Key words
asylum seekers, mental health, refugees,
research
Introduction
This paper reflects on some of the unique challenges
faced by researchers in the field of mental health of
asylum seekers. We begin with a brief introduction to
the topic and present an overview of our mixedmethods
research, which focused on the mental health
of newly arrived asylum seekers living in Plymouth,
UK and their experiences of health and social care
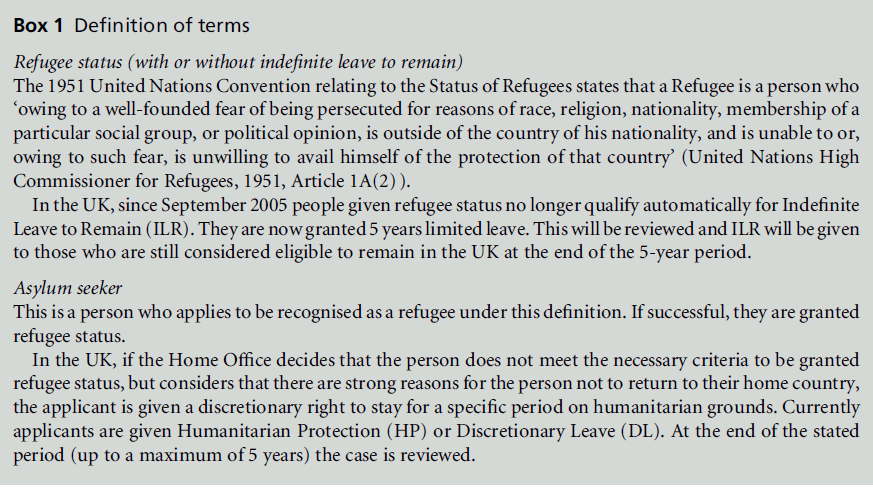
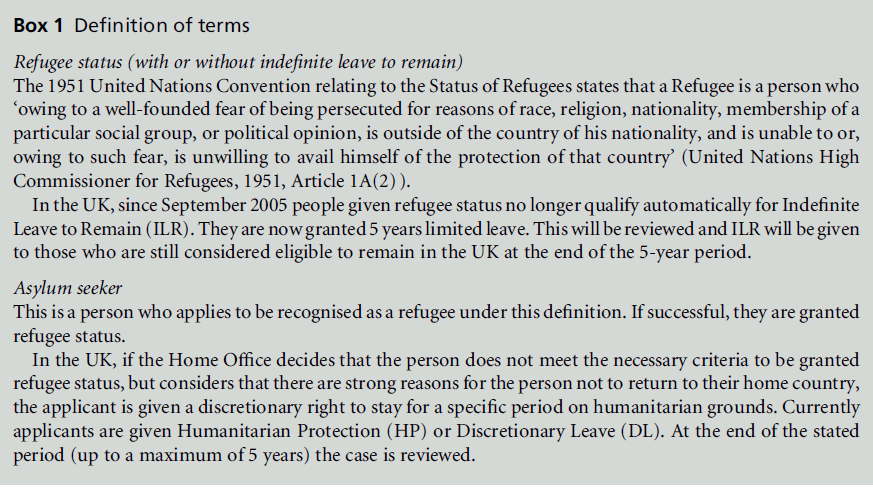
services (Bernardes et al, 2010; see Box 1). This
provides a basis for reflecting on the challenges that we experienced during this project, and offering our
suggested recommendations for ethical and culturally
competent research. In particular, we reflect upon
issues of accessing and engaging with participants
and obtaining informed consent, language, and dealing
with emotional aspects of the research. Recommendations
for tackling these issues are offered.
