Keywords
Family medicine; Family physician; 5-star doctor; Rural Bangladesh; Primary health care
Introduction
Globalization with consequent epidemiological transitions is the phenomena of the 21st century’s global health system. The emerging global burden of diseases could hardly be explained simply by organic lesions without taking into account the interactions among its socio-economic, demographic, political, technological and cultural determinants [1]. Moreover, the complex determinants of those diseases have been more complicated with concomitant inequity, inefficient cost and quality control and urban concentration of scarce human resources in healthcare [2,3]. The Primary Health Care (PHC) is one the proven cost-effective reform of global health system of combating the rising threats of globalized diseases at community level [4]. Family Medicine is gripping interests of academicians, researchers and policymakers of nations because of its recognized efficiency in achieving goals of PHC and ensuring inclusive patient-centered care. Thus, Family Medicine has been institutionalized in many countries in the world although it is still either in infancy or unrecognized in many developing countries [5,6]. Family Physicians are distinct medical professionals with postgraduate specialty [7]. However, status conflict among Family Physicians and other clinical specialist doctors challenges to promote and prospect of Family Medicine in many countries [8].
In Bangladesh, the private health market is growing rapidly in urban areas and majority of public facilities are rural-based. District* hospitals at the district headquarters and teaching/ specialized hospitals at megacities are the public secondary, tertiary/specialized curative facilities respectively. The PHC system consists of three-tier rural facilities: the Community Clinic (CC), Union Sub-Centre (USC) and Upazilla (subdistrict) Health Complex (UHC). The CCs and USCs provide outdoor and home-based primary care through paramedics and domiciliary staff which constitute about 63% of nearly 100,000 national health workforces. The UHCs are referral facilities of the PHC system with 50 bed capacity. UHCs have posts for graduate and specialist doctors (Ministry of Health and Family Welfare [9]. However, absenteeism and shortage of doctors at rural facilities make barrier to rural people’s access to healthcare [10].
Healthcare costs are a major concern of economic development of the country. In 2008/2009, nearly 67% total health expenditures (THE) was shared privately; of which, 96.5% was out-of-pocket payments (OPP). The rest 33% of was tax and donor sourced public contribution [11]. Resource shortage along with non-provision of health insurance forms an OPP-model of healthcare system which threatens health catastrophe. About 72% of over 150 million population of Bangladesh are rural residents; of them, about 35.2% live below the poverty line Bangladesh Bureau of Statistics [12,13]. Despite well-structured PHC system, universal health coverage has yet to be improved [14].
This study aims to promote the scopes of Family Medicine specialty for improving social, health and economic prospects at rural Bangladesh. To achieve this aim, a short description of the study methods will follow the findings on the emerging diseases burden especially of rural Bangladesh and the key health system factors influence medical students’ and doctors’ motivation and distribution with its impacts. Based on findings, the discussion section will describe priority healthcare needs, and evidence-based strategies of promoting Family Medicine and retaining doctors in rural communities. Lastly, conclusion and recommendations will be addressed.
Methods
The study is based on: literature review on health system structure and financing, and trends of morbidity and mortality with risk factors of priority diseases in rural Bangladesh and personal contacts with health professionals. Formal and informal searches were conducted during February 2015 on the websites of the MOHFW, WHO and World Bank. Snowballing strategy was also used for searching relevant articles. Google and Google Scholar were used as search engines.
The following eligibility criteria were used to recruit article: primary research, review articles and reports on Family Medicine practice, training, and education curriculum. After a quick screen through reading titles and abstracts of all the available articles, the full text of the primarily accepted literatures was skimmed to assess the applicability and quality for final inclusion. Applicability of the primarily accepted article was assessed based on inclusion criteria. Quality was assessed using ‘Critical Appraisal Skills Programme’ (CASP) criteria. Each Yes-answer of the ten CASP criteria scored one point. An aggregate of Yesscores ≥ 6 was considered as acceptable quality.
