Case Report - (2022) Volume 8, Issue 2
Saphenous Vein Graft Stenosis
Khuzeima Khanbhai1,2*,
Suhaila Bhimani1,
Jaison Chacko1,
Simon Peter1,
Abel Mussa1,
Hussein Hassanali1,
Peter Kisenge1,2,
Martha Mbona1,2 and
Sarah Matuja3
1Department of Cardiology, Saifee Hospital Tanzania, Tanzania
2Department of Cardiology, Jakaya Kikwete Cardiac Institute, Tanzania
3Internalmedicine Catholic University of Health and Allied Sciences, Tanzania
*Correspondence:
Khuzeima Khanbhai, Department of Cardiology, Saifee Hospital Tanzania,
Tanzania,
Email:
Received: 26-Jan-2022, Manuscript No. IPIC-22-12573;
Editor assigned: 28-Jan-2022, Pre QC No. IPIC-22-12573;
Reviewed: 11-Feb-2022, QC No. IPIC-22-12573;
Revised: 16-Feb-2022, Manuscript No. IPIC-22-12573;
Published:
23-Feb-2022, DOI: 10.21767/2471-8157.8.2.06
Abstract
Key clinical message: When used as conduits for coronary atery bypass surgery, saphenous vein grafts (SVG) develop
atherosclerotic disease that may result in stenosis or occlusion in 50% of patients by 10 years. SVG intervention
has become an attractive alternative to re operation in these patients, but also it is favourable with less acute and
long term outcomes compared with percutaneous coronary intervention (PCI) of native vessels. The potentional
of Drug Eluting Stents (DES) in improving long term results of SVG interventrtion is still debated and up to date
there is no clear evidence of benefit in relevant clinical end point, However a retrospective study conducted in italy
commented that the study they conduced supports the growing use of DES for SVG PCI by documenting safety and
reduced rates of restenosis and adverse cardiovascular events.
Introduction
Coronary artery disease (CAD) is a highly prevalent and initial
consensus disease afflicting many. The treatment of CAD ranges
from medical management and life style modification to
invasive coronary revascularization. Using of SVG has been ongoing
since 1967 because of an easy accessibility and reliability
conduit with significant length [1].
In most SVG the Great Saphenous vein (GSV) is utilized, however
in select circumstances the Short saphenous vein (SSV) may
be a suitable option [2].
SVG lesions are associated with a higher restenosis rate, particularly
in the proximal anastomotic (58%) and body (52%)
portions of the graft. Distal anastomotic narrowing responds
to angioplasty well, especially in patients with recurrent CABG
surgery [3]. The clinical patency of SVG In arterial circulation
can be divided into: Early (0 days-30 days); Short Term (30 days-24 month) and Long Term (More than 24 months).
In The United states, >300,000 patients undergo CABG each
year, Graft occlusion before discharge has been reported to occur
in approximately 10% of the Venous grafts. During the 1st year after CABG approximately 15%-30% occlusion has been
recorded and After 1 year Post CABG annual occlusion rate 2%
and it rises approximately 4% annually between post OP and
years 4 and 6 [4].
The Main causes of graft diseases are: During the Early Period-
Stenosis due to Technical issues occurring at graft anastomoses
eg. Position of graft, Kinking of graft, Poor distal runoff
which occurs in as many as 10% of total vein graft failure [5].
During the short Term period the possible causes of graft diseases
are perivascular myofibroblast remodeling, Platelet derived
growth factor, Smooth muscle Proliferation, decreased
local nitrogen oxide release, Decreased endothelial relaxation
and Initimal vein thickening. The Causes for Diseased graft at the long term phase are formation of atheroscelerosis with
plaque formation to adjacent areas of lipid deposition intimal
and hyperplasia [6].
Case Report
We report a case of a 68 year old male patient who was referred
for coronary angiography because of clinical presentation
of unstable angina for 5 days (CCS?) and a Positive Trop
leak of 1.613 ng/mL. He had a history of arterial hypertension,
hyperlipidemia, DM type 2, Cigarette smoking, parkinsonism
and coronary artery diseases post CABG in 2014 (8 years ago)
with LIMA to LAD, SVG to PDA and OM [7].
