Arif Al-Nooryani1*, Wael Elabbassi1, Marija Markovic1, Milan Dobric2,3 and Branko Beleslin2,3
1Al Qassimi Hospital, Sharjah, United Arab Emirates
2Clinic for Cardiology, Clinical Center of Serbia, Belgrade, Serbia
3School of Medicine, University of Belgrade, Belgrade, Serbia
*Corresponding Author:
Arif Al Nooryani
Al Qassimi Hospital, Sharjah - United Arab Emirates
Tel: +97165188283
E-mail: arif345@yahoo.com
Received Date: November 07, 2015 Accepted Date: November 09, 2015 Published Date: November 15, 2015
Keywords
Robotic assistance, Percutaneous coronary intervention, Bioresorbable vascular scaffolds
Case presentation
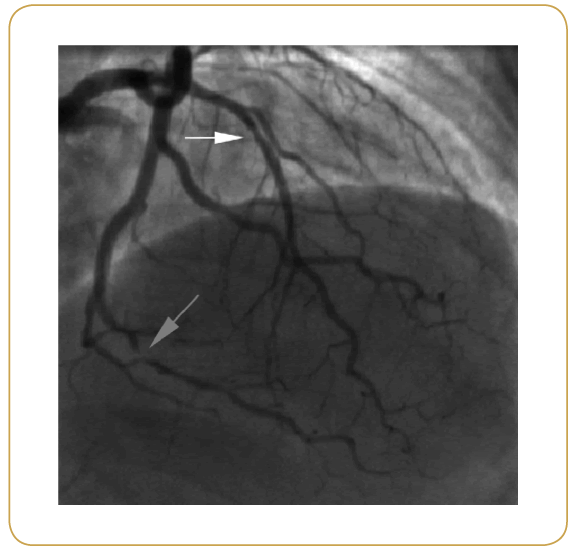
A 69 years old lady, with history of hypertension, dyslipidemia, diabetes treated with oral hypoglycemic, and coronary artery disease, presented with unstable angina. She first presented with stable angina 6 years ago which was treated successfully by balloon angioplasty on diagonal branch of left coronary artery. After that, she remained angina free until current admission. She had normal global left ventricular function without segmental wall motion abnormalities. Coronary angiography revealed two-vessel disease with short 50-70% stenosis of the mid left anterior descending (LAD) artery, 90% stenosis of the posterior descending artery (PDA) originating from dominant circumflex (Cx), and 50% stenosis of the first obtuse marginal (OM1) branch (Figure 1). SYNTAX score for this patient was 10, and we decided to proceed with PCI to PDA, using robotic-assisted approach (CorPath®, Corindus Vascular Robotics, Waltham, Massachusetts, USA), with further PCI of LAD and/or OM1 after physiological and morphological evaluation of lesion severity using fractional flow measurement (FFR; PresureWire™ Aeris™, St. Jude Medical, Saint Paul, Minnesota, USA) and optical coherence tomography (OCT; Dragonfly™ Duo, St. Jude Medical, Saint Paul, Minnesota, USA).
