Case Report - (2022) Volume 8, Issue 1
Rudimentary Horn Pregnancy- A Diagnostic Dilemma
Deeba Khanam*,
Seema Hakim and
Shweta Mhatre
Department of Obstetrics and Gynecology, Aligarh Muslim University, UP, India
*Correspondence:
Deeba Khanam, Department of Obstetrics and Gynecology, Aligarh Muslim University, UP,
India,
Tel: + 7895172183,
Email:
Received: 15-Dec-2021, Manuscript No. IPGOCR-21-12004;
Editor assigned: 17-Dec-2021, Pre QC No. IPGOCR-21-12004 (PQ);
Reviewed: 12-Jan-2022, QC No. IPGOCR-21-12004;
Revised: 19-Jan-2022, Manuscript No. IPGOCR-21-12004 (R);
Published:
26-Jan-2022, DOI: 10.21767/2471-8165.100001
Abstract
p>Pregnancy implanted in the rudimentary horn of unicornuate uterus is very rare with an incidence of 1 in 75,000 to 1 in 150,000 pregnancies and 50% of them rupture, while 80% of rupture occurs in first and second trimesters, where atrocious outcomes are reported. Horn pregnancy rarely reaches third trimester and when it does the diagnosis becomes more challenging. Ectopic in unicornuate rudimentary horn of uterus is difficult to diagnose even with best facilities available. Consequences are grave with slightest error of radiological and clinical judgment.
Here we report a case of a 20-year-primigravida with 34 weeks, IUD baby who reported to labor ward with pain lower abdomen. She was induced and in the process she went in to shock following which laparotomy was performed and per operatively we found ruptured rudimentary horn, and unilateral horn resection with salpingectomy was performed. The purpose is to spread awareness of all such rare cases where maternal and fetal well is jeopardized, and accentuates the significance of high index of suspicion in all such cases.
Keywords
Ectopic; Rudimentary horn; Mullerian anomaly; Rupture
Introduction
Mullerian anomalies were first classified in 1979 by Buttram
and Gibbons which was revised by the American Society of
Reproductive Medicine in 1988. Developmental deviations can
result in Unicornuate uterus with rudimentary horn [1-3]. ASRM
classification places unicornuate uterus in to type-2 classification
with unilateral hypoplasia or agenesis which is further classified
into communicating, non-communicating, no cavity and no horn
[4]. Its incidence is 2.4-13% of all the Mullerian anomalies [5].
72-85% of the rudimentary horns are non-communicating with
the cavity [6]. Various gynecological and obstetric complications
like infertility, hematometra, urinary tract anomalies, abortions,
preterm deliveries are associated with unicornuate uterus with
rudimentary horn. Pregnancy in a rudimentary horn is a very rare
condition with an incidence ranging from 1 in 75000 to 150000
pregnancies and results in uterine rupture 50-90% of the times
mostly by the end of second trimester [7,8]. Diagnosis is difficult
as majority of cases present in emergency with hemoperitoneum
in early trimesters. Here we report a case of ruptured rudimentary
horn pregnancy of 34weeks gestation which was misdiagnosed as
intrauterine pregnancy with fetal demise with abruption.
Case Presentation
20 years primi with 34 weeeks of gestation reported to the
emergency with chief complaints of labour pains since 6hours.
She came with a USG report showing intrauterine fetal demise of
34 weeks gestation. On general examination, her blood pressure
was 150/96 mm hg and pulse rate 110/min. Urine albumin was
traces. On per abdomen examination, uterine size was 30 weeks
and fetal heart sound was no localized. Uterus was tense and
tender. On per vaginal examination, OS was closed with uneffaced
cervix. No bleeding was seen. A diagnosis of abruption with fetal
demise was made and patient was induced with Tab Misoprost 50
microgm S/L 4 hourly according to bishops’ score with maximum
of five doses. After completion of five doses, Inj Syntocinon was
started 5 units @ 10 dpm and was titrated according to pains.
