Keywords
Renal sympathetic denervation; Hypertension;
Atherosclerosis; Atrial fibrillation; Insulin resistance
Introduction
In 1943, Smithwick reported that lumbar dorsal
sympathectomy decreased blood pressure and reduced longterm
mortality, but clinical application of this procedure was
prevented because of its side effects [1]. The renal
sympathetic nervous system plays a major role in regulating
the entire body and local organ function and includes an
efferent and afferent nerve. The activated afferent nerve of
the kidney activates the central sympathetic nerve and
pathological changes in the structures and functions of organs
emerge due to the excessive activity of the central sympathetic
nerve. In addition, when the efferent nerve is activated, it
changes renal blood flow, affects the reabsorption of sodium
and water in the renal tubular, and causes the release of renin and renal prostaglandin. Eventually, chronic activation of the
sympathetic system causes the development of cardiovascular
diseases through a vicious neuroendocrine cycle. Therefore,
the renal sympathetic nerve influences cardiovascular
diseases.
In 2009, Krum [2], an Australian researcher, was first to
report that they successful control of resistant hypertension by
percutaneous radiofrequency ablation of the renal
sympathetic nerve in the Lancet, and the efficiency and safety
of that procedure were also was proven in that trial. However,
the findings of the Symplicity HTN-3 and a follow-up clinic trial
[3,4], have hindered the application of RDN. Although those
trials denied the efficiency of RDN for the treatment of
resistant hypertension, RDN is safe and inhibits over-activation
of the sympathetic nerve. Our group found that RDN
effectively decreased the blood pressure of spontaneous
hypertensive rats and, especially, inhibited the progression of
left ventricular hypertrophy in a hypertensive beagle model
[5].
Some researchers showed that RDN has a vital influence on
diseases with over-activation of the sympathetic nerve, such
as ventricular hypertrophy, ventricular arrhythmia, atrial
fibrillation, insulin resistance, endothelium dysfunction,
chronic kidney diseases, obstructive sleep apnea and so on.
Therefore, many clinical trials have been performed, and a
great deal of exciting research results will emerge in upcoming
years.
RDN and hypertension
Although the efficiency of RDN for hypertension has been
doubted by some researchers, RDN is a milestone in the
progression of hypertension treatment, and other
investigators are still investigating how to resolve the issues
with the process of RDN. Renal sympathetic nerve activity
plays a crucial role in the pathogenesis of hypertension. In
addition to regulating sympathetic nervous system activity, it
also regulates the renin-angiotensin-aldosterone system
(RAAS). Because of these unique features, inhibiting the renal
sympathetic nerve is likely an effective intervention for
controlling hypertension [6].
Inhibition of the renal sympathetic nerve results in complex
physiological changes and affected by multiple factors.
Therefore, the functional mechanism of RDN is still unclear.
Many investigators are trying to determine the mechanism of
RDN. During the development of RDN, researchers mainly
focused on how RDN affected the SNS; however, many
paradoxical results were obtained. Yoshida [7] and reported
that blocking renal sympathetic nerve does not change the
concentrations of circulating catecholamines. Holmer [8]
showed that renin, angiotensin II and aldosterone levels
significantly declined after renal nerve radiofrequency
ablation; however, Voskuil [9] found that plasma renin activity
did not change after RDN.
In summary, although RDN had been applied to control
resistant hypertension, the functional mechanism of RDN is
unclear; therefore, we cannot fully deny the value of RDN and
discontinue its use based on the findings of Symplicity HTN-3.
More accurate and effective targets should be explored to
illuminate the mechanism of RDN. Additionally, an increasing
numbers of multicenter randomized clinical studies with large
sample sizes are being carrying out to determine the efficiency
of RDN.
RDN and arrhythmia (ventricular tachycardia
(VT), atrial fibrillation)
Sympathetic over-activation directly increases
catecholamine levels, and catecholamine disturbs the
autorhythmicity of myocardial cells and induces trigger action
or reentry in local ventricle, eventually causing arrhythmia. In
addition, catecholamine aggravates ventricular repolarization
by disturbing Ca2+ and Ca2+ transporter levels, which
ultimately induces ventricular arrhythmia [10-12]. Ventricular
arrhythmia is closely related to increased density of the
sympathetic nerves. Cao [13] studied 53 native hearts of
transplant recipients and found that abnormally increased
post-injury sympathetic nerve density may be partially
responsible for the occurrence of ventricular arrhythmia and
sudden cardiac death in these patients. Therefore, inhibiting
sympathetic activity can reduce the occurrence of cardiac
arrhythmias. After RDN was developed, researchers found that
it reduced SNS activity and proved that renal sympathetic
denervation affects heart rate and atrioventricular conduction
[14]. Subsequently, other researchers found that RDN can treat
arrhythmia. Huang [15] reported that RDN reduced the
occurrence of long QT syndrome by inhibiting SNS activity.