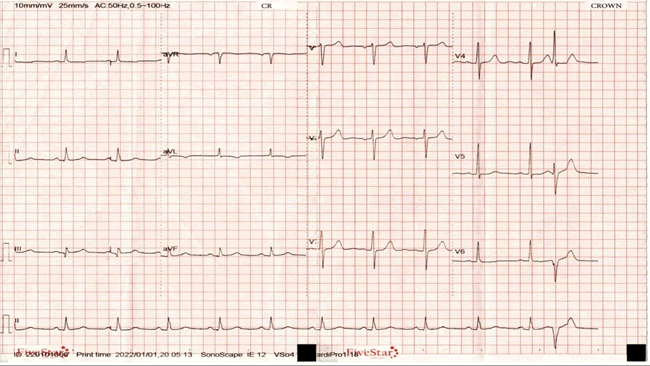
Electrocardiography showed a Premature Ventricular Complex
(PVC), T wave inversion in lead I and aVL (High Lateral Leads), Q
wave in lead III (Figure 1), Whereas Echocardiography revealed
No Regional wall motion abnormality with a EF of 60%, Mild to
Moderate Mitral Regurgitation, Moderate Aortic Regurgitation,
Mild Tricuspid Regurgitation, Mild Pulmonary Hypertension,
Concentric LVH [8].
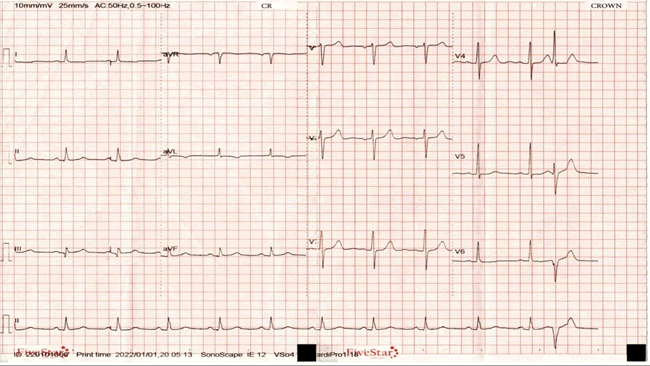
Figure 1: Electrocardiography
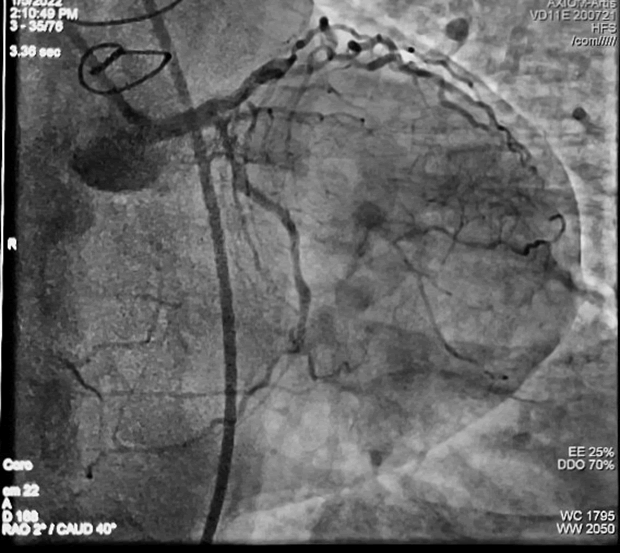
