Rita F Wehrman1*, Lionel Sebbag1, Chris M Reilly2, Rachel A Allbaugh1, Gil Ben-Shlomo1, Erika P Berger1 and Margaret L Musser1
1Department of Veterinary Clinical Sciences, College of Veterinary Medicine, Iowa State University, 1809 South Riverside Drive, Ames, IA, 50011, USA
2Insight Veterinary Specialty Pathology, 215 C Street, Suite 301, Davis, CA, 95616, USA
- *Corresponding Author:
- Rita Wehrman
Department of Veterinary Clinical Sciences, College of Veterinary Medicine, Iowa State University, 1809 South Riverside Drive, Ames, IA, 50011, USA
Tel: 515-294-4900
E-mail: rwehrman@iastate.edu
Received Date: February 01, 2019; Accepted Date: February 20, 2019; Published Date: February 23, 2019
Citation: Wehrman RF, S ebbag L, Reilly C M, A llbaugh RA, B en-Shlomo G , et a l. ( 2019) Richter’s Syndrome as an Ocular Manifestation of Systemic Disease in a Dog: A Case Report. J Vet Med Surg. Vol. 3 No. 1:22.
Copyright: © 2019 Wehrman RF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source is credited.
Introduction
Lymphoma is a common malignant neoplasm in dogs, but a lesser known variant is Richter’s syndrome. Richter’s syndrome (RS) is defined as a clinical condition in which indolent chronic lymphocytic leukemia (CLL) transforms into aggressive high-grade lymphoma. RS is a well-documented condition in humans, with an overall prevalence of up to 20% in the CLL population [1]. Clinically, patients typically present with abdominal pain due to organomegaly [1]. Diagnosis is confirmed via biopsy of the affected tissue, coupled with a history of CLL. Unfortunately, the prognosis is grave [1]. Most cases of RS in humans (90%) result from the transformation of a B-cell CLL into a B-cell lymphoma [1,2]. The transformation of T-cell CLL into large T-cell lymphoma is exceedingly rare and to our knowledge, only one human case report exists [1].
Although RS has been previously described in animals, the syndrome is rare in veterinary medicine with less than a dozen cases reported in dogs to date [3-5]. A recent retrospective study described 153 dogs with CLL, in which 8 cases (5.2%) developed RS – 6 having a B-cell immunophenotype and 2 having a T-cell immunophenotype [4]. None of these cases had ocular manifestations. Here we report the clinical features, diagnostic test results, and outcome of a dog that was diagnosed with T-cell RS based on initial ophthalmic complaint. This is the first case report to describe RS as an ocular manifestation in any veterinary species.
Case Description
A 10-year-old, 20 kg, spayed female, treeing walker coonhound was presented to Iowa State University’s Lloyd Veterinary Medical Center (ISU-LVMC) Ophthalmology service for a protruded left globe of 1 week duration. Previously, the dog was in clinical remission for T-cell CLL that was diagnosed 1.5 years prior to presentation and managed with prednisone (5 mg PO q 24 h) and chlorambucil (2.5 mg PO q 24 h) by the ISU-LVMC Oncology service.
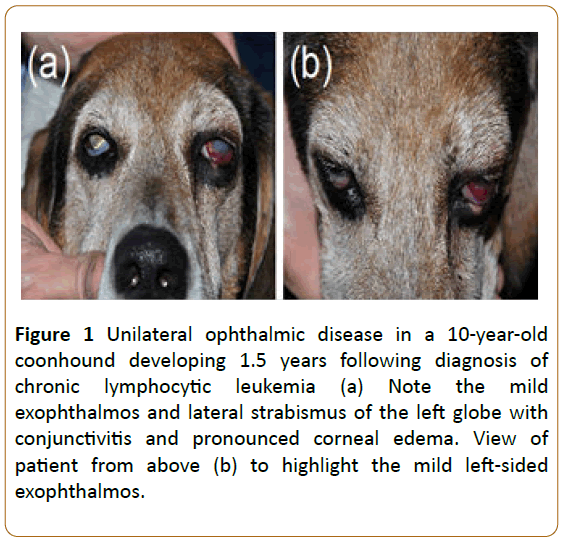
On physical examination, the dog was quiet, alert, and responsive with slightly tacky, pink mucous membranes, but normal capillary refill time, respiratory rate, and heart rate. The rectal temperature was mildly elevated at 102.9 °F. The patient’s oral cavity was unremarkable, and no pain was elicited upon opening the jaws. Lymph node palpation was within normal limits. Ophthalmic examination was unremarkable in the right eye, but revealed several abnormalities in the left eye, including vision loss (absent menace response and dazzle reflex), mild exophthalmos and resistance to globe retropulsion, mild lateral strabismus, severe conjunctival hyperemia and chemosis, and diffuse marked corneal edema that precluded visualization of the intraocular structures (Figure 1). The intraocular pressure was measured with rebound tonometry and was elevated at 35 mmHg. Based on the examination findings a retrobulbar mass was suspected.