After 6 hours of syntocinon, patients’ blood pressure started
falling with tachycardia. USG guided tapping was done and blood
was aspirated from peritoneal cavity. Patient was immediately
shifted to OT for Laparotomy in view of rupture uterus.
Intraoperatively, around 1.5 L of hemoperitoneum was found
with left sided ruptured non- communicating rudimentary uterine
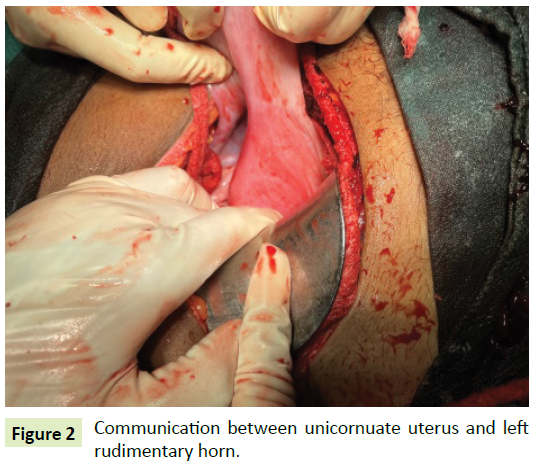
horn of a unicornuate uterus as shown in Figures 1 and 2 and intact sac with male fetus still lying inside the rudimentary horn.
The weight of the fetus shown in Figure 3 was 1.5 kilograms. The
left sided rudimentary horn was removed along with left sided
salpingectomy leaving left sided ovary intact as shown in Figure 4. After achieving homeostasis, abdomen was closed in layers and
drain was put in-situ. 3 units of PRBC and 2 units of FFP were
transfused. Patient was discharged on post-operative day 10 after
stitch removal in healthy condition.

Figure 1: Ruptured site over left rudimentary horn.
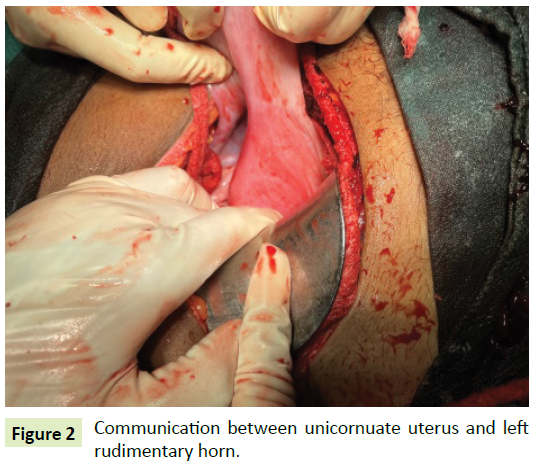
Figure 2: Communication between unicornuate uterus and left
rudimentary horn.

Figure 3: Male dead baby with skin peeling.

Figure 4: Resected left rudimentary horn with ruptured site.
Discussion
Failure of the complete development of one of the Mullerian
ducts and incomplete fusion with the contralateral side results
in the development of a rudimentary horn with a unicornuate
uterus. Mauriceau and Vassal in 1669 were the first to described
pregnancy in a rudimentary horn [9]. Pregnancy in a noncommunicating
rudimentary horn is rarely observed and is
thought to be due to transperitoneal migration of spermatozoan or fertilized ovum [10]. It is very rare to achieve a viable pregnancy
in such cases and most of them result in rupture of the horn in
first or second trimester of pregnancy [11]. Few cases reach
term and fetal salvage is only 2% [12]. Prior to rupture diagnosis
is difficult as sensitivity of USG to diagnose rudimentary horn
pregnancy is around 26%-30% which further decreases with the
advancement of pregnancy. In the present scenario the patient reported at 30 weeks but the scan could not diagnose it as a
rudimentary horn, and was induced which resulted in rupture
of the rudimentary horn. So the question is when to suspect a
rudimentary horn pregnancy? The present experience supports
the fact that any disproportionate pain in pregnancy should
always be thoroughly evaluated. A high index of suspicion should
be kept when a pregnant uterus does not respond to induction.