Findings
Emerging burden of diseases with risk factors in Bangladesh
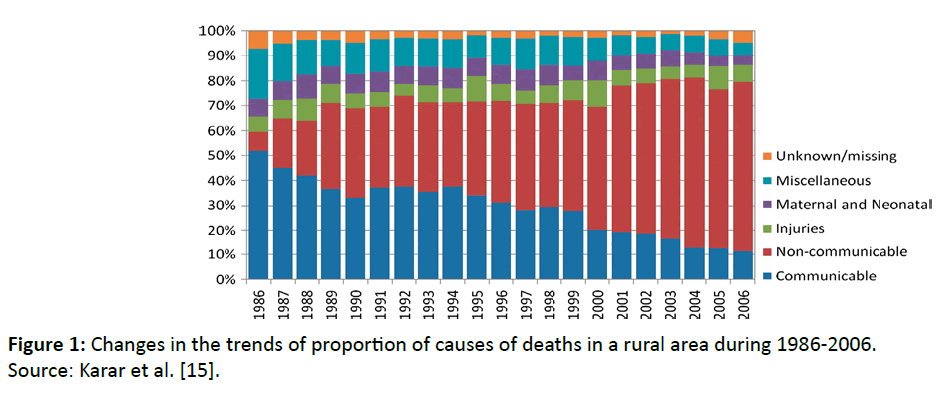
Karar et al. conducted a study at a rural area and analyzed the trends of causes of a total 18,917 deaths during 1986-2006. The study shows the ratio of the proportion of deaths due to noncommunicable (NCDs) to communicable diseases (CDs) was 8:52 in 1986 that was reversed to 68:11 in 2006 [15] (Figure 1).
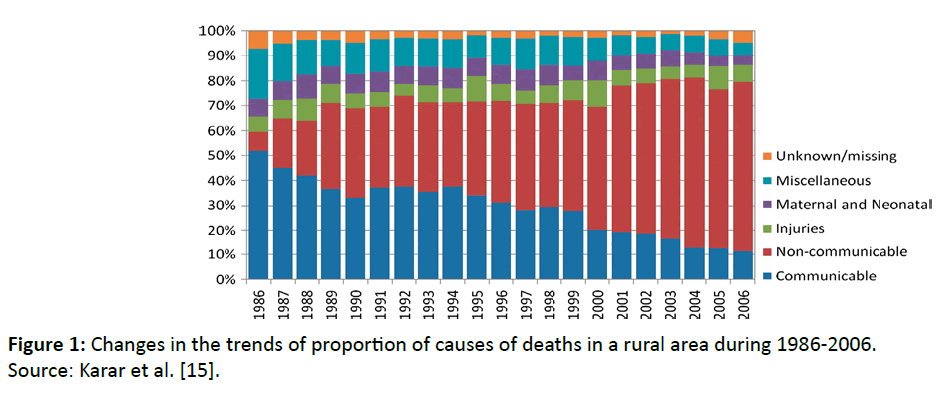
Figure 1: Changes in the trends of proportion of causes of deaths in a rural area during 1986-2006. Source: Karar et al. [15].