Figure 1: Unilateral ophthalmic disease in a 10-year-old coonhound developing 1.5 years following diagnosis of chronic lymphocytic leukemia (a) Note the mild exophthalmos and lateral strabismus of the left globe with conjunctivitis and pronounced corneal edema. View of patient from above (b) to highlight the mild left-sided exophthalmos.
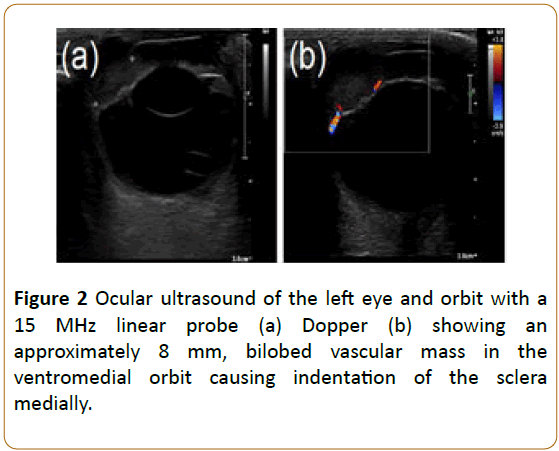
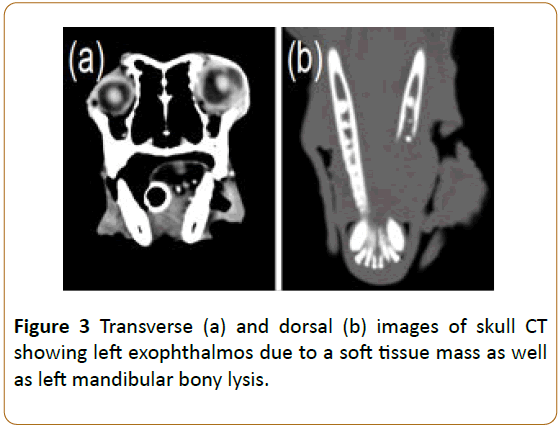
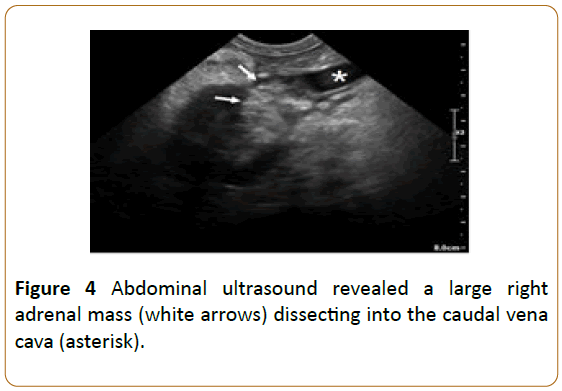
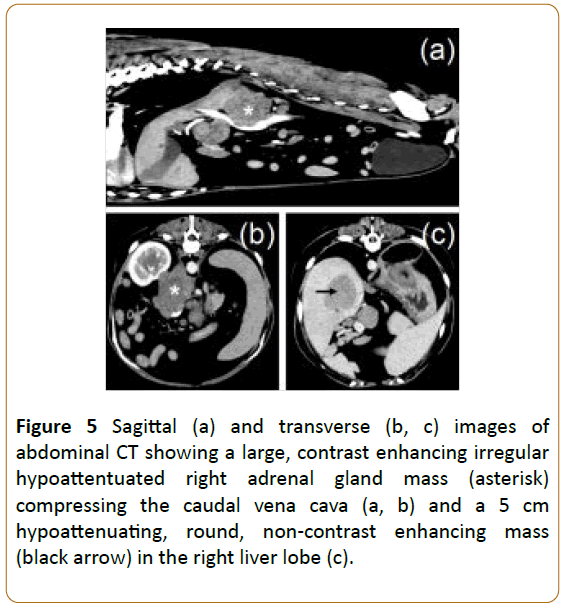
A systemic workup, including lab work and imaging studies, was recommended based on the patient’s history of CLL and the suspected left-sided retrobulbar mass. The complete blood count was unremarkable, while serum biochemistry profile showed mild liver enzyme elevations (alanine aminotransferase: 169; reference interval: 24-90; alkaline phosphatase: 350; reference interval: 20-150), mild hypoproteinemia (2.6; reference interval: 2.7-4.0), and mild decrease in BUN (6; reference interval: 10-30). Urinalysis showed trace proteinuria but was otherwise unremarkable. Lymph node measurements and fine needle aspirates were normal. Three view thoracic radiographs were within normal limits. Ultrasound of the left orbit with a linear 15 MHz probe revealed an approximately 8 mm, bilobed vascular mass in the ventromedial orbit causing indentation of the sclera medially (Figure 2). The anterior chamber OS was filled with an amorphous, echogenic material. A skull computed tomography (CT) showed left-sided exophthalmos due to an elongated soft tissue attenuating mass closely associated with the ventromedial aspect of the left globe (Figure 3a). The mass was seen extending medially and ventrally from the medial anterior chamber into the wall of the orbit. Additionally, severe left rostral mandibular bony lysis from tooth 304 to 309 was