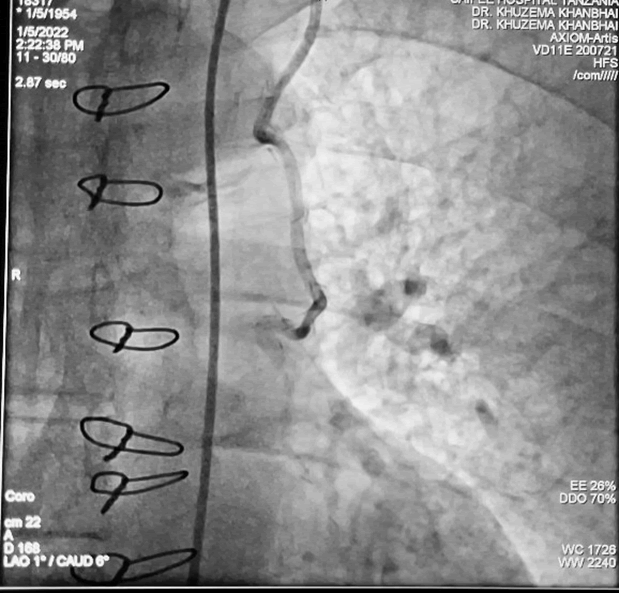
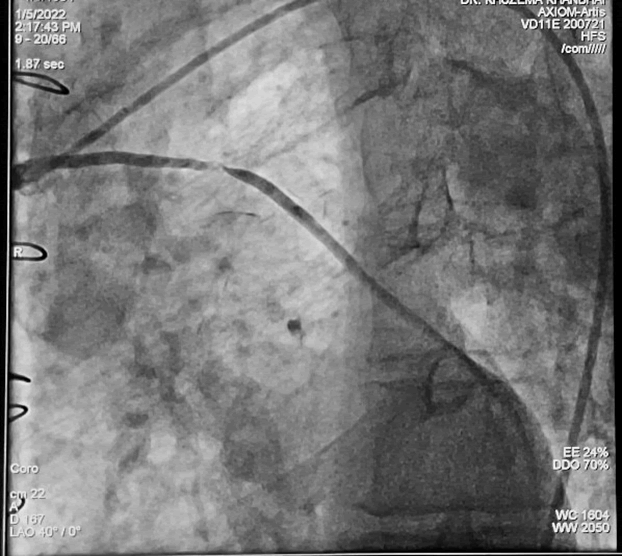
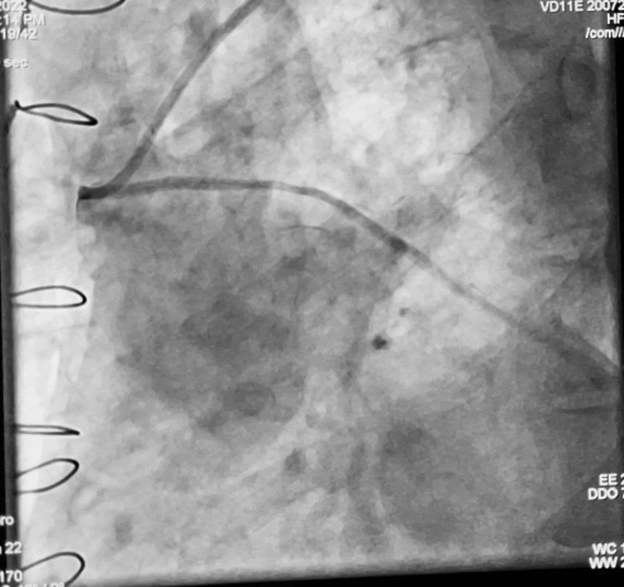
Coronary and Graft angiography showed a Normal Left Main
Coronary artery with a Patent LIMA with good distal runoff into
mid LAD artery and a retrograde flow into proximal LAD artery
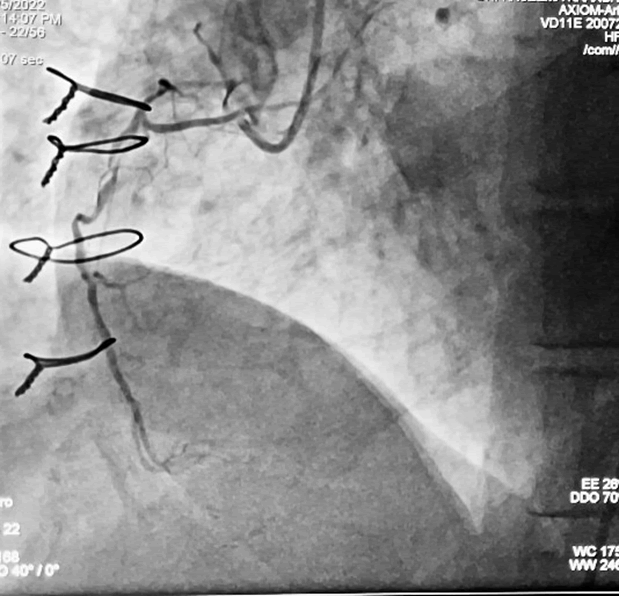
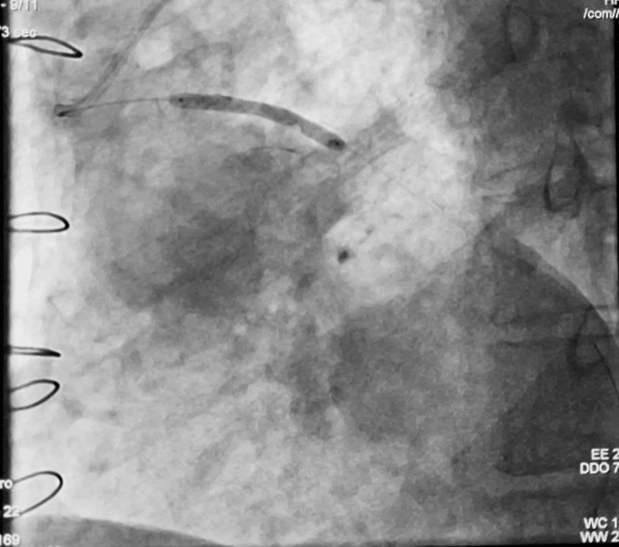
and LCX artery (Figures 2 and 3), Occlusion of the mid SVG to a
second OM branch and a patent to the PD branch of proximally
(Figure 4) [9].