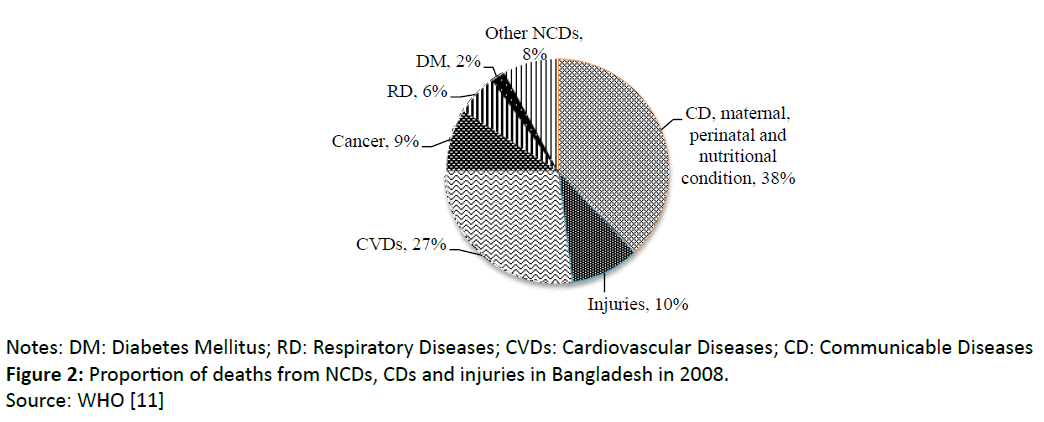
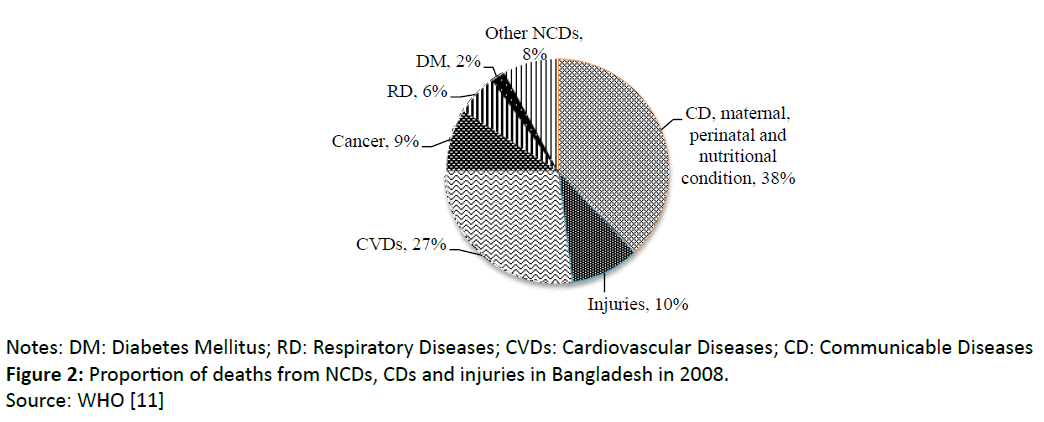
Figure 2: Proportion of deaths from NCDs, CDs and injuries in Bangladesh in 2008.
Notes: DM: Diabetes Mellitus; RD: Respiratory Diseases; CVDs: Cardiovascular Diseases; CD: Communicable Diseases
Source: WHO [11].
The report of the WHO (2011c) [16] shows that in 2010 the estimated prevalence of deaths due to NCDs and CDs were about 62% and 38% respectively in Bangladesh (Figure 2). Karar et al. [15] included communicable diseases were different from the WHO report that caused the differences in the proportion of CDs between those studies [17] (Figure 2).
From those reports, the distribution of morbidity and mortality at different referral facilities cannot be determined. We investigated the recently developed management information system (MIS) of the MOHFW to identify morbidity and mortality patterns at public referral facilities by Ministry of Health and Family Welfare [9,18].
A compare between top-5 prevalent morbidities in year 2011 and 2012 showed that diarrhoea, assault and respiratory disorders were common across all three referral facilities. Road traffic accidents (RTAs) were prevalent both in secondary and tertiary levels; however, cerebrovascular accidents and myocardial infarction were in rising trends at tertiary level facilities (Table 1).
| PHC level hospitals |
District (secondary) hospitals |
Tertiary level hospitals |
| Disease |
2011
Perc. (Rank) |
2012
Perc. (Rank) |
Disease |
2011
Perc. (Rank) |
2012
Perc. (Rank) |
Disease |
2011
Perc. (Rank) |
2012
Perc. (Rank) |
| Diarrhoea |
15.54 (1) |
17.74 (1) |
Diarrhoea |
11.10 (1) |
12.24 (1) |
Assault |
5.90 (1) |
4.92 (2) |
| Assault |
12.63 (2) |
13.51 (2) |
Assault |
7.42 (2) |
7.91 (2) |
RTA |
5.58 (2) |
6.31 (1) |
| Pneumonia |
7.46 (3) |
6.41 (4) |
Pneumonia |
5.73 (3) |
5.17 (3) |
Diarrhoea |
2.82 (3) |
Not in top-5 |
| Peptic ulcer |
7.43 (4) |
6.43 (3) |
RTA |
3.43 (4) |
3.71 (4) |
CVA |
2.31 (4) |
2.59 (4) |
| Enteric fever |
3.48 (5) |
3.48 (5) |
Br. asthma |
2.43 (5) |
2.44 (5) |
Poisoning |
1.98 (5) |
2.05 (5) |
| - |
- |
- |
- |
- |
- |
MI |
Not in top-5 |
2.82 (3) |
Notes: Perc.: Percentage; CVA: Cerebrovascular Accident; MI: Myocardial Ischemia.