noted (Figure 3b). An approximately 7 cm right adrenal mass was observed on abdominal ultrasound (Figure 4) and CT (Figures 5a and 5b) dissecting into the caudal vena cava. Abdominal CT further revealed a 5 cm hypoattenuating, round, non-contrast enhancing mass in the right liver lobe (Figure 5c), enlargement of several abdominal lymph nodes (mesenteric, kidney, and left medial iliac), wedge-shaped filling defects in the right kidney, and soft tissue nodules in the dorsal body wall fat. Given these imaging findings, including the ocular/orbital mass, the left rostral mandibular lysis, the liver nodules, the multifocal peritoneal lymphadenopathy, and soft tissue nodules, disseminated lymphoma was considered a top differential. Due to the possibility of the adrenal mass being a pheochromocytoma, an electrocardiogram and systolic blood pressure via Doppler were performed once the patient recovered from general anesthesia. The patient’s heart rhythm and blood pressure were normal and recovery from anesthesia was uneventful.
Figure 2: Ocular ultrasound of the left eye and orbit with a 15 MHz linear probe (a) Dopper (b) showing an approximately 8 mm, bilobed vascular mass in the ventromedial orbit causing indentation of the sclera medially.
Figure 3: Transverse (a) and dorsal (b) images of skull CT showing left exophthalmos due to a soft tissue mass as well as left mandibular bony lysis.
Figure 4: Abdominal ultrasound revealed a large right adrenal mass (white arrows) dissecting into the caudal vena cava (asterisk).
Figure 5: Sagittal (a) and transverse (b, c) images of abdominal CT showing a large, contrast enhancing irregular hypoattentuated right adrenal gland mass (asterisk) compressing the caudal vena cava (a, b) and a 5 cm hypoattenuating, round, non-contrast enhancing mass (black arrow) in the right liver lobe (c).
