Research Article - (2018) Volume 2, Issue 1
Deanna L Mulvihill1*, Marilyn Ford-Gilboe2, Helene Berman3, Cheryl Forchuk2, and Rick Csiernik4
1Department of Hospital & Health Care, Nursing & Education at Cogenz, USA
2Arthur Labatt Family School of Nursing, The University of Western Ontario, Canada
3Faculty of Health Sciences, The University of Western Ontario, Canada
4School of Social Work, King's University College, Canada
*Corresponding Author:
Mulvihill DL
Director, Department of Hospital & Health Care
Nursing & Education at Cogenz, USA
Tel: 703-585-7264
Email: deannalifestyle@hotmail.com
Received date: April 2, 2018; Accepted date: April 13, 2018; Published date: April 25, 2018
Citation: Mulvihill DL, Ford-Gilboe M, Berman H, Forchuk C, Csiernik R (2018) Seeking and Obtaining Help for Alcohol Dependence by Women with Posttraumatic Stress Disorder and a History of Intimate Partner Violence. J Addict Behav Ther Vol 2 No 1:4.
Copyright: © 2018 Mulvihill DL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Women who have experienced violence are at a greater risk for physical and mental health problems. Researchers report that women with these experiences are more difficult to treat and many do not seek treatment and those that do are more difficult to treat and have difficulty maintaining helping relationships. However these women's perspectives have not been previously studied. This study describes the experience of seeking help for alcohol dependence by women with PTSD and a history of intimate partner violence in the context in which it occurs.
Keywords
Women; Trauma; Intimate partner violence; Alcohol dependence
Introduction
In addition to safety concerns, women who have experienced Intimate Partner Violence (IPV) are at greater risk for physical and mental health problems including posttraumatic stress disorder (PTSD) and alcohol dependency [1] than their nonabused counterparts [2,3]. IPV, PTSD and alcohol dependency result in significant personal, social and economic costs [4,5] and the impact of all three experiences together may compound these costs.
Women with these experiences are more difficult to treat than those with alcohol dependency alone [4,6]. Many do not access treatment programs [7] and, those who do, frequently do not stay [8]. Counselors report that these women have difficulty in maintaining helping relationships [6,9,10]. However, these women’s perspectives about seeking help have not previously been studied.
The benefits of social support in recovery from alcohol dependency have been documented [10,11]. However, little is known about the role social support plays in the recovery process [12] or the ways in which women with a history of IPV and PTSD seek and obtain help for alcohol dependency. The purpose of this study was to describe the experiences of seeking help for alcohol dependence by women with PTSD and a history of IPV. The study focused on one treatment center to explore how the culture of the organization and the interactions between the women and the treatment staff shaped the women’s experiences.
Theoretical framework
Since no theory fully explains IPV, PTSD or alcohol dependency, researchers recognize the need for a broad lens to study these problems [13,14]. An ecological model provides such a lens by focusing on how the health of individuals is shaped not only by individual dispositions, but also by various social, structural, and environmental factors and the interactions between these elements [15,16]. These factors are represented by a set of nested concentric circles of systems in which the individual is embedded, that interact and influence the development and health of that individual. These systems are known as the microsystem, mesosystem, macrosystem, exosystem, and the chronosystem [15]. The microsystem is the primary system where individuals spend considerable time, such as the family or work setting. The mesosystem reflects the interaction between two or more primary systems, such as the interface between a health agency and the family, or work and the family. The macrosystem refers to the overall authority such as the Ministry of Health for the health agency, and the exosystem refers to the broad cultural values and beliefs, such as patriarchy and democracy that shape other systems. When these broader systems make decisions, they influence the primary system in ways that they may not fully appreciate. Finally, the chronosystem includes those transitions in life, such as graduation and marriage that change the individual’s role in society.
The mesosystem has the greatest possibility of directly influencing health [15]. Thus, in this study, Bronfenbrenner’s ecological model provided a lens for focusing on the interactions that occur within a key mesosystem context for women with PTSD, alcohol dependency and a history of IPV. More specifically, this study examined the interaction of women seeking help and the counseling staff. An ecological framework necessitates studying the ways in which features of the macrosystem and exosystem also affect women’s help seeking.
Extensive research has been conducted in the areas of IPV, PTSD and alcohol dependency and recent research has explored the relationship between PTSD and alcohol dependency. However, little research has examined the interrelationships among all three phenomena. This review focuses on the relationships among IPV, PTSD and alcohol dependency and the impact on women’s efforts to seek and obtain help.