Table 1: Reported proportions of top-5 diseases among admitted patients in all age and sex groups at primary, secondary and tertiary hospitals in 2011 and 2012; Source: Ministry of Health and Family Welfare, 2012; Ministry of Health and Family Welfare, 2013.
| PHC level hospitals |
District (secondary) hospitals |
Tertiary level hospitals |
| Disease RD |
2011
Perc.(Rank) 31.75 (1) |
2012
Perc. (Rank) 68.6 (1) |
Disease CVD |
2011
Perc. (Rank) 27.95 (1) |
2012(Rank) 17.9 (1) |
Disease CVD |
2011
Perc. (Rank) 23.41 (1) |
2012
Perc. (Rank) 12.9 (1) |
| CVD |
23.48 (2) |
45.3 (2) |
RD |
19.03 (2) |
10.4 (3) |
Poisoning and injury |
11.50 (2) |
8.9 (3) |
| Poisoning and injury |
11.99 (3) |
13.4 (3) |
Poisoning and injury |
10.26 (3) |
3.8 (4) |
Perinatal |
11.02 (3) |
9.7 (2) |
| Infections |
5.54 (4) |
12.0 (4) |
Infections |
9.59 (4) |
3.2 (5) |
RD |
9.21 (4) |
4.9 (5) |
| AAD |
3.04 (5) |
Not in top-5 |
Perinatal |
8.92 (5) |
13.8 (2) |
CVA |
8.93 (5) |
Not in top-5 |
| Perinatal cause |
Not in top-5 |
11.7 (5) |
- |
- |
- |
External causes |
Not in top-5 |
5.9 (4) |
Source: Ministry of Health and Family Welfare, 2012; Ministry of Health and Family Welfare, 2013.
Notes: Perc.: Percentage; RD: Respiratory Diseases; CVD/CS: Cardiovascular Diseases; AAD: Acute Abdominal Diseases.
Table 2: Reported proportions of top-5 causes of mortality in all sex and age groups at primary, secondary and tertiary hospitals in 2011 and 2012.
Notably, a compare of the top-5 causes of mortality in 2011 and 2012 revealed that respiratory, cardiovascular, poisoning and injury, perinatal disorders and infections were the prevalent causes of deaths in all three levels of public healthcare facilities with changing ranks (Table 2). Highly prevalent NCDs like diabetes mellitus, cancer, mental disorders were detected in rising trends that showed under the respective specialized facilities in the MIS reports. The MIS reports did not indicate rural-urban distribution of morbidity and mortality (Table 2).
Explicit evidence elsewhere show that changes in dietary habit and life style, rapid urbanization, increasing motorized mobility, reduced physical activity, tobacco use and indoor air pollution are the primordial factors of NCDs in Bangladesh [18]. The STEPS survey of the WHO in a sample of 9,619 adult (age ≥ 25) men and women showed that tobacco use in any form was 70% and 34.4% respectively. Tobacco use was higher in rural (55.5%) than urban (46.5%) area. Prevalence of overweight and obesity was 14.3% and 3.6% respectively. Whereas the prevalence of overweight is in rising trends, that the under nutrition in Bangladesh is one of the highest rankers among the developing countries (Directorate general of Health Services, 2010). There are commendable progresses to mitigate CDs through PHC activities; for example, by 2012, full immunization coverage in children ≤ 23 years was 84%. The reported national proportion of using improved drinking water and sanitary latrines were 98.2% and 80.4% respectively (Ministry of Health and family Welfare, 2013). However, the national strategic plan 2011-2015 of combating the emerging NCDs has yet to be effected as a priority public health issue [19].
