- (2012) Volume 13, Issue 2
Muhammad Wasif Saif
Columbia University College of Physicians and Surgeons. New York, NY, USA
Blood Vessels; General Surgery; Neoplasm Staging; Pancreas; Pancreatic Neoplasms
In 2010, there were an estimated 43,140 new cases of pancreatic ductal adenocarcinoma and 36,800 deaths from pancreatic cancer in the United States [1]. This represents the 10th most common cancer diagnosis but the 4th most common cause of cancer-related death among men and women (6% of all cancer-related deaths), highlighting the disproportionate mortality associated with this diagnosis [2].
Sadly, only 20% patients are “resectable” at the time of diagnosis [3]. Pancreatic cancer is “resectable” if the tumor is confined to the pancreas without the encasement of adjacent surrounding major vessels, or distant metastases. Even among those patients who undergo resection for pancreatic cancer and have tumor-free margins, the 5-year survival rate after resection is 10-25% and the median survival is 15-19 months [3]. “Locally advanced pancreatic cancer” is defined as the tumor that has a local invasion: arterial (celiac trunk, hepatic artery, superior mesenteric artery) or venous (portal vein, superior mesenteric vein) but not metastasized, and represents about 25% of pancreatic cancer cases at presentation [4]. Locally advanced stage is associated with a median survival of 6-10 months. The vast majority of these patients develop metastatic disease within the first year of therapy. The tumor is considered “advanced” when it has metastasized to other organs, such as the liver or distant areas of the abdomen. Approximately 45% to 55% of patients are diagnosed at this stage. The prognosis of patients with advanced disease remains extremely poor, with a median survival of 6 months [5].
The staging system for pancreatic exocrine cancer continues to evolve. Staging information helps to determine appropriate treatment and to predict a patient’s prognosis. It is important that like surgery, the staging of pancreatic cancer should be done at a specialized and experienced center.
There are different stage descriptions for different types of cancer.
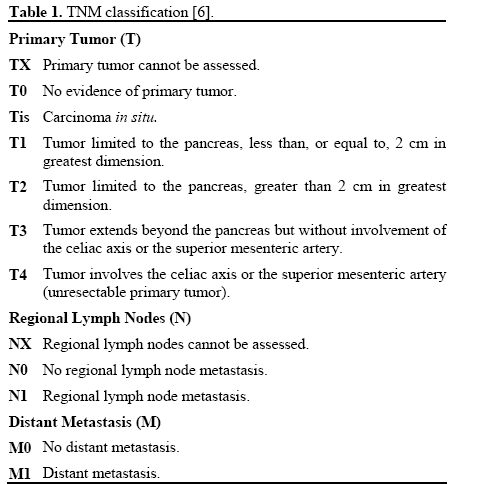
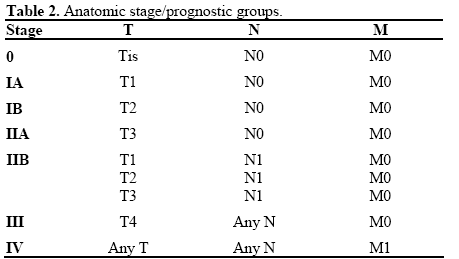
TNM Classification
The TNM classification [6] (Tables 1 and 2) often applied for other solid tumors is not usually used for pancreatic cancer.
The significance of staging beyond that of resectable and unresectable is uncertain in this disease because standard therapies have demonstrated mild impact on survival. Historically, the more common way to classify pancreatic cancer is to divide it into three categories based on whether it can be removed with surgery and where it has spread.
Staley’s Classification
Staley’s classification offers a simple model for groups engaged in protocol-based clinical research examining innovative multimodality treatment strategies for patients with pancreatic cancer (Table 3) [7]. His group examined the impact of standardized pathologic evaluation of pancreaticoduodenectomy specimens on the identification of regional lymph nodes and describes a detailed system for the pathologic analysis of the pancreaticoduodenectomy specimen.