Mental health of asylum seekers
and refugees
Many asylum seekers demonstrate resourcefulness
and resilience in the face of their experiences. For
example, personal factors including cognitive strategies
such as reframing the situation, relying on their
inner resources, and focusing on future wishes and
aspirations have been described as helpful coping
strategies by Sudanese refugees living in Australia
(Khawaja et al, 2008). Social and family support and
cohesiveness have also been reported to be a protective
factor associated with increased psychological wellbeing
in refugees (McMichael and Manderson, 2004;
Schweitzer et al, 2007). The role of religion in increasing
resilience and helping refugees to cope with stress
has also been documented. For example, religion was
associated with resilienceamongBosnian refugeewomen
(Sossou et al, 2008), and with reducing acculturation
stress among Hindu Bhutanese refugees (Benson et al,
2011) in the USA. Other factors, such as employment
and job satisfaction, financial satisfaction and social
support, have also been found to predict life satisfaction
among refugees (Peisker-Colic, 2009). In addition,
access to health and social services, freedom and
positive media attitudes have all been described as
enablers of successful settlement (Papadopoulos et al,
2004). However, some asylum seekers and refugees,
and particularly survivors of torture and war, are
vulnerable to psychiatric disorders such as depression,
suicide and post-traumatic stress disorder (Fazel et al,
2005; Steel et al, 2009). In addition to traumatic premigration
experiences, difficulties in the country of
exile, such as detention, dispersal, social isolation and living difficulties, including poor accommodation,
unemployment, poverty, racism and discrimination,
can have an impact on the mental health of asylum
seekers and refugees (McColl et al, 2008; Sulaiman-
Hill and Thompson, 2012).
A great deal of research focusing on the mental
health of asylum seekers and refugees has focused on
symptoms of distress, namely post-traumatic stress
disorder, which has led some to question whether
western conceptions of ‘diagnosis’ and ‘distress’ can be
meaningfully applied (Bracken et al, 1995; Summerfield,
1999; Breslau, 2004). More recently, some authors have
started to make use of a variety of research methods,
such as participant observation and in-depth interviews,
in order to capture the multidimensional nature of the
asylum-seeking experience (e.g. Bernardes et al, 2010;
Misra et al, 2006; Papadopoulos et al, 2004; Sulaiman-
Hill and Thompson, 2012). These methods are crucial
for making explicit the details and complexity of
asylum seekers’ and refugees’ experiences.
Investigating the mental health
and service experience of asylum
seekers in Plymouth
We used mixed-methods research to investigate
asylum seekers’ perspectives on their mental health
and their views of local health and social services
(Bernardes et al, 2010). Our project examined the
mental health of asylum seekers who had recently
arrived in the UK by using mental health screening
questionnaires, as well as by conducting interviews that explored subjective experiences of the asylum
process and its potential impact on their mental
health, and participants’ suggestions for tackling mental
health needs. Ethical approval for our project was
granted by the local research ethics committee (Ref.
08/H0203/209) and NHS trust (Ref. PCT0646).
Sample and procedure
Asylum seekers who were waiting to hear the outcome
of their first asylum application, aged 18 and 65 years
(criteria set by AdultMental Health Services) and living
in the dispersal area of Plymouth, UK, were included
in the study. Over a 6-month period (February–
September 2009), 52 people were invited to take part
in a mental health screening while attending a health
clinic; of these, 13 individuals agreed to take part.
Asylum seekers who were receiving psychological support
from the local AsylumSeeker and Refugee Mental
Health Team were approached. Sixteen further participants
were recruited in this manner, giving a total
of 29 participants. All of them were assured that taking
part in the research would not affect their applications
for asylum, and that they could withdraw from the
study at any time without their medical and legal
rights being affected. All of the participants gave their
written informed consent. All of them completed all of
the questionnaires, except for four participants who
did not complete the PTSD Symptom Scale Interview.
In total, 19 participants (65%) were interviewed with
the assistance of accredited interpreters; the remaining
interviews were conducted in English.
Measures
To decide on which mental health screening measures
to use,we started by reviewing the literature on asylum
seekers’ and refugees’ mental health. We then invited
asylumseekers, refugees and local practitioners working
with them to review our findings and choose a final
set. The measures used included a shortened version of
the Post-Migration Living Difficulties (PMDL) scale
(Schweitzer et al, 2006) on which six items (such as
‘worry about family back home’)were rated on a 5-point
scale from ‘no problem’ to ‘a very serious problem.’
The Generalized Anxiety Disorder-7 (GAD-7) scale
(Spitzer et al, 2006) was included to assess the presence
of generalised anxiety disorder and the severity of
anxiety. Seven items (among them ‘feeling nervous,
anxious or on edge’; � = 0.88) were rated on a 4-point
scale from‘not at all’ to ‘nearly every day.’ Scores were
aggregated to provide the overall scale score. Cut-off
points of 5, 10 and 15 were interpreted as representing mild, moderate and severe levels of anxiety, respectively.