Situation of medical students’ and doctors’ motivation for rural working
Impact of medical curricula on doctors and medical students
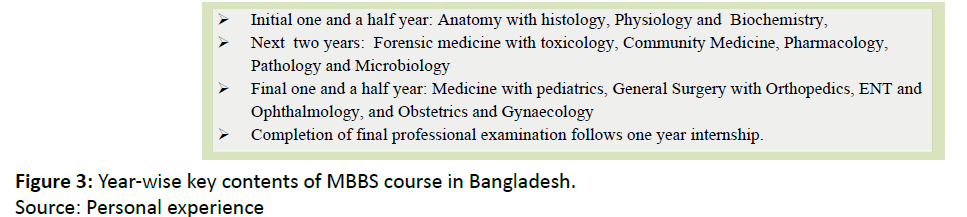
Graduate medical curricula are regulated by the ‘Bangladesh Medical and Dental Council’ [18]. The Bachelor of Medicine and Bachelor of Surgery (MBBS) curriculum lacks medical students’ opportunity of interacting with rural community except only 10 days visits to the rural PHC facilities for accrediting Community Medicine training out of a total 6-years MBBS education including one year internship. Figure 3 shows the main subjects of MBBS course (Figure 3).
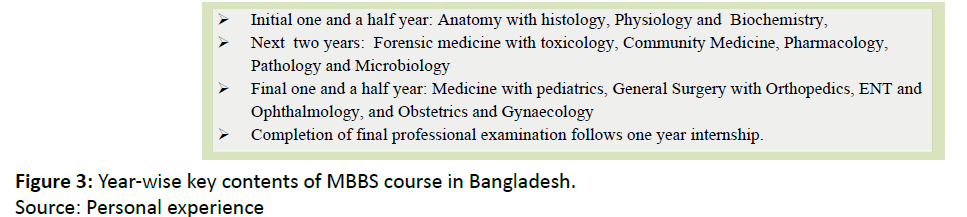
Figure 3: Year-wise key contents of MBBS course in Bangladesh.
Source: Personal experience.
Students irrespective of rural/urban residents constantly expose to urban environment and disease-oriented rather than rural-environment and patient-centered training, since all public and private medical colleges with adjoining training hospitals are urban-based tertiary level facilities. Consequently, at the end of graduation, it is usual to develop status gaps between doctors and rural people. The medical curricula have yet to adopt community-based total-care approach. Specialization in a curative discipline is often the main target of doctors for upgrading socio-economic and professional status. In Bangladesh, medical curricula are mostly influenced by the elites of the clinical disciplines. There is no evidence-based postgraduate course in family Medicine; hence, policymakers and doctors lack motivation and knowledge of the leadership supremacy of competent Family Physicians of implementing efficient and effective PHC services.
Health sector regulation versus doctors’ motivation for rural working with its impacts
The MOHFW implements health policy decisions through its central and local organizations. The Directorate General of Health Services is the central executive organization. Each Civil Surgeon (CS) is the head of a district (local) PHC system and district hospital. The ‘Upazilla Health and Family Planning Officer (UHFPO)’ is accountable to the CS and supervises the PHC activities of an upazilla [18]. While postgraduate public doctors are promoted to consultants and professors of the subdistrict/ district and teaching/specialized hospitals, that the senior Medical Officers initially to UHFPOs and then CSs. The key criterion to be promoted as UHFPOs is the duration of service rather than appraising one’s managerial skills.
Vacancies in the rural doctors’ posts are a problem of inefficient management of human resources. The following key demotivating factors were identified barrier to public doctors’ working at rural areas: lack of incentives and career opportunity, inadequate working environment and lack of transport and living facilities. Inefficient healthcare management is one of the key barriers to optimal utilization of the PHC facilities [14]. Nearly 70% of the total patients seek healthcare from private market where cost and quality are inadequately controlled; thus, rural people are at the risk of health catastrophe [20].