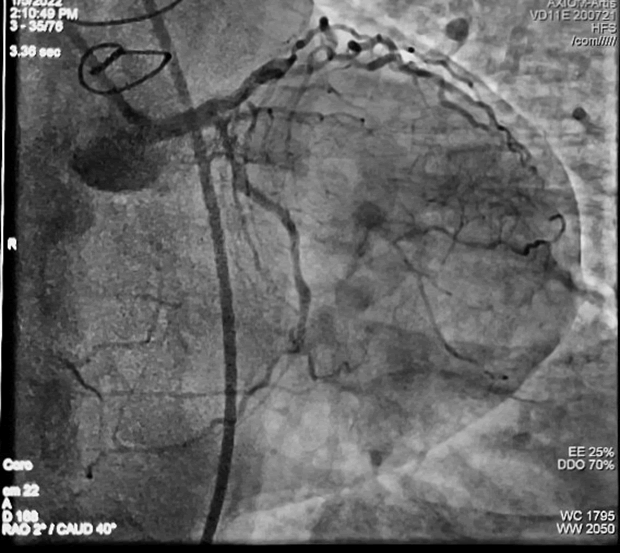
Figure 2: Coronary Angiography of Left Coronary Artery
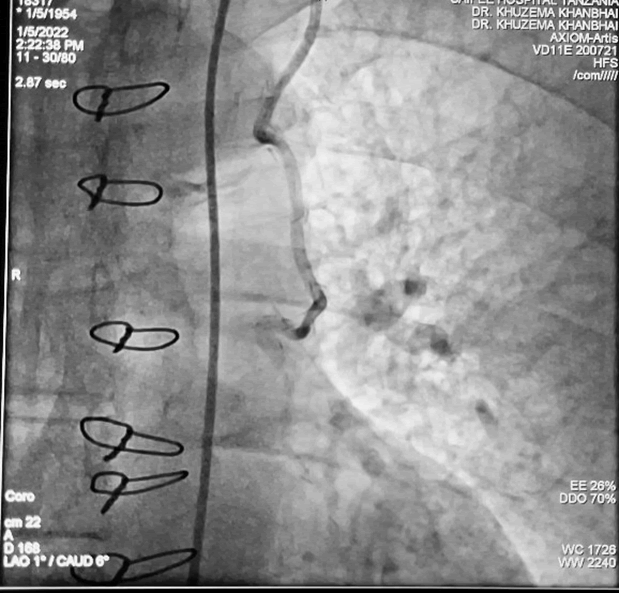
Figure 3: Angiography of LIMA
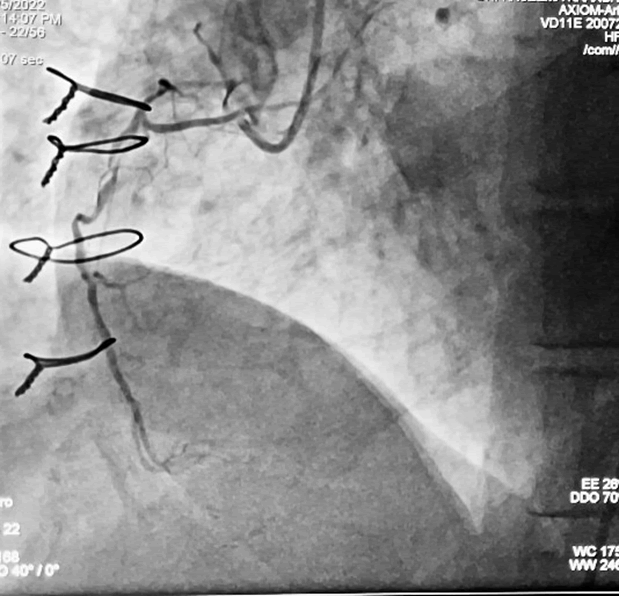
Figure 4: Coronary Angiography Right Coronary Artery
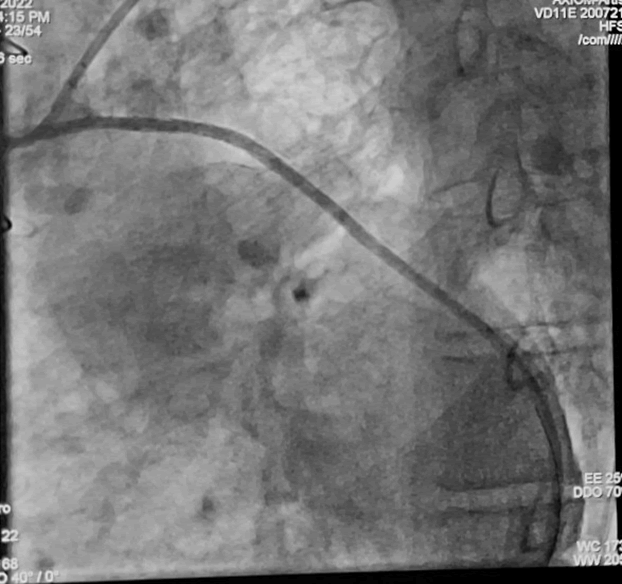
We proceeded with stent angioplasty of the Mid SVG lesion.
After low pressure predilation with BrosMed 2.5 x 15 mm Semi
complaint balloon (Figure 5), Treatment of the critical stenosis
of SVG-PDA and OM was successfully done using a 3.0 × 29 mm
Angiolite sirolimus and excellent angiographic result was obtained
(Figures 6 and 7). No reflow phenomenon was not observed
and final angipgraphy showed good dilation and patency
of the SVG with normal distal runoff into the Dg artery and