Health effects of IPV
The effects of violence can be devastating to a woman's mental and physical wellbeing [17,18]. In addition to causing injury, violence increases women's long-term risk to a number of health problems, including chronic pain, physical disability, drug and alcohol abuse, and depression [19,20]. Furthermore, there is evidence to suggest that the health effects of IPV may persist after the violence ends [21,22]. Findings from an ongoing, longitudinal study examining the physical and mental health of a sample of 309 Canadian women who had recently left abusive partners suggest that women experience varied ongoing health challenges after leaving. For example, at the time of first interview, 82% of women reported one or more active medical diagnoses, 45% screened positive for problem drinking and 52% were experiencing symptoms consistent with a diagnosis of PTSD [23]. This suggests that IPV, PTSD and alcohol dependency are often intertwined, with each providing a context for the others.
Such findings point to a need for ongoing support from health and social services. The loss of social contacts experienced by women during IPV may lead to social phobia, while fear of embarrassment may result in low self-concept and self stigmatization [24,25]. Trauma appears to disrupt the sense of an intact self [26], such that the person's identity becomes externally derived. Trauma also affects the person’s social reality and worldview [27], shattering views about themselves and the social environment [28]. Their concepts of right and wrong are challenged, and often destroyed [29]. After trauma, access to social support has been linked to better health outcomes while continued social isolation has been associated with an increase in symptomatology [26]. However, many victims of violence who seek care often go inadequately treated [18].
PTSD and alcohol dependency
Individuals with PTSD show evidence of increased autonomic reactivity [30] in which repeated exposure to threatening stimuli, whether actual or with PTSD reexperiencing symptoms, causes neural activation [31,32]. Repeated neural activation results in a lower threshold of stimulation required for activation, such that minor stressors can elicit full-blown hyperarousal [33]. While reexperiencing traumatic events, persons may disassociate, especially when dealing with strong emotions [31,34]. At intense points in treatment, a person with PTSD may unconsciously disassociate, and, if the counselor does not recognize this, he or she may misinterpret the symptoms, interfering with the therapeutic relationship.
Neurobiological and brain-imaging studies have identified chemicals, regions [35] and neurotransmitter pathways [36] involved in alcohol cravings. The brain adapts to the prolonged or excessive presence of alcohol by making changes in certain cells, called neuroadaptation. This neuroadaptation occurs more quickly in persons who have experienced trauma [37,38]. Once these changes occur, it has been proposed that a process of classical conditioning is responsible for the cravings and compulsions [35]. Alcohol, a central nervous system depressant, may be used as a form of self-medication [39]. After alcohol consumption, as the blood alcohol level drops, the nervous system is aroused. This hyperarousal may trigger reexperiencing and even greater hyperarousal that can, subsequently, increase the craving for alcohol [40]. There is evidence to suggest that persons with PTSD and alcohol dependency may find the physiological arousal from withdrawal extremely difficult, such that inpatient admission with pharmacological support may be necessary [35]. Furthermore, results of research on detoxification have documented increases in anxiety, cravings and seizures with each successive detoxification [41]. These findings highlight the importance of considering the role of PTSD in detoxification and in building supports for success with each detoxification. However, little attention has been given to the intersection of PTSD and alcohol dependency or how to deal with these conditions together as part of a treatment plan.
Social support in IPV, PTSD and alcohol dependency
A woman's development and experiences throughout her lifetime are structured around relationships and it is within the context of societal attitudes toward women's use of alcohol that women's views of themselves are formed. Therefore, if society devalues women who are dependent on alcohol, these women may also think less of themselves.
In this regard, families can either help or hinder but they are seldom neutral. Women who do not have social support from family members, friends or a partner are less likely to access treatment. If problems in relationships are unresolved, it is difficult for women to sustain any progress made through treatment. Additionally, women may find their roles as caregivers to be incompatible with treatment seeking such that they forgo or postpone treatment because they do not have someone whom they can trust to care for their children. Some fear that they will lose their children if they enter treatment while, for others, regaining custody is a primary motive for entering treatment. Despite these findings, little research has been conducted to examine how friends and family relational styles or behavior might help or hinder the woman with alcohol dependence. Although many programs have family sessions as part of the treatment approach, it is primarily psychoeducational with little consistency in the content or the type of guidance considered most beneficial [13].