Discussion
Emerging health burdens of rural people
The rising prevalence of non-communicable diseases (NCDs), assaults and injuries and unsettled issues of communicable diseases comply with pattern of triple burden of diseases in Bangladesh. Gastrointestinal disorders are the commonest cause of morbidity at rural area which contradicting with the reported high access to safe water and sanitation (Table 1). For this, attention should be given either to health promotion for improving community knowledge, attitude and practice of hygiene or reporting system or both. It is identified that higher the referral level higher the admission rates of NCDs cases; hence, higher the total healthcare costs of the rural people. However, the PHC structure is adequate to prevent and control those cases at the community level provided doctors are deployed, retained and efficiently leading the PHC teams. The high prevalence of morbidity and mortality due to assault and poisoning are primarily social issues; hence, the solution remains beyond healthcare intervention. Moreover, all recognized risk factors of NCDs are highly prevalent in Bangladesh. For these, prevention and control of those factors through communitybased multisectoral approach integrating social and health services are the crucial health and economic priorities. Family Physicians as the leaders of the integrated services at Quebec, Canada have proved effective [21].
Influences of students and doctors motivation of rural working with its impacts
The current medical graduate and postgraduate curricula are hardly effective of motivating medical students to future working for rural community. The curricula do not address the patient-centered and community-oriented total healthcare rather than it diverts doctors to be urbanized, symptom-oriented curative healthcare professionals. Thus, solid science and technology-based medical trainings lack orientation regarding rural communities’ social, health and economic concerns. Nevertheless, public health service rules are insufficient to ensure regulatory compliance as well as managers’ and doctors’ responsiveness and innovation for healthcare needs of the rural people. Thus, the existing urban distribution and inefficient utilization of scarce resources, inequity and low access in healthcare are the risks of impoverishment of rural dwellers. Explicit evidences elsewhere recognize that competent Family Medicine practices are the cost-effective intervention to face the emerging globalized diseases burden [5,7].
Evidence-based practices of integrating Family Medicine and retaining rural doctors
Family Medicine has been recognized as a distinct specialty in many countries; for example, Australia, UK, USA, Brazil, South Africa, Hong Kong and sub-Saharan Africa. Some countries like Australia, UK, USA and Hong Kong conduct Family Medicine vocational training with varied duration after graduation. However, South Africa and Brazil conduct undergraduate Family Medicine courses. The curriculum of FM across countries’ unique goal is to develop five-star doctors having following qualities: competent clinician, manager, PHC team leader, teacher and community leader. Accordingly, there are similarities in course modules that include both scientific and humanitarian values. Some objective-based subjects of Family Medicine curriculum are: global health, social science, anthropology, public health, and bio-psychology. All countries commonly include community-based training. The promotion of statutory Family Medicine commonly requires political and professional motivation to prioritize for developing primary care equitable, accessible and optimally productive. However, to motivate and retain doctors to work as Family Physicians at rural areas are challenging [5,7,8,22,23]. Evidence-based practices to retain rural doctors elsewhere are: financial incentives in Laos, out of two, one year mandatory internship at rural area as in Columbia, and free housing and career-growth facilities for rural doctors as in Romania [3,24].
Strengths and limitations
To the best of our knowledge, this study is the first addressing need for Family Medicine in Bangladesh. Validity of the newly developed health Management Information System reports which is used in this study may not be claimed; moreover, private sector data are missing. However, opinions of the experienced local practicing doctors indicate that the reported diseases profile is a national reflection indeed.
Conclusion
Socio-economic, behavioural, cultural, healthful-awareness and environmental factors are the key determinants of the emerging diseases in rural Bangladesh. However, the traditional medical trainings and practices are neither person-centered nor community-oriented but technology-based. As a result, the bigger part of the iceberg of diseases burden remains unchallenged. To overcome the rural population’s social, health and economic threats, integration of Family Medicine in the country’s health system is a high priority. With this goal, the following policy reforms are recommended.