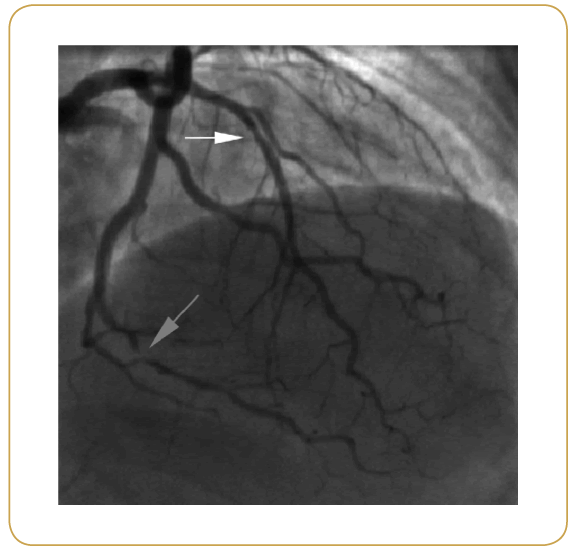
Figure 1:
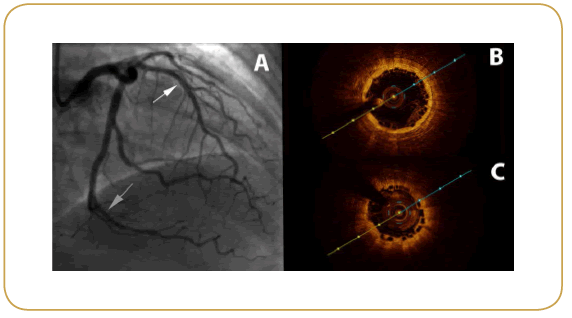
After selective cannulation of the left main (6F EBU guiding catheter), we have evaluated functional significance of intermediate stenosis of LAD and OM1 branch which appeared to be 0.76 for LAD and 0.91 for ostial OM1 branch. Minimal luminal area measured by OCT was 1.7 mm2 for mid LAD lesion. From this point of intervention, all coronary wires (floppy wires and PressureWire™), balloons and bioresorbable vascular scaffolds (BVS) were navigated through coronary arteries using roboticassistance.
Mid LAD artery lesion was predilated with 3.0 × 15 mm balloon, followed by BVS implantation (Absorb 3.0 × 18 mm, Abbott Laboratories, Illinois, USA) at 12 atmospheres, and BVS postdilatation with 3.25 × 10 mm non-compliant balloon (Figure 2A, white arrow) at 18 atmospheres. BVS was advanced by robotic navigation and tracking that underwent successfully and without any manual corrections. OCT, after BVS implantation, showed good BVS expansion and wall apposition (Figure 2B).
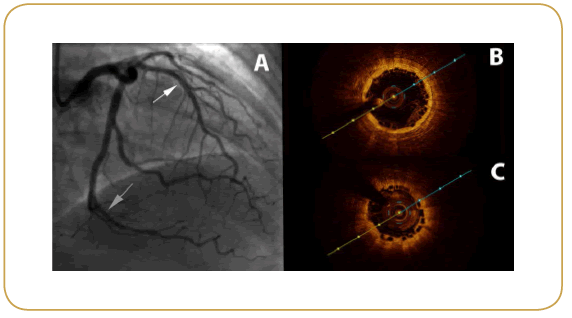
Figure 2:
Coronary wire manipulation, advancement and fine positioning of all balloons and BVS through long and tortuous distal Cx/ PDA was performed by robotic-assistance. PDA lesion was predilated with 2.0 × 15 mm balloon, followed by Absorb 2.5 × 28 mm implantation at 10 atmospheres. BVS was subsequently postdilated by non-compliant balloons 2.5 × 20 mm and 2.75 × 15 mm at 20 atmospheres (Figure 2A, gray arrow). Final OCT showed good BVS expansion and wall apposition (Figure 2C).
Hospital course was uneventful, and the patient was discharged from the hospital in good condition with following medications: perindopril 5 mg, amlodipine 5 mg, bisoprolol 5 mg, rosuvastatin 10 mg, aspirin 100 mg, and clopidogrel 75 mg (all medications once daily). The patient did not have any chest pain or other clinical events during nine months follow-up.
Total of 280 ml of contrast and 32 minutes of fluoroscopy was used for the entire procedure, and the radiation dose was 3900.7 mGy.
Discussion
Robotic-assisted angioplasty systems has been developed in order to overcome procedural challenges and occupational hazards (exposure to ionizing radiation, orthopedic injuries resulting from wearing shielding aprons, and fatigue from standing for hours) associated with traditional PCI [1-3].
First-in-human experience in remote-control PCI was reported in 2006 by Beyar et al. using Remote Navigation System (RNS, NaviCath, Haifa, Israel) [4]. In population of 18 treated patients, they reported technical success of 94% for the guidewire and 83% for the overall procedure. This system underwent a series of modifications culminating in the present CorPath® system (Corindus Vascular Robotics, Natick, MA) [2,3]. Initial experience with CorPath® robotic system was reported in 2011 in series of 8 patients, where the authors demonstrated system feasibility and safety, and procedural effectiveness that was comparable to manual operation [1]. Furthermore, total operator exposure to radiation was 97% lower than at the procedure table, with a mean fluoroscopy time of 11.5±3.7 minutes in their single lesion PCI population.