The loss of social contacts experienced by many women during IPV may lead to social phobia and fear of embarrassment, resulting in low self-concept, loss of selfesteem, and selfstigmatization [24,25]. Negative stereotypes may prevent women from identifying their own alcohol use as problematic [42], as there is an association between women’s self-image, stigmatization and their denial of alcohol dependence. An outcome of these stereotypes, professionals are reluctant to ask women about substance use and, therefore, they may miss an early intervention opportunity [1].
Social support has been associated with positive outcomes of alcohol treatment in many studies [7,43-45]. In a study by Bischof et al. success factors in treating alcohol abuse included having few social problems and a high degree of social support. It is also suggested that lack of social support is a risk factor for relapse. Clearly, for women with IPV, PTSD and alcohol dependency, social support is a critical factor affecting their recovery and quality of life. However, few studies have addressed broader factors involved in social relationships, such as alienation or stigma that may be crucial factors in explaining how women manage the fallout of past or ongoing violence, cope with distressing symptoms of PTSD and alcohol dependency or seek treatment for dependency.
Studies of women who have experienced IPV have documented the buffering effect of social support on health outcomes [21,46,47]. There is also empirical evidence for the role of social support in decreasing PTSD symptoms [48] and with decreasing relapses in sobriety for those dependent on alcohol [7,43-45]. However, the results of such studies are difficult to compare due to differences in the definition and measurement of social support.
Formal social support
There is evidence that IPV often goes unrecognized in health care settings [49-51]. Women who experience IPV may be reluctant to reveal their abuse for fear of retaliation by their partners [52]. Regrettably, in many alcohol treatment settings, staff do not generally assess for PTSD or IPV [53]. In a grounded theory study, Wuest et al. [54] identified intrusion or interference in everyday life as the primary problem faced by women after leaving an abusive partner. Intrusion stems from past and ongoing abuse and its consequences, including economic and health problems and the costs of getting help from both the formal system and women’s own social networks. Many times, offers of support came with conditions, such that the women felt robbed of the control they needed to make necessary changes in their lives. Although this study included women with both PTSD symptoms and alcohol dependency, whether these conditions interfered with help seeking was not specifically considered in the analyses.
Women who have experienced IPV often feel isolated [55,56]; women with PTSD have symptoms that may interfere with their relational capacity [47]; and women who become dependent on alcohol tend to isolate themselves [57]. However, we do not know what happens when women who have a history of IPV and PTSD seek help for alcohol dependency and if such interactions meet their needs. Although a few studies have addressed the role of support in recovery from alcohol dependency, no studies have examined formal support provided to women who have PTSD, alcohol dependency and a history of IPV. A better understanding of women’s experience of seeking support for alcohol dependency is needed as a foundation for developing programs that are effective in supporting women in their attempts to regain their health.
Canadian researchers suggest that two-thirds of women with alcohol dependence have mental health problems that include posttraumatic stress disorder (PTSD) and many of these women are survivors of intimate partner violence (IPV) [1]. The combination of alcohol dependence, PTSD and IPV may compound the personal, social and economic cost of each [4,5], in part, because women with these experiences are more difficult to treat than those with alcohol dependence alone [4,6].
Recognizing that recovery from alcohol dependence is a longterm process that cannot occur solely in short-term, residential treatment, in this paper we explore the women’s experiences of seeking help before, during and after residential treatment, with a focus on their efforts to access treatment. In this study, we utilized an ecological model to focus on the women in the context in which they live and the complex association between health and the environment [15].
The role of trauma in recovery from alcohol dependence
Clinicians and researchers acknowledge the importance of being sensitive to trauma, gender and individual needs in the delivery of alcohol treatment services for women [58]. For instance, women often describe their substance use as having a sudden and heavy onset, often following a traumatic event. In contrast, men’s patterns of substance use are often described as gradual and progressive. Thus, opportunities for early intervention for women who develop a dependency because of a traumatic event have a limited timeframe [1]. In addition, substance abuse treatment for women received little attention until the 1970s when research on the differential impact of alcohol on women’s versus men’s bodies became prominent. This body of research also highlighted other factors that shape women’s use of treatment, such as access, child care, transportation and financial resources. However, despite these studies, women still do not have access to a broad range of services, coordination of care remains lacking and screening to identify the need for treatment is frequently not carried out.
In many alcohol treatment settings, information about trauma is not investigated or treated, and staff members are generally not requested to assess for PTSD or IPV [53]. This may have some bearing on why some research suggests that persons with alcohol dependency and PTSD are more difficult to treat [4,6,9].