The Clinical Outcomes Routine Evaluation–
Outcome Measure (CORE-OM; Evans et al, 2002)
was used as a general measure of distress. This measure
consists of 34 items (� = 0.93) covering four domains,
namely subjective well-being, symptoms, life functioning
and risk. The sum of scores for all items was
used to ascertain levels of distress, in which cut-off
points of 20, 34, 51, 68 and 85 represented low, mild,
moderate, moderate to severe, and severe levels of
distress, respectively (CORE Net, 2008). A mean total
score was also calculated and multiplied by 10 so that
meaningful differences between scores were whole
numbers (scores range, 0–40). A cut-off value of 10
has been assumed to discriminate between clinical and
general populations (Connell et al, 2007). Finally, the
PTSD Symptom Scale–Interview (PSS-I; Foa et al,
1993) was used as a measure of trauma and PTSD
symptoms. Participants were presented with a list of
16 traumatic events or situations (e.g. having experienced
‘adult physical assault or abuse’ or ‘sudden
death of someone close to you’), and were asked to
select all of those that they had witnessed or experienced.
Participants were then asked to focus on the
traumatic event which ‘bothers you the most’ and
asked to rate 17 items (e.g. ‘feeling distant or cut off
from people around you’; � = 0.88) on a 4-point scale
from ‘not at all’ to ‘five or more times per week/very
much.’ These provided both diagnostic and severity
information about each of the DSM-IV criteria (American
Psychiatric Association, 2000) for PTSD. Sums of
raw items were calculated (score range, 0–51), and
cut-off values of 11, 21 and 36 were interpreted as
moderate, moderate to severe, and severe levels of
PTSD, respectively.
All of the participants who underwent the mental
health screening were invited to take part in in-depth
interviews 1 month later. Eight participants agreed to
be interviewed about their experiences of seeking
asylum, their mental health experiences while in the
UK, and their perspectives on how to tackle any mental
health problems. Accredited interpreters were used
when requested by participants (n = 6), and responses
were regularly clarified and repeated back verbatim to
the respondents for confirmation during the interview.
Participants were asked six general questions about
seeking asylum and mental health, elaborated in consultation
with asylum seekers and practitioners. Examples
of these questions include ‘Can you tell me
about your story of seeking asylum?’, ‘Can you tell me
about how being an asylum seeker is affecting your
mental health/well-being at the present time?’ and
‘What has been your experience of the local services,
such as GPs, mental health team or other services in
helping you with your mental health? What are your
recommendations for services?’ Questions were not
presented in a fixed order, but were introduced following the participants’ thought associations (Hollway
and Jefferson, 2000). Six interviews were taped and
transcribed with the participants’ consent. Two participants
did not consent to their interviews being
taped but agreed to the compilation of process notes
afterwards. The interview data were analysed using the
free-association narrative interview method, which
focuses on gestalt principles (Hollway and Jefferson,
2000).
Sample characteristics
In total, 26 of the 29 participants were male (90%).
The mean age of participants was 29.5 years (SD = 8.5
years), and they originated from 13 countries: Iran (n =
9), Zimbabwe (n = 3),Afghanistan (n = 3), Iraq (n = 2),
Sri Lanka (n = 2), Eritrea (n = 2), Ethiopia (n = 2),
Guinea (n = 1), Morocco (n =1), Cabinda (n = 1),
Sudan (n = 1), Kuwait (n = 1) and Turkey (n = 1). In
total, 18 participants (62%) had been in theUKfor less
than a year, four (14%) for 1–2 years, three (10%) for
2–4 years, two (7%) for 4–6 years and two (7%) for 6
or more years. The average waiting time for the asylum
application was 19.8 months (SD = 29.3 months). The
longest delay was 9 years. In total, 14 participants
(48%) were single, 13 (45%) were married, one was
divorced (3%) and one was widowed (3%). Before
migrating to the UK, 73% (n = 21) of the participants
were employed, and 14% (n = 4) were students. None
of them had ever been employed in the UK. In total, 25
participants (87%) were living temporarily in shared
accommodation, and the remainder were living alone
or with friends or relatives.