Remo [16] used RDN as an adjunctive therapy for refractory VT
in 4 patients with cardiomyopathy and found that the number
of VT episodes was decreased from 11.0 ± 4.2 (5.0-14.0) during
the month before ablation to 0.3 ± 0.1 (0.2-0.4) per month
after ablation. Ukena [17] reported that RDN reduced the
incidence of ventricular tachyarrhythmias in 2 patients with
chronic heart failure (NYHA III) and electrical storm. RDN also
reduced the incidence of secondary ventricular arrhythmia.
RDN effectively and safely reduced the occurrence of VT and
VF in that patients, therefore, the researchers proposed that
RDN may be a new adjunctive interventional bailout treatment
for such highly challenging patients.
Atrial fibrillation is the most common arrhythmia clinically
and is associated with significant morbidity and mortality. The
sympathetic nerve is directly involved in atrial fibrillation as
indicted by its excessive activation during it [18]. Pulmonary
vein isolation (PVI) through radiofrequency ablation or
cryoablation is the most widely used and most effective clinical
treatment for atrial fibrillation [19]. However, atrial fibrillation
had not completely been controlled by this method of local
electrical isolation; 10 -20% patients experience a recurrence
of atrial fibrillation after PVI. With the development of RDN in
recent years, performing RDN in conjunction with PVI can
effectively improve the success rate of PVI and reduce the risk
of recurrence [20]. Pokushalov designed a randomized study to
compare PVI with and without concomitant RDN and enrolled
27 patients with atrial fibrillation and hypertension in 2012.
They found that the atrial fibrillation free rate in the PVI with
RDN group was higher than that in the PVI only group at the
12-month post-ablation follow-up (69% vs 29%, p=0.033) [21].
Another doctor, Vollmann, reported one case of use of RDN
instead of PVI in a 58-year-old female, the patient showed
marked improvement in symptoms and exercise capacity after
RDN.
Several potential antiarrhythmic strategies involving
modulation of the autonomic nervous system, such as
baroreflex stimulation, ganglion ablation, thoracic epidural
anesthesia, low-level vagal nerve stimulation and RDN, have
been explored. RDN had been showed to have a special effect
on arrhythmia. We believe that RDN may be an effective
treatment or adjuvant therapy for atrial fibrillation or other
arrhythmias.
RDN and myocardial remodeling
Neurohumoral activation, for which enhanced activity of the
sympathetic nervous system is a key component, plays a
pivotal role in heart failure. Myocardial remodeling is the key
pathological process of heart failure, and involves changes to
cardiac structure and function in patients with left ventricular
hypertrophy or cardiomyopathy. Renal sympathetic nerve
activity directly or indirectly impacts the structure and
function of the heart. Renal sympathetic afferent nerve
activation activates systemic sympathetic nervous system
activity, and activation of the renal sympathetic efferent nerve
stimulates the release of rennin and increases water sodium
retention and renal vascular resistance. Therefore, inhibiting
the renal sympathetic nerve is also another strategy with
significant value for the treatment of heart failure. Davies et al.
[22] designed a pilot study that evaluated the safety of RDN for
the treatment of heart failure, they researched 7 patients
(mean age 69 years) with chronic systolic heart failure and
found improvements in both symptoms and exercise capacity
following RDN over 6 months of intensive follow-up. The six
minute walk distance was significantly increased at six months
(Δ=27.1 ± 9.7 m, p=0.03). Furthermore, Nozawa [23] reported
that RDN reduces LV filling pressure and improves LV function
after myocardial infraction. Therefore, decreased renal
sympathetic nerve activity may help inhibit the progression of
heart failure after myocardial infraction. Sympathetic
activation has been suggested to contribute to ventricular hypertrophy. McLellan [24] researched the effects of lowered
blood pressure after RDN on structural remodeling in 14
patients, and they found significant reductions in left
ventricular mass (from139 ± 37 g to 120 ± 29 g, P<0.01) and
diffuse ventricular fibrosis (T1 partition coefficient reduced
from 0.39 ± 0.07 to 0.31 ± 0.09, P=0.01) on cardiac magnetic
resonance imaging.
