- (2014) Volume 15, Issue 4
Nancy Kaddis, Muhammad Wasif Saif
Tufts Medical Center, Boston, MA, USA
Recent data suggests that treating patients with pancreatic cancer that express mutations in BRCA1, BRCA2, and PALB2 with chemotherapy which targets the DNA repair defect in these cells, such as platinum based therapies or PARPi [poly (ADP-ribose) polymerase inhibitor], may be more beneficial in these patients. Moreover, further data also indicates the promise of combining PARPi with conventional chemotherapy. Authors summarize the data related to PARPi in BRCA-associated pancreatic cancer that was presented at the annual meeting of ASCO 2014. Enrolment on a clinical trial for patients who fit these criteria should be encouraged.
5-fluoropyrimidine; Drug Therapy, Combination; irinotecan; Pancreatic Neoplasms; S1 (combination)
FOLFOX: 5-fluorouracil, leucovorin and oxaliplatin; IRIS: S-1 plus irinotecan; APC: advanced pancreatic cancer; PDAC: pancreatic ductal adenocarcinoma; GEM=gemcitabine; FOLFIRINOX: FOLFOX plus irinotecan; MPC: metastatic pancreatic cancer; PFS: progression free survival; OS: overall survival; ECOG PS: Eastern Cooperative Oncology Group performance status; AE: adverse event; nab-P: nab-paclitaxel; INFL: inflammation; OFF: Oxaliplatin + 5-FU + Leucovorin
There has been limited data regarding optimal second line treatment for advanced pancreatic cancer (APC). However, this is starting to change, as new studies have shown positive effect on overall survival in the second line setting. Until recently, various regimens were used as palliation in this setting. However, there has been interesting data regarding the combination of gemcitabine with oxaliplatin or docetaxel with respect to progression free survival (PFS) and tumor response in 1st line. Other regimens used fluoropyrimidines either alone or in combination with oxaliplatin or other chemotherapeutic agents (such as the FOLFIRINOX regimen).
One study, the Doc-Ox trial, investigated the combination of oxaliplatin with docetaxel as 2nd line treatment after progression under palliative first-line systemic treatment with gemcitabine [1]. The response rate was 16% with a disease control rate of 48% after the first two treatment cycles. Median PFS was 7 weeks and median OS after start of 2nd line therapy was 36 weeks; these results were very encouraging compared to other 2nd line-protocols such as OFF. Some patients seemed to benefit particularly as indicated by long periods of treatment in this setting. Even after 8 cycles of treatment with Doc-Ox, partial response was observed in 2 patients and stable disease in another 6 patients, corresponding to a disease control rate of 18%.
Ameta-analysis presented at ASCO 2013 investigated optimal second line treatment for APC [2]. A total of 69 studies of 2nd line chemotherapy for pancreatic cancer (77 arms, n=2859) were identified. A majority of the subjects had received prior gemcitabine-based chemotherapy. An exploratory analysis hinted that intensification of gemcitabine-based therapy (ORR: 10.0%; DCR: 54.7%) might be marginally more active than fluoropyrimidine (7.6%; 32.2%) or taxane based 2nd line treatment (5.2%; 33.6%). Not surprisingly, the percentage of second line delivery ranged from 14 – 68% and correlated with OS (r=.49, p<.01) and PPS (r=.57, p<.01). When phase II studies were excluded, correlation was improved for OS (r=.63, p<.01) and PPS (r=.79, p<.01). The authors of this meta-analysis concluded that while we await further advancement in the 1st line setting of pancreatic cancer, the increased delivery of 2nd line chemotherapy to patients with advanced pancreatic cancer who maintained performance status may offer a survival benefit for this population.
To this end, several studies, presented as the 2014 ASCO meeting, address the issue of the most effective, and least toxic, regimens to use in 2nd line treatment of pancreatic cancer.