Quantitative findings
In total, 16 of the asylum seekers in our sample
presented with PTSD (76%), and 24 participants
(86%) presented with moderate or severe anxiety on
the GAD and moderate levels of psychological distress
on the CORE-EM. Asylum seekers’ scores on the
CORE-OM were significantly higher than those of
an indigenous sample of mental health service users
(Evans et al, 2002) and a primary care service user
sample (Barkham et al, 2005) in the domains of ‘wellbeing’
and ‘life functioning.’ Indeed, the asylum seekers
in our sample presented with significant post-migratory
living difficulties, mainly acculturation problems (n =
22; 76%), not being allowed to work (n = 24; 83%),
and worries about their family back in their home
country (n = 24; 86%). Other common problems were
communication (n = 20; 69%), discrimination (n = 15; 52%), and accessing health and welfare services
(n = 15; 52%) (Bernardes et al, 2010).
Quantitative findings
The interview data corroborated the quantitative data
and provided further insight into asylum-seeking
experiences. For example, all of the participants who
were interviewed (n = 8) reported feeling fear and
sadness about the uncertainty of the outcome of their
asylum application, while fear of deportation affected
their ability to carry out activities of daily living.
Moreover, participants reported difficulties related
to their wish for personal independence and to make
a new life while being dependent on others, and their
need for sanctuary. Social support was very important
to them in helping them to cope with these difficulties,
but opinions about sharing accommodation with
people from the same nationality or ethnic background
were mixed, with some participants finding
it helpful and others viewing it as problematic.
These findings corroborated other evidence that
both past and present social living experiences are
important determinants of asylum seekers’ mental
health (Schweitzer et al, 2006), and highlighted the
prevalence of post-migratory living difficulties. They
also indicated that psychological distress may be common
among asylum seekers. In the following sections
we reflect on our experience of this project and the
challenges that we encountered. We have grouped
these into five sections, namely enhancing the cultural
relevance of the research, engaging with participants
and the wider community, informed consent, language,
and dealing with safety and emotional issues.
This was the first time that the leading researcher
and the research team had undertaken a project with
asylum seekers, which may help to contextualise our
reflections.
Enhancing the cultural relevance of
the research
‘Cultural capability’ is defined as ‘improving the
capacity of the organisation in providing high-quality
service, irrespective of the ethnic or cultural background
of the people using the service. This is not
simply about making services more aware or sensitive
to the perceived cultural needs of individual users, but
is about improving the quality of care, by providing
good-quality but equal services to all those who come
into contact with mental health agencies’ (National
Institute for Mental Health in England, 2003, p. 22).
Achieving ‘cultural capability’ depends on a number
of organisational strategies and processes that are required in order for services to be culturally competent
and capable. This includes ‘developing the
workforce’ to ensure that staff possess the ‘attitudes,
behaviours, knowledge and skills necessary to work
respectfully and effectively with people from minority
ethnic communities’ (National Institute for Mental
Health in England, 2003, p. 22). At an organisational
level, it is argued that ‘statutory mental health providers
must work collaboratively with [the] local
voluntary sector in developing and sustaining a variety
of service models to meet the needs of minority ethnic
groups’ and that ‘mental health services should ensure
that services provided are congruent rather than conflicting
with cultural norms’, and the need for ‘ensuring
language access for persons who prefer a language
other than English’ is highlighted (National Institute
for Mental Health in England, 2003, p. 23).
In research terms, ‘cultural capability’ can be defined
as taking into account the culture and diversity
of a population when developing research ideas, conducting
research and drawing conclusions about the
applicability of the results (O’Brien et al, 2006).
Implicit here is the importance of learning about and
reflecting on one’s own culture, historical roots,
beliefs and values. This requires awareness not only
of other cultures and their values, but also of our own
attitudes towards those values (Fernando, 2002).
One of the challenges in our research was to ensure
that the design, methods and questionswere culturally
relevant. It was not possible to know in advance about
the 13 countries from which our participants originated,
so we began by establishing a research team of
asylum seekers and professionals with long-standing
experience of working with asylum seekers and refugees
with mental health needs. We found that the
ensuing collaboration was extremely valuable, enabling
us to learn about traditional cultural beliefs, systems
and values, and to incorporate these into the research
design. Our aim was to ensure that the measures
selected were sufficiently culturally appropriate for the
participants to trust us. The topic guide for interviews
was discussed and piloted with two asylum seekers,
whose feedback led to changes that made the questions
clearer from their perspective. We came to realise that,
in addition to ‘cultural capability’, we also had to be
sensitive to the socio-political context from which
participants originated; this involved familiarising
ourselves with current affairs. Bringing these reflections
to supervision and discussing them with the
research supervisor and other professionals was also
helpful in terms of making sense of and trying to
understand participants’ stories.