The currently available research findings have proven that
RDN has a significant influence on cardiac structure and
function; however, these findings were obtained by trials with
small sample sizes. Many randomized studies are being
performed to confirm the safety and effectiveness of RDN in
patients with heart failure; maybe more satisfying results will
emerge from those studies.
RDN and endothelium dysfunction
(atherosclerosis, inflammation)
Endothelial dysfunction is the onset of cardiovascular
diseases and is also a predictor of the pathological changes
and the progression of cardiovascular diseases. Excessive
sympathetic activation has a negative influence on the
endothelium. Therefore, it is theoretically possible to inhibit or
delay endothelial damage by reducing sympathetic nerve
excitability. RDN can obviously inhibit SNS and consequently
reduce inflammation. Dörr et al. [25] studied 60 patients (age
67.9 ± 9.6 years) who underwent RDN. They reported that the
serum levels of high-sensitive C-reactive protein (hsCRP)
(p<0.001) and the pro-inflammatory cytokine interleukin-6
(IL-6) (p<0.001) were significantly lower and the levels of
matrix metalloproteinases-9 (MMP-9) (p=0.024) and MMP-2
(p<0.01) were significantly higher after RDN compared to the
baseline values. Wang et al. [26] studied apolipoprotein Edeficient
mice undergoing RDN and found that serum levels of
aldosterone, monocyte chemoattractant protein-1, and 8-
isoprostane were lower in mice that received RDN compared
to sham-operated mice (aldosterone; RDN: 206.8 ± 33.2 versus SO: 405.5 ± 59.4 pg/mL, P<0.05; monocyte chemoattractant
protein-1; RDN: 51.7 ± 7.9 versus SO: 91.71 ± 4.6 pg/mL,
P<0.05; 8-isoprostane; RDN: 331.9 ± 38.2 versus SO: 468.5 ±
42.0 pg/mL, P<0.05). Our research group found that catheterbased
radiofrequency RDN inhibits the renin-angiotensin
system and the oxidative stress response and improved
vascular endothelial function in hypertensive dogs [27]. These
trials confirmed that RDN inhibits excessive activation of the
sympathetic nerve and helps repair endothelial damage.
Therefore, RDN should be examined as a possible new strategy
for improving endothelial function.
RDN and insulin resistance
Chronic over-activity of the sympathetic nerve plays a vital
role in diabetes and insulin resistance is the common feature
of diabetes mellitus (DM) and metabolic syndrome. Insulin
resistance and sympathetic activity have positive feedback
systems. Attenuation of sympathetic nervous system activity
improves insulin sensitivity and we believe that the
development of DM or metabolic syndrome can be slowed down by reducing sympathetic nervous system activity.
Mahfoud et al. [28] enrolled 50 patients undergoing RDN and
found that fasting glucose was reduced from 118 ± 3.4 to 108
± 3.8 mg/dL (P=0.039), insulin levels were reduced from 20.8 ±
3.0 to 9.3 ± 2.5 μIU/mL (P=0.006), and C-peptide levels were
reduced from 5.3 ± 0.6 to 3.0 ± 0.9 ng/mL (P=0.002) after RDN.
In a homeostasis model assessment, insulin resistance
decreased from 6.0 ± 0.9 to 2.4 ± 0.8 (P=0.001) at 3 months
after RDN 118. Witkowski [29] reported that plasma glucose
concentration at 2 hours after glucose administration (median:
7.0 versus 6.4 mmol/L; P=0.05) and hemoglobin A1C level
(median: 6.1% versus 5.6%; P<0.05) were obviously decreased
6 months after RDN in patients with resistant hypertension
and sleep apnea.
The currently available research results have proven that
RDN effectively improves insulin resistance and decreases
plasma glucose concentration in patients with DM or
metabolic syndrome. However, additional large-scale, doubleblind,
multicenter, randomized controlled studies are needed
to further explore the possible relationship between RDN and
insulin resistance.