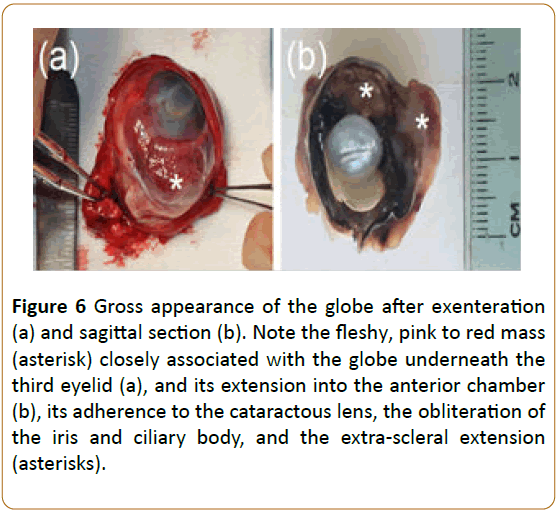
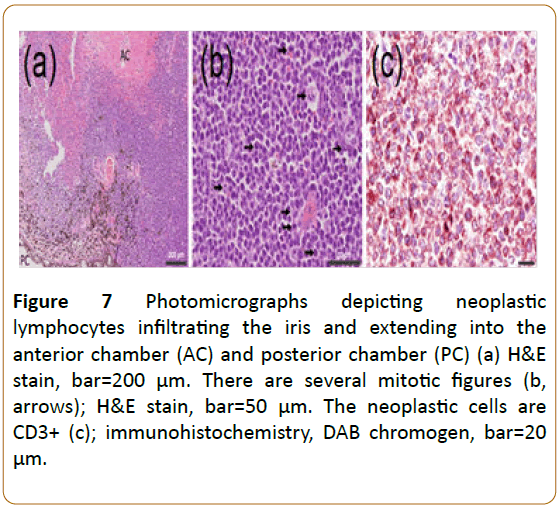
Five days later, surgical removal of the left eye and associated mass was requested by the owner for diagnostic and palliative benefits. Upon re-examination of the left eye, an ovoid 7 mm area of dense cellular infiltrate could be appreciated in the axial cornea. The patient was blood typed and cross matched prior to surgery. Fine-needle aspirates of the mandibular lesion were obtained under general anesthesia and showed a monoclonal population of medium to large lymphocytes consistent with a diagnosis of lymphoma. The left eye and orbital contents were surgically removed (exenteration) and the patient recovered uneventfully from anesthesia. Grossly, examination of the exenterated tissue revealed a fleshy, pink to red mass closely associated with the globe under the inner aspect of the third eyelid (Figure 6a). On sagittal section, the mass extended through the sclera and into the anterior segment of the globe, effaced the ventral anterior uvea (iris and ciliary body), filled much of the anterior chamber, and was adherent to the cataractous lens (Figure 6b). Histologically, the mass was composed of sheets of large, atypical lymphocytes (Figure 7a), with roughly 40 mitotic figures in 10X and 400X fields (Figure 7b). Neoplastic round cells were also noted in the anterior chamber, iris, choroid, vitreous, and posterior episclera. Immunohistochemistry showed a CD3+/CD20- homogenous population of cancerous cells, indicating T-cell lineage (Figure 7c). The final histopathologic diagnosis was large cell, high grade T-cell lymphoma. Secondary diagnoses included severe intraocular hemorrhage, cortical cataract, segmental retinal detachment, and severe, neutrophilic keratitis with Descemet’s membrane rupture.
Figure 6: Gross appearance of the globe after exenteration (a) and sagittal section (b). Note the fleshy, pink to red mass (asterisk) closely associated with the globe underneath the third eyelid (a), and its extension into the anterior chamber (b), its adherence to the cataractous lens, the obliteration of the iris and ciliary body, and the extra-scleral extension (asterisks).
Figure 7: Photomicrographs depicting neoplastic lymphocytes infiltrating the iris and extending into the anterior chamber (AC) and posterior chamber (PC) (a) H&E stain, bar=200 μm. There are several mitotic figures (b, arrows); H&E stain, bar=50 μm. The neoplastic cells are CD3+ (c); immunohistochemistry, DAB chromogen, bar=20 μm.
The day following the exenteration, the owner commented that the dog appeared to be non-painful, was more energetic, and had a good appetite. Unfortunately, the improvement was short-lived as the owner elected humane euthanasia two days after surgery due to rapidly declining systemic health. A necropsy was offered but declined.
Discussion
This report describes RS in a dog in which previously diagnosed T-cell CLL manifested as high-grade ocular T-cell lymphoma. It is unique as (i) an ocular manifestation of RS has not been previously documented in dogs, and (ii) the phenotype of lymphoma was T-cell whereas most cases are described in the human and veterinary literature are B-cell [2,4]. In fact, to the authors’ knowledge, only one report in humans documents the transformation of T-cell CLL to high grade T-cell lymphoma [1].