‘Cultural capability’ when undertaking research with
asylum seekers is dependent on meaningful engagement
with the research participants throughout each
study. Participation in diversity training, reading,
informalmedia (e.g. books,movies, radio programmes) and interaction with people from diverse cultural
backgrounds are just some ways in which the researcher
can be helped to develop an understanding
of the participants’ perspectives. In a wider context,
‘cultural capability’ requires official policies and processes
that enable organisations to improve access to
and quality of services for individuals from diverse
populations.
Engaging with participants and the
wider community
In the initial stages of our research, considerable time
and energy were spent on planning the research and
mapping localcommunity services workingwith asylum
seekers. The aim was to identify possible research partners
and community resources. However, other issues
soon became apparent. The representative of a community
group expressed her fear that collaborating in
the research would compromise the trusting relationships
that had been established with asylum seekers.
Participants also voiced their fears of saying anything
that might undermine their asylum applications. In
response, we tried to ensure that we presented transparent
research aims and that we were as clear as
possible about how we would protect the identity of
potential participants and community groups. Palmer
(2008) has suggested that a steering group which
reflects the community within which the research is
based can help to enable continuous communication
between researchers and those who are being studied.
Following his advice, we found that establishing a
consultative group of local asylum seekers and professionals
from the outset was extremely helpful for
developing trust. It provided a safe space in which to
discuss different points of view, and an opportunity to
share experiences.
However, this consultative group was not sufficient
to convince everyone. In total, 23 individuals declined
to take part; 12 people specifically mentioned fears
about how the information was going to be used. To
overcome this problem, amember of the research team,
who himself had sought asylum, contacted potential
participants to explain the aims of the study. This
helped to foster trust between researchers and participants.
We also told every participant that their participation
was voluntary, completely independent of
any decisions about their status, and that withdrawal
from the study would not affect their legal rights. However,
we also had to recognise the power difference
between ourselves and the participants. We have the
legal status to work and live in the UK, whereas the
asylum seekers were still in the process of finding out
whether they would be given this right. This difference
in legal status could lead some individuals to agree to
participate in the research on the grounds that refusing would compromise their asylum applications. In our
study, we used reflection, supervision and consultation
with community services and groups to help
researchers to clarify, both for themselves and for the
participants, their roles as researchers.
On reflecting on our experience, we recommend
that researchers are clear about the purposes of their
research from the beginning. They must be careful to
avoid raising expectations, as some people may believe
that participation in research will increase the likelihood
that their asylum application will be successful.
Researchers should also be as clear as possible about
the extent to which information is confidential, and
reflect on situations in which confidentiality may be
compromised (e.g. the use of interpreters, referral to a
mental health team, managing risk). Another suggestion
is that, when planning the research, consideration
should be given to the social and economic realities
of potential participants. Although the NHS research
governance guidelines do not approve of monetary
incentives for participation in research (Department
of Health, 2005), this is a matter that researchers ought
to consider, as asylum seekers are not entitled to work,
and they often live in deprived circumstances. A
consultative/steering group may help to elucidate
culturally appropriate ways of providing compensation,
such as expenses payments for research participation
and travel. In retrospect, we could have
offered travel vouchers or supermarket vouchers to
our participants as a way of reimbursing them for their
participation in the research, provided that these did
not compromise their benefits.
Informed consent
Health and social care researchers have a duty to
ensure that participants’ rights are protected, that they
are adequately informed about the research, and that
consent is freely given (Department of Health, 2005).
This is particularly important when undertaking research
with asylum seekers, many of whom will have
experienced complicated and traumatic events. Fears
of deportation, if their applications to stay in the UK
were refused, were a constant source of anxiety
(Palmer, 2008).
We found that although all of the participants gave
oral consent to participate in the study, two asylum
seekers were reluctant to give written consent. This
can be understood in terms of the concerns that
asylum seekers may have about formal documentation.
For example, one may speculate about fears
of how their information could be used against their
asylum application. Similarly, two out of eight participants
who agreed to in-depth interviews did not
consent to audio recording. Past experiences of forced
confessions or other negative past experiences may underlie these choices. The latter point demonstrates
that insistence on a signed consent form may not
always be achievable or desirable, especially if it increases
the participants’ anxieties. Informed consent
should encompass all aspects of the research participation
process, as some individuals may consent to
some aspects but not to all of them.