RDN and chronic kidney dysfunction (CKD)
The sympathetic nerve has a significant influence on kidney
function. Multiple clinical studies have confirmed that patients
with end-stage renal disease exhibit excessive activation of the
SNS and that sympathetic nerve activity is associated with the
progression of renal insufficiency. RDN significantly decreased
the release of neurotransmitters in patients with hypertension
and CKD. Thus, RDN is a potential treatment strategy in
patients with excessive activation of the sympathetic nerve.
Many scholars are concerned about the safety of RDN; there
are some doubts regarding whether the internal membrane of
the renal artery is damaged by RDN and whether thrombosis
at the local ablation point or renal dysfunction can occur after
RDN. However, many investigators have reported that RDN
does not aggravate functional or structural renal damage;
rather, RDN may improve renal function by decreasing SNS
over-activation. Liang Xiao [30] recently performed a study in
an angiotensin II-induced hypertension model and reported
that RDN reduced renal inflammation by decreasing the
accumulation of total leukocytes, T cells and both CD4+ and
CD8+ T cells in the kidney, which were associated with a
marked reduction in renal fibrosis, albuminuria and
nephrinuria. Mahfoud [31] enrolled 100 consecutive patients
with resistant hypertension, and 88 underwent RDN. After 6
months follow-up, they reported that RDN reduced the renal
resistive index and the incidence of albuminuria without
adversely affecting glomerular filtration rate or renal artery
structure. Because of the special relationship between the
sympathetic nervous system and kidney, we also believe that
RDN has more beneficial effects on patients with CKD.
RDN and obstructive sleep apnea (OSA)
OSA is a highly prevalent disorder of breathing rhythm and
frequency during sleep. Increasing evidence suggests that OSA
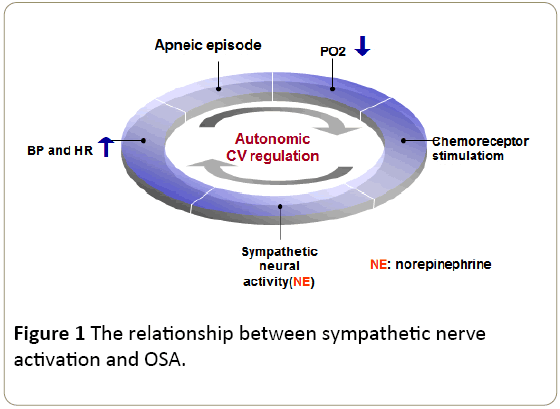
is independently associated with an increased risk of cardiovascular disease. We created the following figure (Figure
1) to demonstrate the relationship between sympathetic nerve
activation and OSA.
Figure 1: The relationship between sympathetic nerve
activation and OSA.
Early recognition and nasal CPAP treatment can improve
cardiovascular function [32]. Witkowski [29] reported that RDN
decreased the apnea-hypopnea index at 6 months after the
operation (median: 16.3 versus 4.5 events per hour; P=0.059),
which indicates that RDN might serve as an adjuvant therapy
for OSA. There is not sufficient evidence to prove that RDN can
serve as the main treatment for OSA, but RDN might be an
important auxiliary treatment. More clinical research is
necessary to confirm this.
RDN and other diseases (polycystic kidney,
polycystic ovarian syndrome)
The sympathetic nervous system effectively regulates body
functions and plays a pivotal role in the neuroendocrine
system. RDN decreases the activity of the SNS and significantly
influences hypertension, heart failure, diabetes,
atherosclerosis and other sympathetic over-activation
diseases. There are also some reports that RDN may be useful
in the treatment of non-cardiovascular diseases.
Chronic pain is a common concern in patients with
polycystic kidney disease. Casteleijn [33] reported a case of a
43-year-old woman with polycystic kidney disease whose
chronic pain could not be controlled by pain medication or
splanchnic nerve blockade but was successfully managed by
catheter-based RDN.
Polycystic ovary syndrome (PCOS) is a common endocrine
and metabolic disturbance disease clinically. It is associated
with long-term health risks, including type 2 diabetes and
vascular dysfunction. Lansdown [34] summarized the animal
and human studies of PCOS and found that RDN reduced
sympathetic nerve activity, which is increased in PCOS due to
increased production of noradrenaline, and improved insulin
sensitivity.