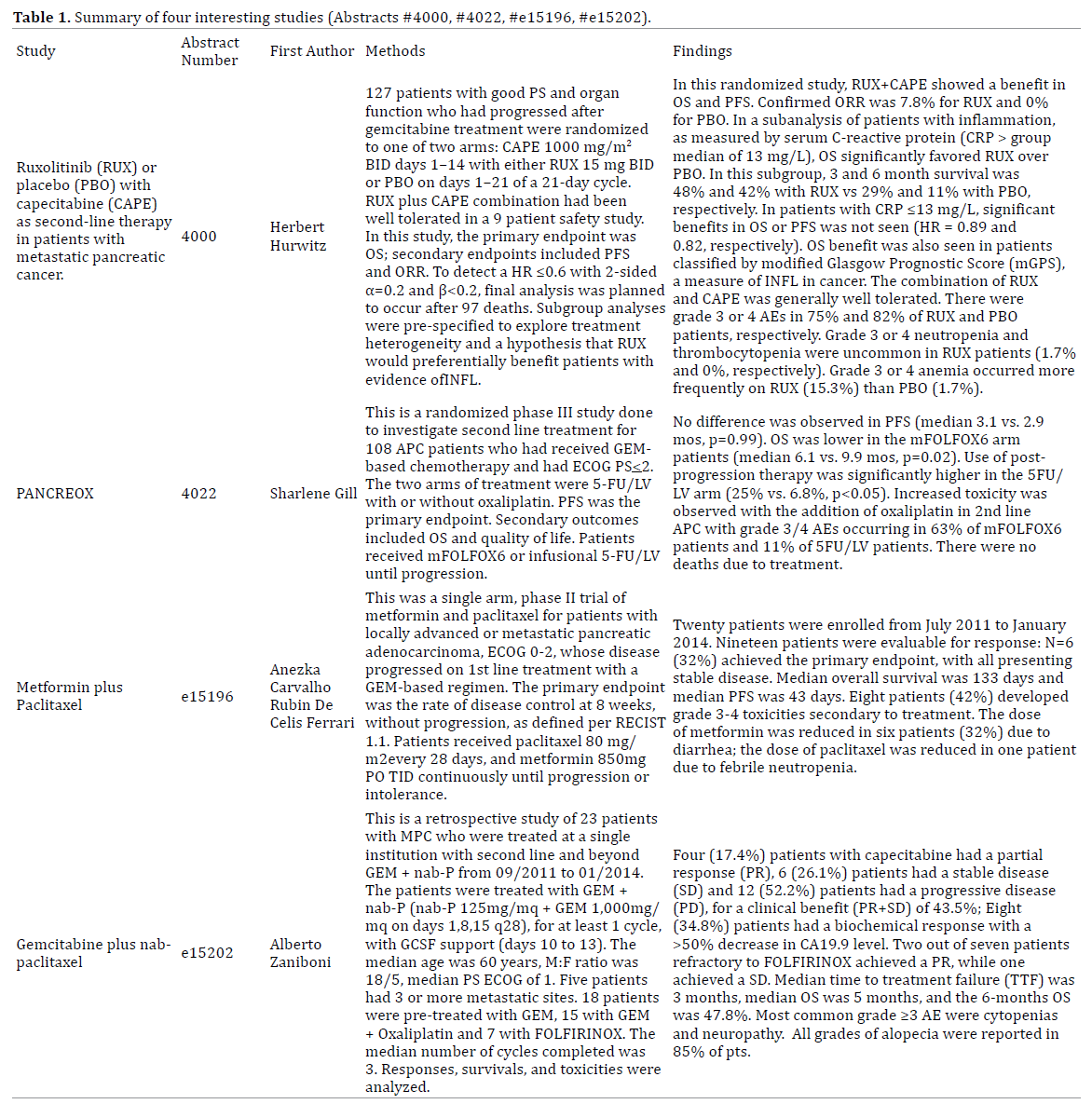
We summarize four interesting studies (Abstract #4000, Abstract#4022, Abstract #e15196, #e15202) presented at the ASCO Annual Meeting in 2014, in Chicago, IL, USA, May 30-June 3, 2014 (Table 1).
Pancreatic ductal adenocarcinoma is a leading cause of deaths due to cancer with a 5 year mortality of < 5%; there are few options for patients whose tumor progresses past first line treatment. Unlike first line treatment of pancreatic cancer, there is not much data regarding standard of care for second line chemotherapy for advanced pancreatic cancer. The following are discussions of the findings of the studies which we have summarized.