MRI should be considered whenever inconclusive diagnosis is
made on ultrasound [13-14]. A criteria for diagnosing pregnancy
in rudimentary horn was outlined by Tsafir A, et al. [13]. They
are: A) A pseudo pattern of asymmetrical bicornuate uterus,
B) Absent visual connective tissue surrounding the gestation
sac and the uterine cervix, C) Presence of myometrial tissue
surrounding the gestation sac. However only few cases are
diagnosed before rupture and mostly present as an emergency
with hemoperitoneum. Cases of false and late diagnosis have
also been reported. Rupture after use of misoprostol due to
misdiagnosis has been reported by Samuels TA and Awonuga A
[15]. A rudimentary horn pregnancy in 6th gravida was reported
by Buntungu KA, et al. [16] with all previous normal vaginal
deliveries.
Rudimentary horn pregnancy ultimately results in rupture
and the gestational age at which it ruptures depends on the
horn musculature and its distensibility, with 70-90% of rupture
occurring before 20 weeks of gestation [17]. Although cases
of pregnancy progressing to term and resulting in live birth
after cesarean section has been documented [11]. Bleeding in
rudimentary horn pregnancy rupture is more severe as uterine
wall is thicker and more vascular [18]. A rudimentary horn
pregnancy can also be complicated by placenta percreta with the incidence of 11.6% due to poorly developed musculature and the
small size of the horn [19]. Hence the morbidity associated with
it is very high.
Surgical removal is the primary strategy for managing rudimentary
horn. Edelman AB, et al. [20] reported successful management
of rudimentary horn pregnancy with methotrexate at an early
gestational age. But with medical management further horn
pregnancy cannot be prevented so mainstay is surgery [21].
However, in some cases with high resource setting, conservative
management was attempted until the viability was advocated
[22,23]. Prophylactic removal of non-communicating horn prior
to pregnancy to prevent complications is also advised. Renal
anomalies are associated in 36% of the cases; hence it is advised
to further investigate these women for renal anomalies [21].
Conclusion
Despite the advances in imaging and diagnostic modalities, the
antenatal diagnosis of rudimentary horn pregnancy is still difficult
for clinicians. Delayed diagnosis or misdiagnosis can worsen the
condition of the patient and golden period may be lost. All such
cases with varied presentations of rudimentary horn pregnancy
should be reported so that the clinicians are aware of atypical
clinical scenario and maternal and fetal morbidities are avoided.
A high index of suspicion for uterine anomalies should be made
in early gestations and also in cases with failed induction. Early
diagnosis of rudimentary horn pregnancy with early intervention
reduces the maternal morbidity and mortality. With a rudimentary
horn pregnancy, excision of the horn and ipsilateral salpingectomy
is the recommended surgical treatment.
REFERENCES
- Okonta PI, Abedi H, Ajuyah C, Omo-Aghoja L (2009) Pregnancy in a non-communicating rudimentary horn of a unicornuate uterus: A case report. Cases J 3: 6624.
Google Scholar
- Tufail A, Hashmi HA (2007) Ruptured ectopic pregnancy in rudimentary horn of the uterus. J Coll Physicians Surg Pak 17: 105-106.
Google Scholar, Indexed at
- Kanagal DV, Hanumanalu LC (2012) Ruptured rudimentary horn pregnancy at 25 weeks with previous vaginal delivery: A case report. Case Rep Obstet Gynecol 2012: 1-4.
Google Scholar, Crossref, Indexed at
- Hassan HC, Kadir A, Karim A, Ismail NAM, Omar MH (2011) Case report of ruptured non-communicating right rudimentary horn pregnancy: An acute emergency. Acta Medica 54: 125-126.
Google Scholar, Crossref, Indexed at
- Simon C, Martinez L, Pardo F, Tortajada M, Pellicer A (1991) Mullerian defects in women with normal reproductive outcome. Fertil Steril 56: 1192-1193.