Conclusion
RDN, a novel non-pharmacological treatment strategy,
reduces sympathetic nervous activity. The results of numerous
studies have demonstrated the capability of RDN to inhibit the
excessive activation of SNS and to protect against sympathetic
over-activation related diseases. The exact mechanism
through which RDN decreases blood pressure, improves insulin
resistance and cardiac function, inhibits endothelium
inflammation, and so on is still unclear. Although the
Symplicity HTN-3 trial reported a negative findings regarding
the use of RDN in resistant hypertension in 2014, there is not
sufficient evidence to fully deny the application of RDN in
diseases other than resistant hypertension. To some extent,
RDN is a potential strategy, or novel therapeutic method, for
the prevention and/or treatment of sympathetic overactivation
related diseases.
Acknowledgement
The study was supported by the Hunan Provincial
Innovation Foundation for Postgraduate (no.CX2015B063), the
National Basic Research Program of China (973 Program) (no.
2014CB542400), and the National Natural Science Foundation
of China (no. 81370359).
References
- Talbott JH, Castleman B, Smithwick RH, Melville RS, Pecora LJ (1943) RENAL BIOPSY STUDIES CORRELATED WITH RENAL CLEARANCE OBSERVATIONS IN HYPERTENSIVE PATIENTS TREATED BY RADICAL SYMPATHECTOMY. J Clin Invest 22: 387-394.
- Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, et al. (2009) Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373: 1275-1281.
- Kandzari DE, Bhatt DL, Sobotka PA, O'Neill WW, Esler M, et al. (2012) Catheter-based renal denervation for resistant hypertension: rationale and design of the SYMPLICITY HTN-3 Trial. Clin Cardiol 35: 528-535.
- Bakris GL, Townsend RR, Flack JM, Brar S, Cohen SA, D'Agostino R, et al. (2015) 12-month blood pressure results of catheter-based renal artery denervation for resistant hypertension: the SYMPLICITY HTN-3 trial. J Am Coll Cardiol 65: 1314-21.
- Jiang W, Guo Y, Tan L, Tang X, Yang Q, et al. (2012) Impact of renal denervation on renalase expression in adult rats with spontaneous hypertension. Exp Ther Med 4: 493-496.
- Hatipoglu E, Ferro A (2013) Catheter-based renal denervation for treatment of resistant hypertension. JRSM Cardiovasc Dis 2: 2048004013486634.
- Yoshida M, Yoshida E, Satoh S (1995) Effect of renal nerve denervation on tissue catecholamine content in spontaneously hypertensive rats. Clin Exp Pharmacol Physiol 22: 512-517.
- Holmer S, Rinne B, Eckardt KU, Le Hir M, Schricker K, et al. (1994) Role of renal nerves for the expression of renin in adult rat kidney. Am J Physiol 266: F738-745.
- Voskuil M, Verloop WL, Blankestijn PJ, Agostoni P, Stella PR, et al. (2011) Percutaneous renal denervation for the treatment of resistant essential hypertension; the first Dutch experience. Neth Heart J 19: 319-323.
- Tung R, Shivkumar K (2015) Neuraxial modulation for treatment of VT storm. J Biomed Res 29: 56-60.
- Bourke T, Vaseghi M, Michowitz Y, Sankhla V, Shah M, et al. (2010) Neuraxial modulation for refractory ventricular arrhythmias: value of thoracic epidural anesthesia and surgical left cardiac sympathetic denervation. Circulation 121: 2255-2262.
- Turley AJ, Thambyrajah J, Harcombe AA (2005) Bilateral thoracoscopic cervical sympathectomy for the treatment of recurrent polymorphic ventricular tachycardia. Heart 91: 15-17.
- Cao JM, Fishbein MC, Han JB, Lai WW, Lai AC, et al. (2000) Shintaku IP, Chen PS, Chen LS. Relationship between regional cardiac hyperinnervation and ventricular arrhythmia. Circulation 101: 1960-1969.
- Ukena C, Mahfoud F, Spies A, Kindermann I, Linz D, et al. (2013) Effects of renal sympathetic denervation on heart rate and atrioventricular conduction in patients with resistant hypertension. Int J Cardiol 167: 2846-2851.
- Huang B, Zhou X, Wang S, Zhou L, Yu L, et al. (2015) Renal sympathetic denervation: A potential therapeutic approach for long QT syndrome. Int J Cardiol 197: 206-207.