Language
For consent to be free, informed consent forms and
participant information sheets should be available in a
format that participants can access. This means that
researchers should ensure that both documents are
translated into the relevant languages by accredited
professionals. In our study, information was presented
verbally by telephone interpreters because we
could not anticipate which languages participants
would prefer. Even when we knew which languages a
participant spoke, we could not anticipate how that
person might wish to communicate. For example, one
participant who spoke Kikongo, but who was also
fluent in Portuguese, the first language of the lead
researcher, refused an interpreter and wanted to speak
in English in the study ‘because I want to adapt to life
in the UK.’
Before the study commenced, these interpreters
received training about confidentiality and anonymity
and were briefed about the research. They conducted
19 of our 29 interviews, usually by telephone. This was
a complex task because the translation of research
terminology is not always straightforward and wordto-
word translation is often impossible. It is important
that enough time is available to enable adequate
explanation and clarification of concepts. Good practice
should always be followed when working in partnership
with interpreters (Tribe, 2007), ensuring due
consideration not only of language but also of dialect
and/or gender, and of any potential political conflict
between interpreter and interviewee. On reflection, it
would have been helpful if the researcher who was
carrying out the mental health screenings and indepth
interviews had had prior training in working
with interpreters in order to foster alliance formation.
Dealing with safety and emotional
issues
In this section we reflect on the management of risk
and the emotional issues that can arise when undertaking
research with asylum seekers and refugees. In
our study, the safety of both researchers and participants
was considered and a careful risk assessmentwas
conducted before data collection started. Whenever
possible we conducted the interviews in places where there were other people about to provide support if
necessary.
We also recognised the possibility that some participants
might experience high levels of distress. All of
the participants were given information about mental
health services, and were provided with contact numbers
for local health and mental health organisations.
Eight out of the 13 participants who were assessed at
the health clinic were referred, with their consent, to
mental health services.
Interpreters were debriefed at the end of each
interview. We suggest that researchers should be
mindful of the potential risks to themselves posed by
the emotional impact of their data, as well as the risk of
re-traumatisation of the participants (Palmer, 2008).
Some practical ways of managing these issues include
the following:
• listening to the needs of participants and using
clinical judgement
• avoiding booking one interview straight after
another, to allow researchers enough time to process
the information gathered and debrief with the
research team
• having clear supervisory arrangements that include
supervision not only about the research process but
also about the content (i.e. focusing on what the
stories told by asylum seekers evoke in the researchers)
• keeping a reflective diary in which feelings and
thoughts evoked during the project are noted and
then brought to supervision for discussion. For
example, the lead researcher noted that while
carrying out in-depth interviews she felt compelled
to adopt a ‘rescuer role’ towards asylum seekers.
Supervision was helpful in providing a space in
which these feelings could be openly discussed.
Conclusion
Researching asylum seekers’ experiences may create
numerous challenges which need to be thoughtfully
considered and addressed. We hope that our reflections
on some of these challenges, and our practical
suggestions, will be of use to others working in this
field.
ACKNOWLEDGEMENTS
We would like to thank our participants and colleagues
who have inspired our thinking. We also wish
to acknowledge and thank the editors and Allyson
Bailey (Research and Development Officer at NHS
Forth Valley) for their valuable suggestions for improving
our paper.
References
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, 4th edn. Washington, DC: American Psychiatric Association.
- Barkham M, Gilbert N, Connell J et al (2005) Suitability and utility of the CORE-OM for assessing severity of presenting problems in psychological therapy services based in primary care and secondary care settings. British Journal of Psychiatry 186:239ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â46.
- Benson GO, Sun F, Hodge D et al (2011) Religious coping and acculturation stress among Hindu Bhutanese: a study of newly resettled refugees in the United States. International Social Work 55:538ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- Bernardes D, Wright J, Edwards C et al (2010) Asylum seekersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ perspectives about their mental health and views on health and social services: contributions for service provision using a mixed-methods approach. International Journal of Migration, Health and Social Care 6:3ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â19.
- Bracken PJ, Giller JE and Summerfield D (1995) Psychological responses to war and atrocity: the limitations of current concepts. Social Science and Medicine 40:1073ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â82.
- Breslau J (2004) Cultures of trauma: anthropological views of posttraumatic stress disorder in international health. Culture, Medicine and Psychiatry 28:113ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â26.