Systemic inflammation is often seen in patients with advanced malignancies, and confers for poor survival [3]. Several studies have shown that baseline elevated CRP (>13 mg/L) is a poor prognostic marker in pancreatic cancer, as well as other malignancies [4, 5]. In this randomized phase II study by Hurwitz et al., a novel agent Ruxolitinib (JAK1 intention to treat analysis shows no significant OS benefit for the whole group but sub-group analysis shows a significant improvement (p=0.01) in OS for the group of patients with APC and increased systemic inflammation, which is indicated by CRP>13 mg/L with a HR of 0.47 for the RUX+CAPE versus the CAPE+PBO group [6]. When a pre-planned Cox regression analysis performed to explore whether baseline characteristics in the subgroup of patients with a CRP>13 mg/L affected OS, adjusted HR for OS was maintained at HR=0.50 and 2 sided p=0.037. These data provide evidence for the important role of inflammation in cancers and the JAK-STAT pathway is a major target for inhibition of inflammation and treatment of advanced pancreatic cancer. Based on this study, other phase III trials are underway to explore the benefits of Ruxolitinib in the second line treatment setting for advanced pancreatic cancer.
In the CONKO-003 trial, there was randomization of patients who had progression of disease after gemcitabine therapy into one of two study arms. The first arm received oxaliplatin (85 mg/m2 on days 8 and 22) plus 5-FU (2 g/ m2 over 24 h) and leucovorin (200 mg/m2 on days 1-8 and 15 to 22) or 5-FU and leucovorin. There was a significant benefit for patients in the oxaliplatin arm with progressionfree survival (13 weeks versus 9 weeks, P = 0.012) and median overall survival (26 weeks versus 13 weeks, P = 0.014) [7]. The use of second-line chemotherapy might, therefore, provide equal benefit as an initial approach of front-line combination chemotherapy. In the study from this year’s ASCO meeting done by Gill et al., no benefit was seen by adding oxaliplatin to infusional 5FU/LV in gemcitabine-treated 2nd line APC [8]. PFS was similar in the two groups and OS was inferior with mFOLFOX6. Given the proven benefit of FOLFIRINOX in untreated APC (ACCORD 11), this indicates that the most optimal setting for use of oxaliplatin-based treatment may be in the 1st line setting. More trials need to take place in order to confirm these findings.
There is a growing body of literature suggesting that type 2 diabetes mellitus (DM) may be associated with the development of pancreatic cancer, but this association is complex and not completely understood [9]. Investigating the effect of anti-diabetic therapies on pancreatic cancer has been thought to be a critical step in clearly understanding the role of type 2 DM in the development of pancreatic cancer. Two epidemiologic studies have, in fact, found that diabetic patients treated with metformin were less likely to develop cancer, but those treated with insulin were more likely to die of various kinds cancer. Despite the encouraging pre-clinical evidence of antitumor activity of metformin in advanced pancreatic cancer, the primary endpoint of disease control rate was not met in the study done by Ferrari et al. presented at this year’s ASCO meeting [10]. In addition to poor efficacy, the treatment combination was poorly tolerated and should probably not be studied further.
Finally, the last study that we discuss focuses on patients who have received FOLFIRINOX as first line treatment for APC, and their disease has progressed after this regimen.
While FOLFIRINOX is a reasonable non-gemcitabine based regimen to be used in first-line setting, patients can also receive gemcitabine as adjuvant therapy. The combination of gemcitabine and nab-P had been shown to be effective in the treatment of metastatic pancreatic cancer and in September 2013 it was approved by the FDA to be used as first line treatment in the first line setting. The study discussed above by Zaniboni et al. showed that gemcitabine plus abraxane with GCSF support is a potential effective second line treatment for metastatic pancreatic cancer, even in FOLFIRINOX refractory patients. Side effects were acceptable and the 6-month OS are promising [11]. However, this is a small study and future larger trials are needed to confirm these findings. It will be important to monitor this population for the development of peripheral neuropathy as both oxaliplatin and abraxane are known to have this potential side effect.
Future trials should further explorethe role of the JAKSTAT pathway in the role of inflammation and treatment of refractory and advanced pancreatic cancer. This is a pathway that seems to have a marked benefit in those with high inflammatory markers in pancreatic cancer as seen in this year’s study by Hurwitz and colleagues. This pathway’s potential role as a target in this setting, if confirmed, is very promising. We also need more studies before we confirm findings reported here by Gill and colleagues, that oxaliplatin-based chemotherapy is most appropriate in the first line setting of treatment for pancreatic cancer. In a small trial presented this year by Ferrari and colleagues, metformin does not seem to be an efficacious agent used in the setting of advanced pancreatic cancer; its toxicities were also great. Finally, we need larger studies to support findings from the trial done by Zaniboni and colleagues that gem-abraxane would be a beneficial regimen to use in the second line treatment setting for metastatic pancreatic cancer (Figure 1).
The authors have no potential conflicts of interest.