retrograde flow distribute to a large area of the anterior-lateral
wall [10] (Figures 8 and 9).
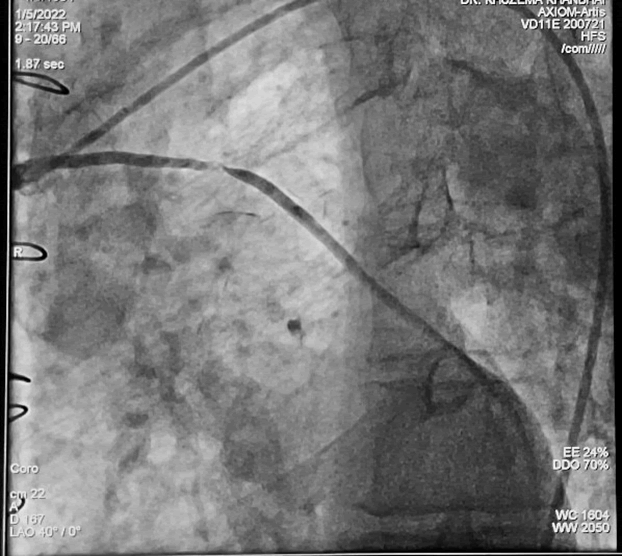
Figure 5: Angiography of SVG–Showing Mid SVG Stenosis

Figure 6: (Angio) Showing Ballooning (Pre Dilation) of Mid SVG
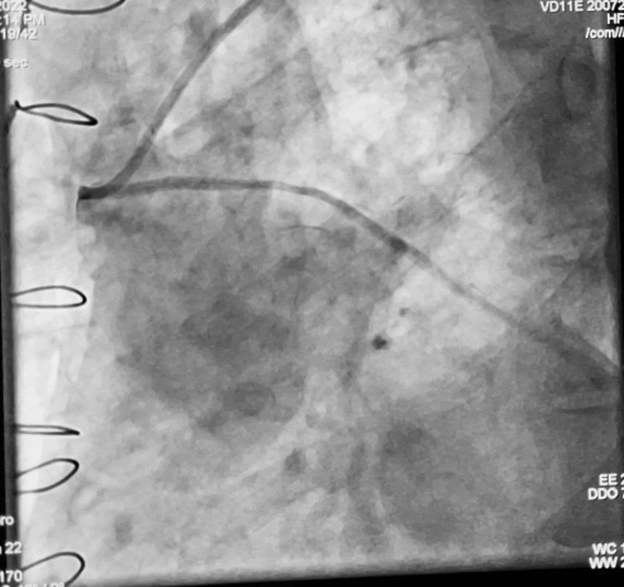
Figure 7: Post Ballooning (PRE Dilation) Flow
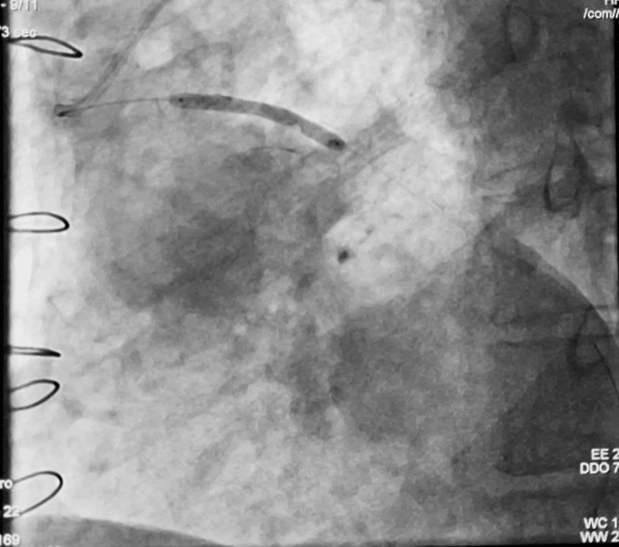
Figure 8: DES Placement at Mid SVG
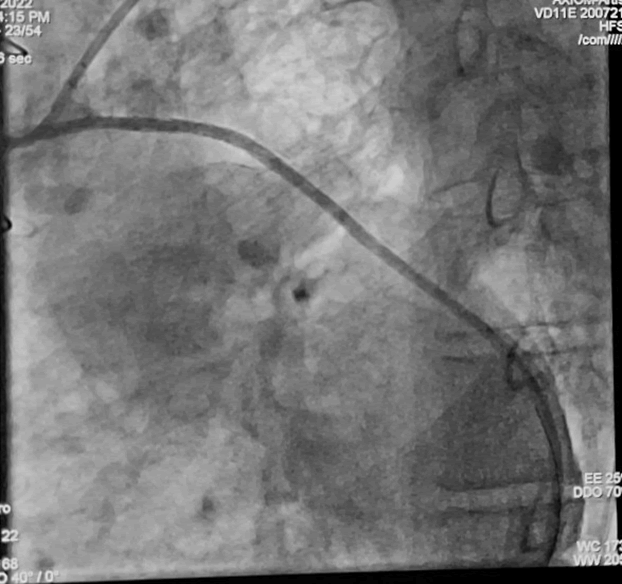
Figure 9: Post Stenting Flow of SVG
Post procedural patient was kept in ICU for observation and
then discharged 2 days later on dual antiplatelet therapy with
aspirin and clopidogrel, an Angiotensin converting enzyme inhibitor,
a beta blocker and a statin [11] (Table 1).
Table 1: Segment values.
| Vessel/segment % |
Ostial |
Proximal |
Mid |
Distal |
Timi flow |
| RCA |
90% |
95% |
90% |
50% |
Ii |
| LM |
Normal |
Normal |
Normal |
Normal |
Iii |
| LAD |
ECTASIA |
ECTASIA |
90% |
Total |
II |
| D1 |
10% |
10% |
MADINA 1,1,1 |
|
II |
| LCX |
ECTASIA |
20% |
40% |
ECTASIA |
II |
| OM2 |
90% |
70% |
95% |
TIMI II |
I |
| RAMUS |
SMALL BRANCH |
| LIMA |
Patent |
Patent |
Patent |
Patent |
Iii |
| SVG |
Patent |
Patent |
90% |
Patent |
Iii |
| LIMA |
Patent |
Patent |
Patent |
Patent |
Iii |
| SVG |
Patent |
Patent |
90% |
Patent |
Iii |
Discussion
Dynamic segmental compression of SVG rare, yet clinically relevant
angiographic finding [12]. Compared with native coronary
artery disease (CAD), vein graft lesions are frequently associated
with considerable plaque burden and intracoronary thrombus,
which increases the risk of peri-interventional adverse events.