Richter’s syndrome is rare in veterinary medicine. To date, it has only been reported in 10 dogs [3-5] and no other veterinary species. Of those 10 dogs, none had an ocular manifestation of lymphoma as described in the present report. Most dogs had B-cell phenotype CLL, although, two-thirds of canine CLL have a T-cell phenotype [4]. In a recent review of canine leukemia, 6 of 22 CLL cases developed RS secondary to their B-cell CLL, or about 27% [4], which represents a similar percentage of RS development in human patients with a B-cell phenotype (2 to 20%) [2]. In this same study, 2 of 22 dogs (9%) developed T-cell RS [4]. Dogs with RS display clinical signs similar to humans including fever, weight loss, lymphadenopathy, and abdominal pain. Complete blood counts often reveal anemia, lymphopenia, and thrombocytopenia. Sadly, these patients deteriorate rapidly, and their median survival time in one report was only 41 days [5].
This dog’s ocular manifestation of RS is unique, and many of the clinico-pathologic findings were like human ocular cases including neoplastic round cell invasion of the orbit [6], sclera [7], iris [8], ciliary body [8], choroid [7,8], and vitreous [9,10]. Neoplastic round cells were also seen in the anterior chamber of this dog’s left eye. Of note, this canine patient had CD8+ T-cell CLL diagnosed 1.5 years prior to the development of high grade CD3+/CD20- T-cell ocular lymphoma. This combination of T-cell CLL to high grade T-cell lymphoma is rare and has been only been documented once in the human literature [1].
Richter’s syndrome, or Richter syndrome, is a clinico-pathologic term used to describe the development of aggressive lymphoma in patients with CLL. The first description was noted by Maurine Richter in 1928, who reported rapid decompensation in a CLL patient, following the development of lymphadenopathy and hepatosplenomegaly [11]. RS refers to either the transformation of CLL into a high-grade form of lymphoma, or the development of lymphoma as a secondary, independent cancer in a patient with CLL. The syndrome has been cited to occur in up to 20% of human patients with CLL, of which the majority suffer from classic, or transformative, RS [1,12]. It has been linked to immune-suppressed CLL individuals obtaining a viral infection, such as Epstein-Barr virus, or having underlying genetic defects [13-15]. The role or causative relationship between Epstein-Barr and Richter’s transformation has yet to be elucidated [13]. Clinically, human RS patients present febrile with progressive lymphadenopathy and elevated serum lactate dehydrogenase, with no systemic evidence of infection [14]. Often their blood count abnormalities (anemia, neutropenia, thrombocytopenia) are thought to occur secondary to their CLL [13]. Retroperitoneal lymphadenopathy, splenomegaly, and hepatomegaly are common, and patients often complain of abdominal pain [16]. Diagnosis is confirmed via biopsy of an affected organ coupled with the history of CLL. Unfortunately, these patients deteriorate rapidly and mean survival time is cited as merely 6 months with conventional chemotherapy [17]. Extranodal RS in humans has been reported to occur in bone, bronchi, the central nervous system, the gastrointestinal system, nose, skin, face and testis [18-20]. To the authors’ knowledge, there are only 7 reports of extranodal RS affecting ocular or periocular tissue in humans. These include vitreal and subretinal RS [9,10], panuveal (iridal, ciliary body, choroidal) RS [8], choroidal with scleral extension RS [7], and 3 cases of orbital RS [6].
The major limitation of this case report is the lack of necropsy confirming lymphoma in the abdomen. While it is presumed that disseminated lymphoma affected multiple abdominal organs as seen with CT (right adrenal, liver, mesenteric lymph nodes, body wall), samples of these organs were not obtained. Instead, the results of aspirates from the area of mandibular lysis and biopsy of the ocular tissues were used to confirm the diagnosis of high grade CD3+ T-cell lymphoma. A diagnosis of RS was made based on the dog’s documented history of CD8+ T-cell CLL, coupled with the clinical findings of weight loss, fever without evidence of infection, unremarkable complete blood count, abdominal lymphadenopathy, hepatomegaly, and extranodal ocular tissue expansion with T-cell lymphoma. It is unclear, however, if this dog’s condition represents the transformative type of RS, or RS due to dual, independent leukemia and lymphoma cancers.
This report describes an unusual presentation of suspect RS in a canine patient previously diagnosed with T-cell CLL. Although rare, given the possibility of CLL transforming into an aggressive, lymphoblastic lymphoma, RS should be a differential for any canine patient previously diagnosed with CLL presenting with acute ocular clinical signs.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Acknowledgements
This work was presented at the 2018 American College of Veterinary Ophthalmologists Annual Meeting in Minneapolis, MN in poster form.