Integrating family medicine in the medical curricula as a postgraduate specialty
Introductory modules of Family Medicine should be included in MBBS curriculum. One year intensive rural-based training should be synchronized with undergraduate Family Medicine modules. Undergraduate Family Medicine and Community Medicine training facilities should be decentralized to the district and upazilla (sub-district) levels. Postgraduate Family Medicine training should be arranged in networks from community to university levels. To equalize the status with other clinical specialties, postgraduate training in Family Medicine should be 3 years long. To develop a context and evidencebased graduate and postgraduate Family Medicine curricula and department, local passionate and faculties from the Family Medicine pioneer countries should be involved. Fellowships should be provided to motivate graduates for Family Medicine. Provision of continuous professional development should be ensured for periodical accreditation of Family Physicians.
Retaining family physicians at rural areas
To retain Family Physicians at rural areas both financial and non-financial incentives should be institutionalized. The posts of the UHFPOs and CSs should only be reserved for the competent Family Physicians. They could be the faculties of Family Medicine training at community, district and university levels. Free housing and transport facilities should be provided to rural working Family Physicians.
References
- Labonte R, Mohindra K, Schrecker T (2011) The growing impact of globalization for health and public health practice. Public Health. 32: 263-283.
- Hays R, Pong LT, Leopando Z (2012) Primary care in the Asia-Pacific region: Challenges and solutions. Asia Pac Fam Med. 11: 8.
- Buchan J, Couper ID, Tangcharoensathien V, Thepannya K, Jaskiewicz W, et al. (2013) Early implementation of WHO recommendations for the retention of health workers in remote and rural areas. Bull. World Health Organ. 91: 834-840.
- WHO (2008) The World Health Report 2008,Primary Health Care Now More Than Ever.
- Evert J, Bazemore A, Hixon A, Withy K (2007) Going global: Considerations for introducing global health Into family medicine training programs.Fam Med. 39: 659-665.
- Reid SJ, Mash R, Downing RV, Moosa S (2011) Perspectives on key principles of generalist medical practice in public service in sub-Saharan Africa: A qualitative study. BMC. 12: 67.
- Sturmberg J, Heard S (2004) General practice education in Australia.
- Blasco PG, Levites MR, Janaudis MA, Moreto G, Roncoletta AFT, et al. (2008) Family medicine education in Brazil: Challenges, opportunities and innovations. Acad Med. 83: 684-690.
- Ministry of Health and Family Welfare (2012) Health Bulletin 2011.
- Lewis M (2006) Governance and corruption in public health care systems.
- WHO (2011a) Bangladesh-national expenditure on health.
- World Bank (2013) World Development Indicators: Poverty rates at national poverty lines.
- Bangladesh Bureau of Statistics (2010) Report on sample vital registration system-2010.
- WHO (2010) Health system in Bangladesh.
- Karar ZA, Alam N, Streatfield PK (2009) Epidemiological transition in rural Bangladesh. Glob Health Action. 2: 10.
- WHO (2011c) Non-communicable disease risk factor survey 2010.
- WHO (2011b) NCD country profiles 2011, Bangladesh.
- Ministry of Health and Family Welfare (2013) Health bulletin 2012.
- Ministry of Health and Family Welfare (2011) Strategic plan for surveillance and prevention of non-communicable diseases in Bangladesh 2011-2015.
- World Bank (2003) Bangladesh- Private sector assessment for health, nutrition and population (HNP) in Bangladesh.
- Vedel I, Monette M, Beland F, Monette J, Bergman H, et al. (2010) Ten years of integrated care: Backwards and forwards. The case of the province of Québec, Canada.
- Mash R, Reid S (2010) Statement of consensus on Family Medicine in Africa.
- Irlam J, Keikelame MJ, Vivian L (2009) Integrating the primary health care approach into a medical curriculum: A programme logic model.
- Busse R, Hafez-Afifi N, Harding A (2003) Regulation of Health Services. In:Harding A, Perker AS.Private Participation in Health Services.