Following this initial experience, only few reports were published on robotic-assisted PCI which is probably due to limited experience worldwide with these devices. The largest published trial on robotic-assisted PCI was PRECISE (Percutaneous Robotically- Enhanced Coronary Intervention) study by Weisz et al. [5]. The trial enrolled 164 patients scheduled for PCI of single vessel. PCI was completed successfully without conversion to manual procedure, device technical success was achieved in 162 of 164 patients (98.8%), and radiation exposure for the primary operator was 95.2% lower than the levels found at the table position.
Data on complex and multivessel PCI performed using roboticassistance is scarce. Kapur et al. recently reported a series of four patients with complex lesions treated by robotic-assisted PCI (multiple lesions in single coronary artery, multivessel disease, vein graft, acute myocardial infarction) [6]. Dominguez et al. demonstrated that robotic-assisted PCI could be used to treat complex coronary lesions including type C lesions, saphenous vein graft lesions, chronic total occlusions, multilesion or multivessel disease, and also via the radial approach [7].
Initial criticism of robotic-assisted approach was directed toward presumed increased radiation exposure to the patient and increased use of contrast media. Recently published data demonstrated that robotic-enhanced PCI was not associated with increased fluoroscopy duration, radiation, or contrast media exposure to patients, and compared favorably to the traditional approach [8]. Furthermore, robotic-assisted PCI has a very steep learning curve, as it is demonstrated that experience gained after only 3 cases is associated with reduced procedure duration and reduced radiation afterwards [9].
To the best of our knowledge, this is the first reported case of robotic-assisted PCI utilized in the case where comprehensive physiologic (FFR) and intravascular morphologic (OCT) assessment was used to govern complete functional myocardial revascularization. Also, this is the unique case of PCI using bioresorbable vascular scaffolds by robotic-assisted angioplasty system, emphasizing the feasibility of the robotic system in more robust BVS platforms.
We demonstrated that robotic-assisted angioplasty systems could be safely and effectively use to deliver novel bioresorbable scaffolds with more robust profile to different and tortuous coronary arteries achieving in this case complete myocardial revascularization.
References
- Granada JF, Delgado JA, Uribe MP (2011) First-in-human evaluation of a novel robotic-assisted coronary angioplasty system. JACC Cardiovascular interventions 4: 460-465.
- Carrozza JP (2012) Robotic-assisted percutaneous coronary intervention--filling an unmet need. Journal of cardiovascular translational research 5: 62-66.
- Smilowitz NR, Weisz G (2012) Robotic-assisted angioplasty: current status and future possibilities. Current cardiology reports 14: 642-646.
- Beyar R, Gruberg L, Deleanu D (2006) Remote-control percutaneous coronary interventions: concept, validation, and first-in-humans pilot clinical trial. Journal of the American College of Cardiology 47: 296-300.
- Weisz G, Metzger DC, Caputo RP (2013) Safety and feasibility of robotic percutaneous coronary intervention: PRECISE (Percutaneous Robotically-Enhanced Coronary Intervention) Study. Journal of the American College of Cardiology 61: 1596-1600.
- Kapur V, Smilowitz NR, Weisz G (2014) Complex robotic-enhanced percutaneous coronary intervention. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions 83: 915-921.
- Dominguez A, Reeves R, Bahadorani J, Patel M, Mahmud E (2014) Feasibility of complex robotic percutaneous coronary intervention. Transcatheter Cardiovascular Therapeutics (TCT). Washington TCT-148.
- Smilowitz NR, Moses JW, Sosa FA (2014) Robotic-Enhanced PCI Compared to the Traditional Manual Approach. The Journal of invasive cardiology 26:318-321.
- Weisz G, Smilowitz NR, Metzger DC (2014) The association between experience and proficiency with robotic-enhanced coronary intervention-insights from the PRECISE multi-center study. Acute cardiac care 16: 37-40.