- Connell J, Barkham M, StilesWBet al (2007) Distribution of CORE-OM scores in a general population, clinical cut-off points and comparison with the CIS-R. British Journal of Psychiatry 19:69ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â74.
- Department of Health (2005) Research Governance Framework for Health and Social Care. www.dh.gov.uk/prod_ consum_dh/groups/dh_digitalassets/@dh/@en/documents/ digitalasset/dh_4122427.pdf (accessed 23 February 2012).
- Evans C, Connell J, Barkham M et al (2002) Towards a standardized brief outcome measure: psychometric properties and utility of the CORE-OM. British Journal of Psychiatry 180:51ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â60.
- Fazel M, Wheeler J and Danesh J (2005) Prevalence of serious mental health disorder in 7000 refugees resettled in western countries: a systematic review. Lancet 365: 1309ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â14.
- Fernando S (2002) Mental Health, Race and Culture. Basingstoke: Palgrave.
- Foa EB, Riggs DS, Dancu CV et al (1993) Reliability and validity of a brief instrument for assessing posttraumautic stress disorder. Journal of Traumatic Stress 6:459ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â73.
- Hollway W and Jefferson T (2000) Doing Qualitative Research Differently: free association, narrative and the interview method. London: Sage.
- Khawaja NG, White K, Schweitzer R et al (2008) Difficulties and coping strategies of Sudanese refugees: a qualitative approach. Transcultural Psychiatry 45:489ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â512.
- McColl H, McKenzie K and Bhui K (2008) Mental health care of asylum seekers and refugees. Advances in Psychiatric Treatment 14:452ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- McMichael C and Manderson L (2004) Somali women and well-being: social networks and social capital among immigrant women in Australia. Human Organization 63:88ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â99.
- Misra T, Connolly AM and Majeed A (2006) Addressing mental health needs of asylum seekers and refugees in a 208 D Bernardes, J Wright and AG Livingstone London Borough: epidemiological and user perspectives. Primary Care Research and Development 7:241ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â8.
- National Institute for Mental Health in England (2003) Inside Outside: improving mental health services for black and minority ethnic communities in England.
- www.dh. gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/ @en/documents/digitalasset/dh_4019452.pdf (accessed 4 June 2012).
- OÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢Brien RL, Kosoko-Lasaki O, Cook CT et al (2006) Selfassessment of cultural attitudes and competence of clinical investigators to enhance recruitment and participation of minority populations in research. Journal of the National Medical Association 98:674ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â82.
- Palmer D (2008) Ethical issues and their practical application in researching mental health and social care needs with forced migrants. Research Ethics Review 4:20ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â25.
- Papadopoulos I, Lees S, Lay M et al (2004) Ethiopian refugees in the UK: migration, adaptation and settlement experiences and their relevance to health. Ethnicity and Health 9:55ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â73.
- Peisker-Colic V (2009) Visibility, settlement success and life satisfaction in three refugee communities in Australia. Ethnicities 9:175ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â99.
- Schweitzer R, Melville F, Steel Z et al (2006) Trauma, postmigration living difficulties and social support as predictors of psychological adjustment in resettled Sudanese refugees. Australian and New Zealand Journal of Psychiatry 40:179ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â87.
- Schweitzer R, Greenslade JH and Kagee A (2007) Coping and resilience in refugees from the Sudan: a narrative account. Australian and New Zealand Journal of Psychiatry 41:282ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â8.
- Sossou M, Craig C, Ogren H et al (2008) A qualitative study of resilience factors of Bosnian refugee women resettled in the southern United States. Journal of Ethnic and Cultural Diversity in Social Work 17:365ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â85.
- Spitzer RL, Kroenke K, Williams JBW et al (2006) Brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine 166:1092ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Steel Z, Chey T, Silove D et al (2009) Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Journal of the American Medical Association 302:537ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â49.
- Sulaiman-Hill CMR and Thompson SC (2012) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âThinking too muchÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: psychological distress, sources of stress and coping strategies of resettled Afghan and Kurdish refugees. Journal of Muslim Mental Health 4:63ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â86.
- Summerfield D (1999) Sociocultural dimensions of war, conflict and displacement. In: A Ager (ed.) Refugees: perspectives on the experience of forced migration. London: Pinter. pp. 111ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â35.
- Tribe R (2007) Working with interpreters. The Psychologist 3:159ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â61. United Nations High Commissioner for Refugees (1951) The 1951 Refugee Convention. Geneva: UNHCR.