- (2012) Volume 13, Issue 2
Suzanne Russo1*, John Chabot2, Muhammad Wasif Saif2
1Department of Radiation Oncol ogy, Mitchell Cancer Institute, University of South Alabama. Mobile, AL, USA
2Division of Hematology and Oncol ogy, Department of Medicine, Columbia University Medical Center. New York, NY, USA
Controversy exist regarding the potential benefit of the neoadjuvant approach to pancreatic cancer as limited retrospective data exists comparing pre- with post-operative chemoradiation. The optimal treatment approach remains unclear as we await prospective randomized clinical trials evaluating the hypothesized benefit of the neoadjuvant therapy for resectable pancreatic cancer and as there has been no proven survival benefit to date. Here we summarize the data presented at the 2012 American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium providing additional insight into the potential of neoadjuvant therapy in the treatment of pancreatic cancer. (Abstracts #156, #162, #168 and #177).
Laparoscopy; Neoadjuvant Therapy; Pancreatic Neoplasms; Proteomics
QALM: quality-adjusted life months; SOMAmer: slow off-rate modified aptamer
Neoadjuvant chemotherapy and radiation has been used in the treatment of patients with pancreas cancer in attempt to improve outcome for those with resectable or borderline resectable tumors. Some believe that early delivery of systemic therapy by using a preoperative approach may improve outcome by addressing subclinical metastatic disease earlier in the course of care [1, 2, 3] or improve margin negative resection local control rates [4]. Furthermore, early delivery of chemoradiation may identify those patients with therapy-resistant tumors or rapidly progressive disease who likely would not benefit from aggressive surgical management.
There are limited retrospective data comparing prewith post-operative chemoradiation that demonstrated no survival benefit, and no prospective randomized trials have been completed demonstrating the hypothesized benefit to the neoadjuvant approach for resectable pancreatic cancer. Although neoadjuvant approaches have also been utilized to improve R0 resection rates for patients with borderline resectable pancreas cancers, it remains difficult to draw conclusions from these studies as there was no consistent definition of borderline resectable. To further evaluate the potential benefit of the neoadjuvant approach for pancreatic cancer, a meta-analysis reviewed data from 111 studies including 4,394 patients who had received neoadjuvant therapy [4]. Patients were divided into initially resectable vs. borderline/potentially resectable patients. Ninety-six percent of patients received chemotherapy and 94% received radiation (24-63 Gy). In the resectable patient population, 74% of patients underwent surgery with 4% complete responses and 31% partial responses observed. In the borderline/potentially resectable patient population, 33% of patients underwent surgery resulting in 5% complete responses 30% partial responses. There was no difference in the rates of progressive disease (21%) and median survival following resection was similar for both groups (23 months and 21 months, respectively).
As the optimal sequence of treating pancreatic cancer with chemotherapy, radiation and surgery remains elusive and we anticipate additional data to further clarify the role of neoadjuvant therapy for resectable/borderline/potentially resectable pancreatic cancer. Most neoadjuvant regimens have incorporated either 5-fluorouracil (5-FU) or gemcitabine with radiation. Currently, the Interdisciplinary Working Group of Gastrointestinal Tumors is enrolling patients in a prospective randomized phase II trial (NCT00335543) in which patients with locally resectable pancreatic cancer are randomized to surgery followed by adjuvant chemotherapy versus neoadjuvant chemoradiation with gemcitabine, cisplatin, and 50.4 Gy radiation followed by surgery and adjuvant chemotherapy [5]. In addition, investigators are continuing to evaluate appropriate selection criteria to guide therapy decisions, as well as turning attention to economic considerations impacted by treatment management.