There is a pattern of interaction between alcohol withdrawal and PTSD symptoms that may make detoxification more difficult. Persons with PTSD and alcohol dependency may find the physiological arousal resulting from alcohol withdrawal impossible to cope with, such that inpatient admission with pharmacological support may be necessary. Furthermore, results of recent research on detoxification have documented increases in anxiety, cravings and seizures with each successive detoxification [41,59]. These findings highlight the importance of considering the role of PTSD in detoxification and the importance of building a structure of support for recovery after detoxification. More attention needs to be given to the intersection of PTSD and alcohol dependency and how these conditions together.
Previous studies on treatment outcomes for alcohol dependence
While the characteristics of persons with alcohol dependence have been widely studied, the outcomes of treatment for AD have received limited attention. The outcome studies that have been conducted have consistently shown that brief interventions are more effective than no treatment and just as effective as long-term treatment. Most often, clinical trials either of a specific program or pharmaceutical intervention have produced more positive results than outcome studies of standard treatment. In response to the high correlation between PTSD and alcohol dependency, together with poor treatment outcomes, Najavits [60] developed a special program for women with co-occurring PTSD and alcohol dependency called Seeking Safety that provides treatment for both problems concurrently. This program is being evaluated in different populations using standardized guidelines so that future meta-analysis will be possible [60]. This program is the most empirically studied treatment thus far for trauma, PTSD and substance abuse. It has shown positive results in seven outcome studies, including two randomized control trials [60].
In one study, Najavits et al. [61] of dually diagnosed women (PTSD and alcohol dependence), decreases in abstinence days, PTSD symptoms, depression and significant positive changes in cognitive and coping skills were found 3 months postintervention. This study shows that women can be helped when they were presented with a program based on their alcohol dependence and other needs. However, the lack of a control group in this study is a limitation [61]. Najavits et al. [61] reported results of a randomized controlled trial of 33 outpatients with both PTSD and substance abuse who received the seeking-safety intervention (n=-18), with treatment as usual (n=15). This trial consisted of 24 out-patient sessions and three months of follow-up. Results showed significantly better outcomes in a variety of domains for those in the intervention group. Another randomized controlled trial of Seeking Safety included 62 patient participants, divided evenly between intervention (n=31) and control (n=31) groups. After 20 weeks of treatment and three months of follow up, there was a significant decrease in substance abuse days, as measured by the Addiction Severity Index at baseline and monthly throughout the study. Brown et al. [9] also conducted a quasiexperimental study of nine treatment sites involving 157 participants and 32 clinicians. The clinicians rated the program as highly relevant and the clients rated it as uniquely touching their needs. In their review article, Najavits et al. [61] list safety as the urgent clinical need and coping skills to work toward discontinuing use, letting go of dangerous relationships, gaining control over PTSD symptoms and asking for help as other critical needs.
In summary, further exploration of the interactions between women with the experiences of IPV, PTSD and alcohol dependency and their formal and informal support networks is required. Women who have experienced IPV often feel socially isolated and stigmatized [55], women with PTSD have symptoms that may interfere with their relational capacity [47] and women who become dependent on alcohol tend to isolate themselves [57]. Unfortunately, we do not know what happens when women seek help from individuals or agencies and how such interactions meet their needs for social support. These interactions do not occur in isolation. Therefore, it is important to understand the sociocultural context in which they occur and how this affects women’s ability to seek, gain access to and benefit from treatment services.
Research Questions
Two research questions were addressed in this study.
• 1) What are the experiences of women with PTSD and a history of IPV in seeking help for alcohol dependence in the context of this site?
• 2) How are women’s experiences of seeking and obtaining help influenced by their personal dispositions and resources, including informal support networks, interactions with treatment staff, and broader cultural beliefs related to IPV, PTSD and alcohol dependency?
Method
This study used an intersubjective Ethnographic approach that incorporated hermeneutic dialogues to develop a shared understanding of women’s experiences of seeking help [62]. The focus was the interactions between women with the experiences of IPV, PTSD and alcohol dependency and the counseling staff at an alcohol treatment center. Since these interactions do not occur in isolation, the sociocultural context was also examined.
Site selection
The treatment center was in a rural area located just outside a large metropolitan city surrounded by small towns and suburban developments. This site was ideal because the Ontario Hospital Insurance Plan covered all treatment fees so that women of varied economic means could attend the program. Although rural, it was easily accessible to a diverse population and had a van to pick up women from the bus station. It was a woman only program as the founders recognized that women often felt safer in a women-only environment than in one that included men.