References
- Matutes E, Wotherspoon RC, Parker NE, Osuji N, Isaacson PG, et al. (2001) Transformation of T-cell large granular lymphocyte leukaemia into a high-grade large T-cell lymphoma. Brit J of Haematol 115: 801-806.
- Jamroziak K, Tadmor T, Robak T, Polliack A (2015) Richter syndrome in chronic lymphocytic leukemia: updates on biology, clinical features and therapy. Leukemia Lymphoma 56: 1949-58.
- Leifer CE, Matus RE (1986) Chronic lymphocytic leukemia in the dog: 22 cases (1974-1984). J Am Vet Med A 189: 214-217.
- Comazzi S, Martini V, Riondato F, Poggi A, Stefanello D, et al. (2015) Chronic lymphocytic leukemia transformation into high-grade lymphoma: a description of Richter's syndrome in eight dogs. Vet Comp Oncol 15: 366-373.
- Comazzi S, Aresu L, Marconato L (2015) Transformation of canine lymphoma/leukemia to more aggressive diseases: anecdotes or reality? Front Vet Sci 2: p42.
- Kiratli H, Tarlan B, Uzun S, Tanas O, Uner A (2013) Orbital richter syndrome. Orbit 32: 381-383.
- Lee R (2012) Ocular lymphoma with extrascleral extension as primary manifestation of Richter syndrome. Eye 26: 890-891.
- JFernandez-Suntay P, Gragoudas ES, Ferry JA, Anderson ME, Dacey MP et al. (2002) High-grade uveal B-cell lymphoma as the initial feature in Richter syndrome. Arch Ophthalmol 120: 1383-1385.
- Kaplan HJ, Meredith TA, Aaberg TM, Keller RH (1980) Reclassification of intraocular reticulum cell sarcoma (histiocytic lymphoma). Immunologic characterization of vitreous cells. Arch Ophthalmol 98: 707-710.
- Hattenhauer MG, Pach JM (1996) Ocular lymphoma in a patient with chronic lymphocytic leukemia. Am J Ophthalmol 122: 266-268.
- Richter MN (1928) Generalized reticular cell sarcoma of lymph nodes associated with lymphatic leukemia. Am J Pathol 4: 285-292.
- Foresti V, Confalonieri F(1984) Richter's syndrome. Presentation of a rare variant with regression of chronic lymphatic leukemia and review of the literature. Minerva Med 75: 2741-2749.
- Tsimberidou AM, Keating MJ (2005) Richter syndrome: biology, incidence, and therapeutic strategies. Cancer 103: 216-228.
- Swords R, Bruzzi J, Giles F (2007) Recent advances in the diagnosis and therapy of Richter's syndrome. Med Oncol 24: 17-32.
- Tsimberidou AM, Keating MJ (2006) Richter's transformation in chronic lymphocytic leukemia. Semin Oncol 33: 250-256.
- Harousseau JL, Flandrin G, Tricot G, Brouet JC, Seligmann M, et al. (1989) Malignant lymphoma supervening in chronic lymphocytic leukemia and related disorders. Richter's syndrome: a study of 25 cases. Cancer 48: 1302-1308.
- Yee KW, O'Brien SM, Giles FJ (2005) Richter's syndrome: biology and therapy. Cancer J 11: 161-174.
- Omoti CE, Omoti AE (2008) Richter syndrome: a review of clinical, ocular, neurological and other manifestations. Br J Haematol 142: 709-716.
- Houdelette P, Dumotier J, Hauteville D, Pierre C, Berthod N (1989) Richter's syndrome with testicular localization. J Urol (Paris) 95: 507-508.
- Jha B, Dass J, Sachdev R, Bhargava R (2014) Testicular swelling: a rare manifestation of chronic lymphocytic leukemia presenting with Richter's syndrome. Indian J Pathol Micro 57: 133-135. Matutes E, Wotherspoon RC, Parker NE, Osuji N, Isaacson PG, et al. (2001) Transformation of T-cell large granular lymphocyte leukaemia into a high-grade large T-cell lymphoma. Brit J of Haematol 115: 801-806.