Neoadjuvant Chemoradiation versus Surgery First for Resectable Pancreatic Head Adenocarcinoma: An Economic and Outcome Analysis (Abstract #156 [6])
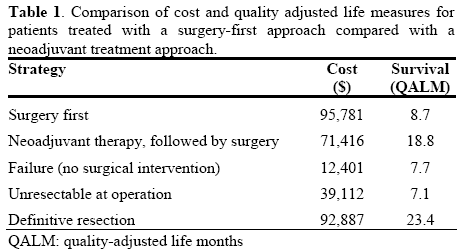
In Dr. Daniel Erik Abbott’s oral presentation and the corresponding abstract, the cost effectiveness of utilizing a neoadjuvant approach for the treatment of pancreatic cancer compared to the surgery first approach was explored. In this study the cost and outcome of surgery as the first treatment modality was compared with neoadjuvant chemoradiation followed by surgery using a decision model designed to contrast the two treatment strategies. Methods utilized by the authors included the National Cancer Data Base (NCDB; 2003-2005; www.facs.org/cancer/ncdb/ index.html), the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP, 2005-9 or 2005-2009; www.acsnsqip.org) and literature to populate probabilities and outcomes for the surgery first group, and data from a personal computer database at Dr. Abbott’s institution (2002-2008) to populate data for the neoadjuvant group. Operative outcome, complication rate, pathologic stage, adjuvant therapy, stage-specific survival, and survival reported in quality-adjusted life months (QALM), were reported for each group. Costs were estimated based on 2011 Medicare reimbursement. In this analysis, 164 patients received neoadjuvant chemoradiation, but only 78% underwent surgery for a variety of reasons including metastases (50%), poor performance status (47%), unresectable disease demonstrated at the time of laparotomy (7%), and refusal (3%). Taking this data into account, the estimated cost of the neoadjuvant strategy was $71,416 to achieve 18.8 QALM for those patients proceeding to definitive resection, compared to $95,781 to yield survival of 8.7 QALM for the surgery first approach. Further stratification of subgroups in the neoadjuvant population also demonstrated cost effectiveness when compared to the surgery first group (Table 1). The authors concluded that treating patients with a neoadjuvant approach not only has the potential to identify patients who can be spared a surgery that might not provide benefit, but may also improve survival at significantly lower cost [6].
The previous abstract provides compelling data to incorporate neoadjuvant therapy in the treatment of resectable pancreatic cancer. In the presented series, of the 22% of patients initially deemed to have resectable tumors half demonstrate distant metastases suggestive of tumor biology unresponsive to therapy, and almost another 10% demonstrated locally unresectable disease at the time of surgery not appreciated at the time of diagnosis. In this regard, there were several other abstracts reported at 2012 ASCO GI Cancer Symposium that focused on predictive methods to better select patients who may benefit from surgery. Utilization of such methods may potentially further enhance cost effectiveness when incorporated in treatment decisions for those patients considered for neoadjuvant treatment.
Is Laparoscopy Still Needed for Staging Resectable Pancreatic Cancer? (Abstract #168 [7])
In this abstract Santoro et al. discussed how improvements in imaging techniques for pancreatic cancer has led to controversy regarding the relative benefit of diagnostic laparoscopy prior to laparotomy and resection. The hypothesis of this study was that laparoscopy is still necessary to detect occult disease and avoid non-curative surgery in a subset of patients. The authors retrospectively reviewed patient data from a large, academic community-based tertiary care center with a specialized pancreatic team. One hundred and seven patients with pancreatic adenocarcinoma were identified as having radiographically resectable tumors by triple phase computed tomography. Of these, 27 patients underwent laparotomy without laparoscopy and 15% were found to have metastatic disease at the time of surgery. Eighty patients underwent diagnostic laparoscopy (75%) and metastatic disease was identified in (10%). Subsequent laparotomy in these patients identified an additional 6 patients with metastatic disease that was missed during initial laparoscopy resulting in a total 18% of patients initially thought to have resectable tumors based on imaging studies. Thus, the sensitivity of laparoscopy to detect radiographically occult metastases was 70%, however laparoscopy still missed.
Forty-three percent (6/14) of patients ultimately found to have metastatic disease. The authors concluded that though laparoscopy is not perfect approximately 10% of patients can be spared an unnecessary laparotomy [7].
Revisiting the Prognostic Significance of Positive Peritoneal Cytology in Pancreatic Cancer (Abstract #177 [8])
In this study by Chen et al. designed to evaluate the significance of positive peritoneal cytology following neoadjuvant therapy, data from 185 patients with pancreatic adenocarcinoma who had undergone peritoneal washings with cytology at the time of resection were reviewed and outcomes were analyzed. Twenty patients (11%) had positive peritoneal cytology at the time of planned resection and 11 of these patients (55%) received neoadjuvant therapy prior to surgery. Of the 165 patients (89%) who had negative peritoneal cytology at the time of planned resection, 75 (45%) received neoadjuvant therapy prior to surgery. All patients without visible evidence of metastatic disease proceeded with resection. Overall, patients with positive peritoneal cytology demonstrated worse disease-free and overall survival compared to those patients with negative cytology, and the 2-year overall survival rate was 42% for negative cytology compared to 20% for positive cytology.
Interestingly, further investigation using mutivariable classification and regression tree (CART) analysis demonstrated that patients with stage II or greater pancreatic adenocarcinoma who did not receive neoadjuvant therapy with positive peritoneal cytology experienced a statistically significant worse diseasefree survival, in contrast to those patients with stage II or higher disease with positive peritoneal cytology who receive neoadjuvant therapy who did not demonstrated statistically significant detriment in disease-free or overall survival. The authors concluded the prognostic significance of positive peritoneal cytology historically predictive of poor survival is not associated with worse survival in patients with stage II and higher disease receiving neoadjuvant therapy [8].