- Remo BF, Preminger M, Bradfield J, Mittal S, Boyle N, et al. (2014) Safety and efficacy of renal denervation as a novel treatment of ventricular tachycardia storm in patients with cardiomyopathy. Heart Rhythm 11:541-6.
- Ukena C, Bauer A, Mahfoud F, Schreieck J, Neuberger HR, et al. (2012) Renal sympathetic denervation for treatment of electrical storm: first-in-man experience. Clin Res Cardiol 101: 63-67.
- Lorincz I, Szabo Z, Simko J, Szantho E, Barta K, et al. (2008) [Atrial fibrillation and the autonomous nervous system]. Orv Hetil 149: 2019-28.
- Nishida K, Datino T, Macle L, Nattel S (2014) Atrial fibrillation ablation: translating basic mechanistic insights to the patient. J Am Coll Cardiol 64: 823-831.
- Tofield A (2015) Recurrent atrial fibrillation reduced after renal denervation with pulmonary vein ablation in select patients. Eur Heart J 36: 257.
- Pokushalov E, Romanov A, Corbucci G, Artyomenko S, Baranova V, et al. (2012) A randomized comparison of pulmonary vein isolation with versus without concomitant renal artery denervation in patients with refractory symptomatic atrial fibrillation and resistant hypertension. J Am Coll Cardiol 60: 1163-1170.
- Davies JE, Manisty CH, Petraco R, Barron AJ, Unsworth B, et al. (2013) First-in-man safety evaluation of renal denervation for chronic systolic heart failure: primary outcome from REACH-Pilot study. Int J Cardiol 162: 189-192.
- Nozawa T, Igawa A, Fujii N, Kato B, Yoshida N, et al. (2002) Effects of long-term renal sympathetic denervation on heart failure after myocardial infarction in rats. Heart Vessels 16: 51-56.
- McLellan AJ, Schlaich MP, Taylor AJ, Prabhu S, Hering D, et al. (2015) Reverse cardiac remodeling after renal denervation: Atrial electrophysiologic and structural changes associated with blood pressure lowering. Heart Rhythm 12: 982-990.
- Dorr O, Liebetrau C, Mollmann H, Mahfoud F, Ewen S, et al. (2015) Beneficial effects of renal sympathetic denervation on cardiovascular inflammation and remodeling in essential hypertension. Clin Res Cardiol 104: 175-184.
- Wang H, Wang J, Guo C, Luo W, Kleiman K, et al. (2015) Renal denervation attenuates progression of atherosclerosis in apolipoprotein E-deficient mice independent of blood pressure lowering. Hypertension 65: 758-765.
- Jiang F, Li H, Zhu F, Zeng L, Wang X, et al.(2015) Investigation of the mechanism underlying the antihypertensive effect of catheter-based radiofrequency renal sympathetic denervation in hypertensive dogs. Biomed Rep 3: 254-260.
- Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, et al. (2011) Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study. Circulation 123: 1940-1946.
- Witkowski A, Prejbisz A, Florczak E, Kadziela J, Sliwinski P, et al. (2011) Effects of renal sympathetic denervation on blood pressure, sleep apnea course, and glycemic control in patients with resistant hypertension and sleep apnea. Hypertension 58: 559-565.
- Xiao L, Kirabo A, Wu J, Saleh MA, Zhu L, et al. (2015) Renal Denervation Prevents Immune Cell Activation and Renal Inflammation in Angiotensin II-Induced Hypertension. Circ Res.
- Mahfoud F, Cremers B, Janker J, Link B, Vonend O, et al. (2012) Renal hemodynamics and renal function after catheter-based renal sympathetic denervation in patients with resistant hypertension. Hypertension 60: 419-424.
- Otsuka K (2001) [Nasal CPAP treatment and hypertension and altered cardiovascular variability associated with obstructive sleep apnea (OSA)]. Nihon Rinsho 59: 983-991.
- Casteleijn NF, de Jager RL, Neeleman MP, Blankestijn PJ, Gansevoort RT (2014) Chronic kidney pain in autosomal dominant polycystic kidney disease: a case report of successful treatment by catheter-based renal denervation. Am J Kidney Dis 63: 1019-1021.
- Lansdown A, Rees DA (2012) The sympathetic nervous system in polycystic ovary syndrome: a novel therapeutic target? Clin Endocrinol (Oxf) 77: 791-801.