In addition, a unique pathophysiology and histomorphology of
SVG lesions with typically friable degenerated plaques result in
a different vessel response to endoluminal interventions and a
high risk of debris embolisation. Finally, patients with diseased
SVGs frequently have additional conditions including advanced
age, more extensive atherosclerosis and reduced left ventricular
function, which predicts a worse outcome after peri-interventional
complications compared with ‘healthier’ patients;
thus, optimised approaches that minimise complications and
maximise the efficacy in patients undergoing vein graft PCI are of specific importance. Saphenous venous bypass grafts are often
used as conduits for CABG. However, ten years after CABG
only 60% of venous grafts remain patent [13].
Conclusion
Saphenous vein graft patency continues to be a significant
problem after CABG because only half of them are free of significant
stenosis. For revascularization after CABG, both surgical
and percutaneous methods have limitations. Percutaneous
coronary intervention (PCI) is recommended only if feasible,
mainly in patients with co-morbidities, left ventricular dysfunction,
lack of available saphenous veins, and in the elderly. SVG
stenting is an attractive alternative in patients without PCI option
in the native vessels. A greater interval between surgery
and SVG PCI reduces the technical success and is associated
with a higher rate of early complications and reduced long
term patency.
REFERENCES
- Sbarzaglia P, Notaristefano S, Cavallini C (2010) Best treatment of saphenous vein graft lesions; 1, 1-06156.
[Crossref] [Google Scholar] [Research Gate]
- Weintraub WS, Jones EL, Craver JM (1994) Frequency of repeat coronary by-pass or coronsary angioplasty after coronary artery bypass surgery using saphenous vein grafts, Am J Cardiol, 73(2): 103-12.
[Crossref] [Google Scholar] [Research Gate]
- Valdes PJ, Dorosh J, Lin JC (2021) vein graft stenosis.
[PubMed] [Google Scholar] [Research Gate]
- Andreas Y. Andreou (2016) A case of dynamic segmental saphenous vein graft compression during diastole.
[Crossref] [Google Scholar] [Research Gate]
- TH Christophides, G Georgious, K Yiangou (2009) Angiographic segmental narrowing of a saphenous vein bypass graft during diastolic, J Invasive cardio.E101-E102.
[PubMed] [Google Scholar] [Research Gate]
- Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, et al. (1996) Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 28 (3):616-26.
[Crossref] [PubMed] [Google Scholar]
- Sanz G, Pajarón A, Alegría E, Coello ICardona M, et al. ( 1990) Prevention of early aortocoronary bypass occlusion by low-dose aspirin and dipyridamole. Circulation. 82(3):765-73.
[Crossref] [PubMed] [Google Scholar]
- Weintraub WS, Jones EL, Morris DC (1997) Outcome of reoperative coronary bypass surgery versus coronary angioplasty after previous bypass surgery. Circulation.95(4):868-77.
[Crossref] [PubMed] [Google Scholar]
- Baim DS (2003) Percutaneous treatment of saphenous vein graft disease: The ongoing challenge.J Am Coll Cardiol.42(8):1370-72.
[Crossref] [PubMed] [Google Scholar]
- Gruentzig AR, Senning A, Siegenthaler WE (1979) Nonoperative dilatation of coronary artery stenosis. Percutaneous transluminal coronary angioplasty.N Engl J Med.301:61-8.
[Crossref] [PubMed] [Google Scholar]
- Henrique Murad (2020) Saphenous Vein Graft Stenosis. Arq Bras Cardiol.115(3):545-546.
[Crossref][PubMed] [Google Scholar]
- Jeffrey R. Alpert, Ernest J. Ring, Henry D. Berkowitz (1979) Treatment of vein graft stenosis by balloon catheter dilation. JAMA.242(25):2769-71.
[Crossref][PubMed] [Google Scholar]
- Guering Eid-Lidta, Jorge Gaspara, Alexander E. Adamesa, Félix Damas de Los Santosa (2010) Long-term outcomes of saphenous vein graft stenting compared with native coronary artery stenting in patients with previous coronary artery bypass graft surgery.Arch Cardiol Mex.80(1):3-9.
[PubMed] [Google Scholar] [Research Gate]
Citation: Khanbhai K, Bhimani S, Chacko J, Peter S, Mussa A, et al. (2022) Saphenous Vein Graft Stenosis. Interv Cardiol J. 8:06.
Copyright: © K Khanbhai, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited