, 16, 23], whereas after 50 to 80% pancreatectomy, this was the case in less than 10% [6, 11, 16, 20, 21]. Our patient, after 90% pancreatectomy, suffered from both diabetes and hypoglycemia.
Treatment options for patients with recurrent hypoglycemia are limited. The simplest strategy is to eat six small low-carbohydrate meals daily. If this is not sufficient, there are reports on successful treatments with diazoxide or octreotide [9, 11, 23, 24]. However, long-term treatment with diazoxide or octreotide often entails unfavorable side effects and is not always successful, as was the case for the patient described here. Two patients with recurrent hypoglycemia after partial pancreatectomy were successfully treated with verapamil 3 times 80 mg daily [16], an approach that our patient declined. In patients such as in the described case, hyperglycemic episodes may trigger hypoglycemia. A possibility to lessen hyperglycemia is treatment with acarbose, or, if not tolerated or not sufficient, with insulin. In the present case, continuous insulin therapy with an insulin pump was helpful to reduce, but could not permanently avoid, both hyper- and hypoglycemia, so that ultimately resection of the remaining pancreatic tissue was necessary. Since postoperative complications are generally frequent and occur in 30 to 40% of patients [6, 9], re-operation of the remaining pancreatic tissue is often difficult due to adhesions and entails a high risk of anew complications. Therefore, long-term follow-up data after 80-95% pancreatectomy is warranted, and if shown more successful in preventing hypoglycemia in the long term, initial subtotal pancreatectomy might be reconsidered as a treatment of choice.
Conflict of interests
Nothing to declare