Detection of Resectable Pancreatic Cancer with SOMAmer Proteomic Technology (Abstract #162 [9])
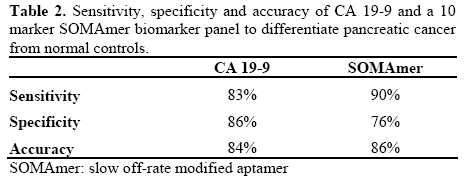
This study by Brand et al. which focused on detection in high-risk populations that may benefit from early intervention, investigated the utility of a slow off-rate modified aptamer (SOMAmer) proteomics platform to identify a biomarker panel that discriminates between pancreatic cancer and normal patients. Plasma samples obtained from a single institution included 100 pancreatic cancer patients and 69 normal controls or patients with acute and chronic pancreatitis, and an independent blinded validation set from another institution with 43 pancreatic cancer and 47 control samples. Of the 143 pancreatic cancer patients, 96 had resectable stages I-IIb. Samples were analyzed for 825- proteins and biomarkers were identified by Random ForestsTM backwards selection. A secondary goal was to compare the panel with CA 19-9. CA 19-9 levels were available on a subset of the patients and a level of CA 19-9 greater than 40 U/mL was defined as positive. Investigators found that 37 markers were significantly different between cases and controls and a 10 marker Random Forests classifier demonstrated an AUC of 0.91 and 0.90 for the training and independent validation set, respectively. When the 10 marker SOMAmer biomarker panel was compared to CA 19-9 levels, a 78% agreement was demonstrated between the two tests. The authors concluded that sensitivity could be maximized with minimal sacrifice of specificity by combining either test positive (95% and 66%, respectively), or conversely maximize specificity (97%) with a lower sensitivity of 77% if both tests are positive (Table 2). They recommended further investigation to assess potential applications of these panels for risk assessment in high risk individuals, who may be identified for surgical intervention in the early stages of pancreatic cancer [9].
Neoadjuvant therapy for resectable pancreatic cancer may provide potential advantages including early delivery of systemic treatment, which may influence survival for patients whose tumors respond to therapy, and the ability to avoid surgery in those patients who have rapidly progressive disease or occult metastases that do not respond to treatment. Preoperative therapies are generally better tolerated than postoperative regimens, and may identify patients who will not tolerate systemic therapies or surgery, selecting out patients who would benefit the most from resection. Approximately 20 to 30% of patients who have surgery for pancreatic cancer fail to receive planned adjuvant therapy due to refusal after a major surgery or poor tolerance [10]. In addition, there are often delays in initiation of adjuvant therapy due to prolonged recovery time, which can result in high systemic and local failure rate. Tumor response prior to resection may also result in improved margin negative resection rates and lower recurrence rates [4], as well as result in a decrease in surgical complications, as anastomotic leaks are less frequent when preoperative radiation is delivered [11]. Furthermore, the effects of radiation and chemotherapy are theoretically enhanced in better perfused and oxygenated tissue prior to surgery.
We await randomized clinical trials comparing neoadjuvant therapy to adjuvant therapy in pancreatic adenocarcinoma to provide clinical evidence to support these theoretical advantages. As it remains unclear whether neoadjuvant therapy offers an advantage or survival benefit over the surgery first approach, the economic and outcome analysis discussed in this paper provided thought-provoking and compelling arguments to consider routine use of the neoadjuvant approach in the treatment of patients with resectable pancreatic adenocarcinoma [6]. In addition, better selection of patients for neoadjuvant therapy may also potentially improve outcome for a subset of patients being considered for neoadjuvant therapy. Although there have been substantial improvements in imaging techniques for pancreatic cancer, patient selection remains limited as approximately 15% of patients thought to have resectable tumors as defined on imaging are found to have metastases on staging laparoscopy [7]. Even though staging laparoscopy improves the ability to identify patients with surgically resectable disease, it still fails to identify 10% of patients with metastases [7] indicating the need for further improvement in patient selection. The sensitivity and specificity of screening may be enhanced by incorporation of serum biomarkers in combination with CA 19-9 for risk assessment in high risk individuals, who may be identified for surgical intervention in the early stages of pancreatic cancer and further investigation is warranted [9]. Interestingly, the predictive value of prognosticators of poor outcome demonstrated in the surgery first approach may not apply to preoperative treatments [8] and need further evaluation in the neoadjuvant setting.
In conclusion, the data presented at the 2012 ASCO GI Cancers Symposium provides compelling data for neoadjuvant therapy for pancreatic cancer with the challenge to identify methods to more accurately evaluate appropriate selection criteria to guide therapy decisions.
The authors have no potential conflict of interest