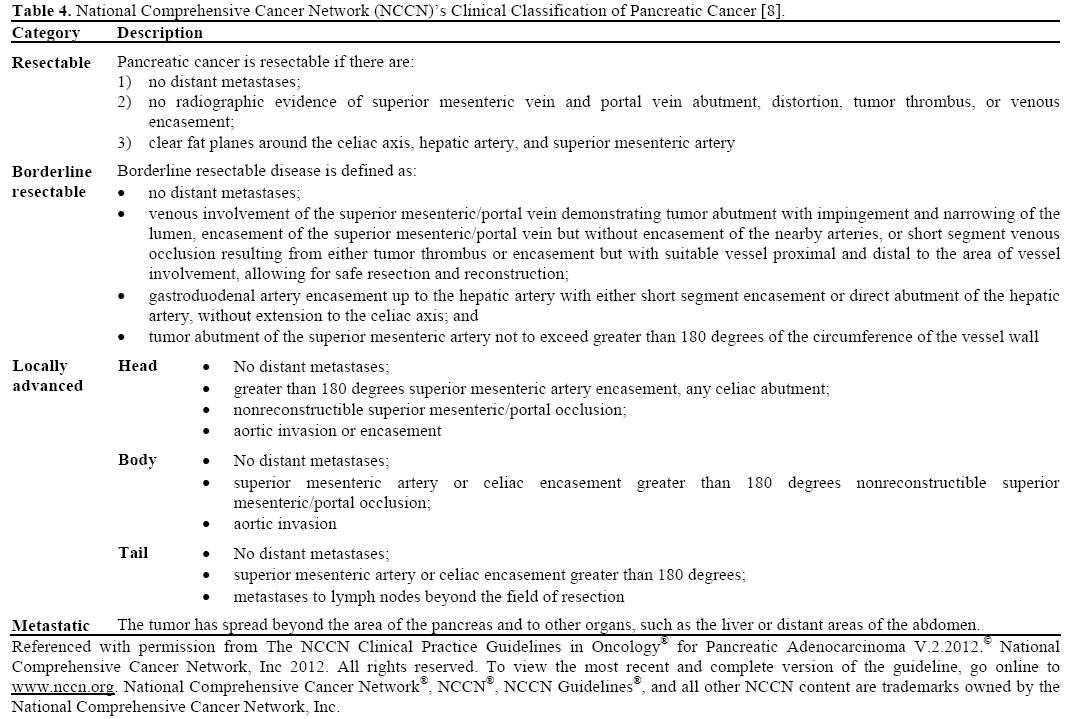
National Comprehensive Cancer Network (NCCN)’s Clinical Staging of Pancreatic Cancer
A fourth category that is now been recognized is called “borderline resectable”. This may be a subcategory of “locally advanced”, disease with limited vascular involvement by tumor. These patients may respond to therapy and may be resected. NCCN guidelines define now four clinical stages of pancreatic cancer (Table 4), which are now guiding investigators and physicians to determine treatment and to define clinical studies [8]. This classification has been adopted well as evidenced by studies presented at the 2011 ASCO Gastrointestinal Cancers Symposium, held in January 2012 in San Francisco [9, 10, 11, 12].
It is crucial to understand that the clinical staging system is based on the results of pre-surgical imaging studies. Because the only potential cure is through surgery, all patients with potentially resectable lesions by CT criteria should be referred for surgical consultation. But reality at the time of surgery may be more complex, and a tumor with no vascular invasion may be found to be “non-resectable” because of “desmoplastic reaction”. Due to the poor survival in patients with metastatic cancer and the high incidence of post-pancreatectomy recurrence, the patients with unresectable pancreatic cancer should be considered for inclusion into investigational trials. Expertise of surgeons in radical and revascularization techniques may significantly influence tumor resectability. Therefore, surgical resection should be performed to high volume and specialist centers to increase resection rates and reduce hospital morbidity and mortality.
The authors have no potential conflicts of interest