- (2014) Volume 15, Issue 4
Jia Li1, Muhammad Wasif Saif2
1VA Connecticut Healthcare System, Yale Cancer Center. New Haven, CT, USA
2Tufts Cancer Center. Boston, MA, USA
Surgery remains the only curative treatment for pancreatic cancer; however, majority of patients present with advanced unresectable disease upon diagnosis. Treatment of nonmetastatic, locally advanced pancreatic cancer (LAPC) continues to require multidisciplinary bimodality or trimodality approach. Neoadjuvant therapies have been investigated for LAPC given its established role in other solid cancers such as breast cancer, gastric cancer, and rectal cancer. This strategy is now moving forward to management of potentially resectable disease as well. This meeting highlight focuses on recent updates on neoadjuvant therapy for both borderline resectable disease and potentially resectable disease. Abstracts #4120, #e15189, #e15226 and #TPS4158 will be discussed.
Chemoradiotherapy; Neoadjuvant Therapy; Pancreatic Neoplasms
Pancreatic cancer remains the 4th leading cause of cancer deaths in the United States with a 5-year survival rate of 6% [1]. The American Cancer Society estimated in 2014, about 46,420 people (23,530 men and 22,890 women) will be diagnosed with pancreatic cancer; about 39,590 will die from this disease in the United States [1].
Pancreatic cancer can be divided into three categories: resectable disease, locally advanced unresectable disease and metastatic disease. Only less than 20% of patients present with surgically resectable disease, surgery followed by adjuvant chemotherapy could offer a cure for this group although median overall survival (OS) was only 22.1 months with 5-year survival rate of 22.5% [2]. Approximately 40% of patients present with metastatic disease, palliative chemotherapy with gemcitabine, or combination therapy (gemcitabine/nab-paclitaxel, FOLFIRINOX) could be considered depending on patients’ performance status and preference. This group has a median OS of ranging from 6.8 months to 11.1 months [3-5]. The rest 40% of patients present with LAPC, currently no optimal or standard treatment is available; surgery alone is not a good option due to high probability of residual tumor at the surgical margin or in draining lymph nodes. Chemotherapy and radiation have been investigated in the neoadjuvant setting in an effort to improve local and distant tumor control [6].
LAPC is further categorized into two sub-groups: locally advanced unresectable and borderline resectable. The locally advanced unresectable tumor typically invades into critical structures such as celiac or superior mesenteric arteries (SMA). Despite of various clinical trials, this subgroup rarely derives sufficient response to allow complete surgical resection. Borderline resectable tumor usually abuts or encases major arteries or veins to a lesser degree, thus, there is a high likelihood of down staging disease after pre-operative therapy (or therapies) to achieve a subsequent margin-negative resection and long-term survival. Although surgery upfront is the standard of care for potentially resectable disease, the poor longterm outcomes following surgical resection and adjuvant chemotherapy have led investigators to explore whether neoadjuvant therapy plays a role in potentially resectable disease as well.
The optimal regimen for LAPC has not been established, enrollment of these patients on clinical trials is highly recommended. In practice, despite of lack of randomized phase III data, most institutions offer induction chemotherapy followed by chemoradiotherapy and subsequent attempt of surgical resection in fit patients [6-8].
Induction chemotherapy usually consists of single agent gemcitabine, gemcitabine in combination (gemcitabine/ oxaliplatin, gemcitabine /S-1), or FOLFIRINOX (FU, LV, irinotecan and oxaliplatin) [9-14]. Given the impressive objective response rates and encouraging efficacy results in the metastatic setting, combination therapies are expected to be more effective in achieving pathologic complete response and increasing complete resection rate, however, there are no adequately powered randomized trials comparing these regimens in LAPC yet.
Patients without disease progression after initial induction chemotherapy are usually recommended to receive concurrent chemoradiotherapy. Commonly used radiosensitizers include: gemcitabine at various dose ranging from 40mg/m2 twice weekly to 1000 mg/m2 weekly, infusional fluorouracil, or oral capecitabine (based upon rectal cancer data) [15-17].
Report from MD Anderson demonstrated encouraging results in using this approach, near 40% of patients with borderline resectable disease underwent marginnegative pancreatectomy after receiving neoadjuvant chemotherapy with or without chemoradiotherapy; mOS reached 40 months with 5-year survival rate of 40%. Results from other small single institutional studies are also supportive of this triple modality approach in treating LAPC [18].
Currently, there are no studies showing a survival benefit of incorporating neoadjuvant chemotherapy or chemoradiotherapy to potentially resectable disease. Both 5-FU based and gemcitabine based chemotherapy and/ or chemoradiotherapy were investigated in early phase trials or retrospective studies, however, results are not convincing, it remains unknown whether neoadjuvant chemotherapy and/or chemoradiotherapy achieved better outcomes than upfront surgery followed by adjuvant chemotherapy.
Several early phase trials have been conducted to investigate the role of neoadjuvant therapy for potentially resectable and borderline resectable diseases; large randomized phase III data are still greatly needed (Table 1).