Google Scholar, Crossref, Indexed at
- Sevtap HK, Aral AM, Sertac B (2007) An early diagnosis and successful local medical treatment of a rudimentary uterine horn pregnancy: A case report. Arch Gynecol Obstet 275: 297-298.
Google Scholar, Crossref, Indexed at
- Rackow BW, Arici A (2007) Reproductive performance of women with müllerian anomalies. Curr Opin Obstet Gynecol 19: 229-237.
Google Scholar, Crossref, Indexed at
- Akar ME, Bayar D, Yildiz S, Ozel M, Yilmaz Z (2005) Reproductive outcome of women with unicornuate uterus. Aust N Z Obstet Gynaecol 45: 148-150.
Google Scholar, Crossref, Indexed at
- Mauriceau F (1721) Traite des maladaies des femmes grosses. Compaigne des libraries Paris, France.
Google Scholar
- Scholtz M (1951) A full-time pregnancy in a rudimentary horn of the uterus. Int J Obstetr Gynaecol 58: 293-296.
Google Scholar
- Shin JW, Kim HJ (2005) Case of live birth in a non communicating rudimentary horn pregnancy. J Obstet Gynaecol Res 31: 329-331.
Google Scholar, Crossref, Indexed at
- Corte LD, Fabozzi A, Giampaolino P, Saccone G, Pizzuti LM, et al. (2019) A case of 20-week abortion in a rare communicating rudimentary horn of a misinterpreted unicornuate uterus, incorrectly diagnosed as bicornuate: A serious hazard! Eur J Obstet Gynecol Reprod Biol 235: 133-135.
Google Scholar, Crossref, Indexed at
- Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M (2005) Rudimentary horn pregnancy: First-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med 24: 219-223.
Google Scholar, Crossref, Indexed at
- Gaikwad V, Gite R, Deshpande HG, Pingle A, Puri M (2014) Rudimentary horn pregnancy-prerupture diagnosis and management. Med J Obstet Gynecol 2: 1042.
Google Scholar
- Samuels TA, Awonuga A (2005) Second-trimester rudimentary uterine horn pregnancy: Rupture after labor induction with misoprostol. Obstet Gynecol 106: 1160-1162.
Google Scholar, Crossref, Indexed at
- Buntungu KA, Ntumy MY, Ameh EO, Obed SA (2008) Rudimentary horn pregnancy: Pre-rupture diagnosis and management. Ghana Med J 42: 92-94.
Google Scholar, Crossref
- O’leary JL, O’leary JA. (1963) Rudimentary horn pregnancy. Obstet Gynecol 22: 371-374.
Google Scholar
- Chowdhury S, Chowdhury T, Azim E. Pregnancy in a non-communicating rudimentary horn of uterus: A clinical case report. Bangladesh Med J 39: 47-48.
Google Scholar, Crossref
- Jain R, Gami N, Puri M, Trivedi SS (2010) A rare case of intact rudimentary horn pregnancy presenting as hemoperitoneum. J Hum Reprod Sci 3: 113-115.
Google Scholar, Crossref, Indexed at
- Edelman AB, Jensen JT, Lee DM and Nichols MD (2003) Successful medical abortion of a pregnancy within a noncommunicating rudimentary uterine horn. Am J Obstet Gynecol 189: 886-887.
Google Scholar, Crossref, Indexed at
- Jayasinghe Y, Rane A, Stalewski H, Grover S (2005) The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 105: 1456-1467.
Google Scholar, Crossref, Indexed at
- Nahum G (2002) Rudimentary uterine horn pregnancy: the 20th century worldwide experience of 588 cases. J Reprod Med 47: 151-163.
Google Scholar, Indexed at
- Shin JW, Kim HJ (2005) Case of live birth in a non-communicating rudimentary horn pregnancy. J Obstet Gynaecol Res 31: 329-331.
Google Scholar, Crossref, Indexed at
Citation: Khanam D, Hakim S, Mhatre S (2022) In Gynaecologic Oncology, Research on Cancer Care Delivery is Being Conducted. Gynecol Obstet Case Rep. Vol.8 No.1:1.
Copyright: © Khanam D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.