A Phase II Study of Perioperative GTX Therapy with XELOX Combined with Radiotherapy for Patients with Resectable and Borderline-Resectable Pancreatic Adenocarcinoma
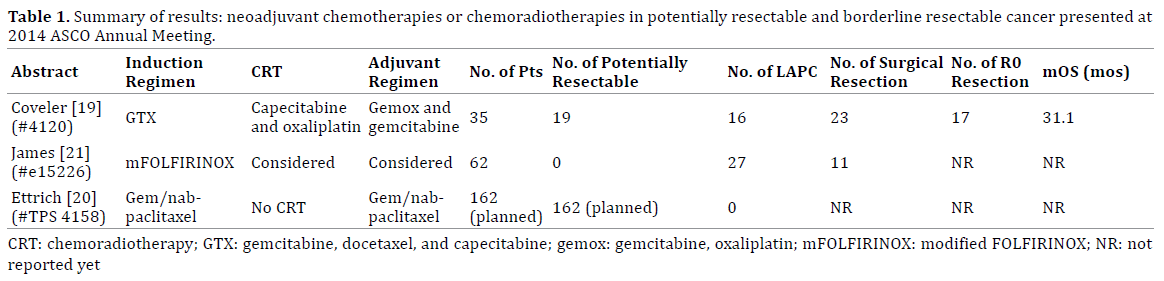
This trial enrolled 35 patients with 19 potentially resectable diseases and 16 borderline resectable diseases [19]. Neoadjuvant therapy includes induction chemotherapy with a combination of gemcitabine, docetaxel and capecitabine, followed by a 2-week course of concurrent chemoradiotherapy with capecitabine and oxaliplatin. Postoperatively, patients also received adjuvant chemotherapy consisting of gemcitabine/oxaliplatin and single agent gemcitabine. With this complicated neoadjuvant strategy, 31 out of 35 patients had surgery, among them 23 had surgical resection, 75% had R0 resection. Median OS for all comers was 31.1months, but for patients achieved surgical resection, mOS was not even reached yet. Certainly this perioperative triple modality approach is encouraging, large randomized trial is warranted to validate the exciting results, potentially include locally advanced unresectable disease as well. Unfortunately, based on this single arm study, we are not able to conclude that perioperative approach (induction chemo + chemoradiation + surgery + adjuvant chemo) is superior to standard of care with upfront surgery; especially half of the enrollment had potentially resectable disease.
NEONAX: Neoadjuvant plus Adjuvant or Only Adjuvant Nab-Paclitaxel plus Gemcitabine for Resectable Pancreatic Cancer - A Phase II Study of the AIO Pancreatic Cancer Group
Neonax is a phase II international study in an effort to address the role of neoadjuvant chemotherapy for potentially resectable disease [20]. The investigators chose the combination of gemcitabine/nab-paclitaxel based upon the favorable toxicity when compared with the other first-line FOLFIRINOX. This trial is planning to enroll 162 patients with potentially resectable disease. There will be no borderline resectable or locally advanced unresectable disease in this study. Planned treatment included either upfront surgery followed by 6 cycles of adjuvant gemcitabine/nab-paclitaxel or perioperative approach consisting 2 cycles pre-operatively and 4 cycles post-operatively.
Interim Analysis of a Phase II Study of Dose-Modified FOLFIRINOX (mFOLFIRINOX) in Locally Advanced (LAPC) and Metastatic Pancreatic Cancer (MPC)
A dose modified FOLFIRINOX in the setting of both locally advanced and metastatic pancreatic cancer was updated in the ASCO annual meeting [21]. This phase 2 trial enrolled 27 LAPC (including borderline resectable disease) and 35 metastatic diseases. All patients received 25% dose reduction of irinotecan and bolus FU, other agents’ dose was same as standard FOLFIRINOX. Neutropenia and vomiting were significantly decreased with this modified regimen, efficacy appears promising. More than 40% LAPC underwent surgery; prolonged survival is expected for this group of patients.
Prognostic Value of Serum Carbohydrate 19-9 in Patients Receiving Gemcitabine-Based Neoadjuvant Therapy for Pancreatic Cancer
Tumor marker CA 19-9 has been often used in clinical practice; however, its role as either diagnostic or prognostic is not well established. The purpose of this retrospective study is to investigate the prognostic role of CA 19-9 in the neoadjuvant setting [22]. This study included potentially resectable disease and locally advanced disease. After receiving gemcitabine based neoadjuvant therapy, patients with normalized CA 19-9 were found to have the high likelihood of undergoing surgical resection, and longterm survival.
These aforementioned studies are aiming to incorporate various chemotherapy and or chemoradiotherapy into the management of potentially resectable disease and locally advanced disease in order to improve resectability of tumors that may prolong overall survival. The results are promising, however, current studies are limited to early phase trials with small sample size or retrospective study from a single institution, and large randomized international studies are warranted to validate phase 2 results.
Despite advances in research, treating pancreatic cancer remains a challenge to both scientists and clinicians. As of now, there is no optimal neoadjuvant or perioperative therapy available, enrolling patients on appropriate clinical trials are highly recommended. Despite of lack of solid evidence from prospective studies providing survival benefit, most clinicians consider neoadjuvant chemotherapy with or without radiotherapy for locally advanced pancreatic cancer. Many early phase trials demonstrated a survival benefit with multidisciplinary strategy, the optimal chemotherapeutic agents, dosage and schedule are still in evolution.
The authors have no potential conflicts of interest.