Sample recruitment and consent
Women seeking treatment (clients) and staff who provided services at the treatment center were recruited as participants. Informed consent was obtained from all participants prior to data collection. Sample recruitment occurred in stages that coincided with the phases of data collection. First, consent to be a participant observer in the center was obtained from the Board of Directors through the Executive Director. I then met with the staff as a group to explain the project and each staff member was asked to indicate in writing if they were willing to have me contacted them. I contacted all staff members who gave consent, answered their questions and invited them to participate in an in-depth interview. All the staff consented to participate in the participant observation period and to be observed in group and individual sessions to which their clients consented.
Clients: All 40 women who entered the residential center over a four-month period were observed in various interactions with the staff. At the first group meeting, I explained the study. All groups gave consent to attend both individual and group sessions provided I would leave if anyone became uncomfortable with me being there. Women who signed ‘Consent to Contact Form’ were approached for an in-depth interview.
A purposeful sample of 12 adult, English speaking clients was selected to be key informants based on the following criteria:
• a) over 19 years of age;
• b) past or ongoing IPV;
• c) a score of 5 or above on SPAN a screening tool to determine the presence or absence of PTSD symptoms [63];
• d) identified alcohol as their drug of choice; and, to verbally articulate their experience of seeking treatment.
Each key informant selected a pseudonym for herself; this name and the code number were accessible only to the researcher and her supervisor. Maximum variation sampling in age, length of time of dependence, economic status and educational attainment was utilized making any patterns in this small number more significant [64]. Many women wanted to participate as key informants but did not meet the criteria; typically because alcohol was not their drug of choice or they did not have a history of IPV.
The 12 key client informants varied in age from 19 to 52 years, with all but one being under 36 years. All but four of the women had children (ages three months to 20 years) and all children under 16 were under some form of supervision by a child protection agency. The women’s employment status was diverse and included managers, educators and waitress. However, many were presently receiving social assistance (welfare) benefits. Educational attainment ranged from Grade 9 to master degrees. Their abuse histories spanned from occasional incidents of abuse to battering for more than 10 years, while the duration of alcohol dependency varied from 1-15 years. Their scores on the SPAN test ranged from 5-12. Although many previously had stable employment situations, most had suffered substantive losses, including jobs, cars and homes and only three of the women were presently living with a partner. All of these women had experienced childhood trauma.
Staff: Six key staff informants were selected for in-depth interviews. Maximum variation was sought in age and length of time working as an addiction counselor and whether the staff had a personal history of recovering from a alcohol dependence. All women spoke English and their ages ranged from 22 to 66 with only two being under 44. Their work experience varied from six months to 16 years with only one being under two years and only two being under six years. Only one had previously worked in another treatment center. Four staff key informants had a personal history of alcohol dependence and the other two did not. All had some level of addiction education, but none had achieved a university degree.
Data collection
This study received ethics approval from the Health Science Research Ethics Board at the University of Western Ontario. Methods used to collect data were participant observation, informal interviews, in-depth interviews, reflective journaling and focus groups. The materials produced by these methods were field notes and transcribed text. Periods of data collection were interspersed with periods of analysis such that questions raised during the analysis were taken back to the participants for clarification and more in-depth discussion, thus building shared understanding. Using a reflective journal, I critically questioned my responses to the data in order to reveal my own biases, so that the impact of these biases on the findings could be minimized and to develop an authentic description of women’s experiences of seeking help.
There were three periods of data collection lasting to ten days over a four-month period (Figure 1). In period one, I observed the interactions between clients and the staff and then asked questions of both about what I observed. These informal interviews during the participant observation period helped validate my observations and clarify the informant’s perceptions (e.g. Was that feedback helpful to you? You seem upset; can you tell me about it? Could you explain why you responded to the client in that manner?). Field notes were kept and analyzed, and new questions formulated for the in-depth interviews. Semistructured, in-depth interviews began at the end of the first data collection period and continued into period two. These interviews lasted approximately 60 minutes and took place in a private office or a place of the women’s choosing. All interviews were recorded and transcribed verbatim. Staff interviews took place after the first set of client interviews were completed so that client interviews could inform the questions asked during staff interviews. After analysis of the in-depth interviews, I conducted second interviews with some of the key informants to clarify the analysis or ask more detailed questions. Not all informants were interviewed a second time, but the interviews alternated between the clients and staff members and continued until a shared understanding was reached between the informants and myself. After each data collection period, the researcher developed a narrative summary for the executive director who then shared her perspective on the findings from an administrative point of view. After initial analysis, I held two focus groups, one for the clients and one for the staff, to share the emerging analysis and to obtain feedback.
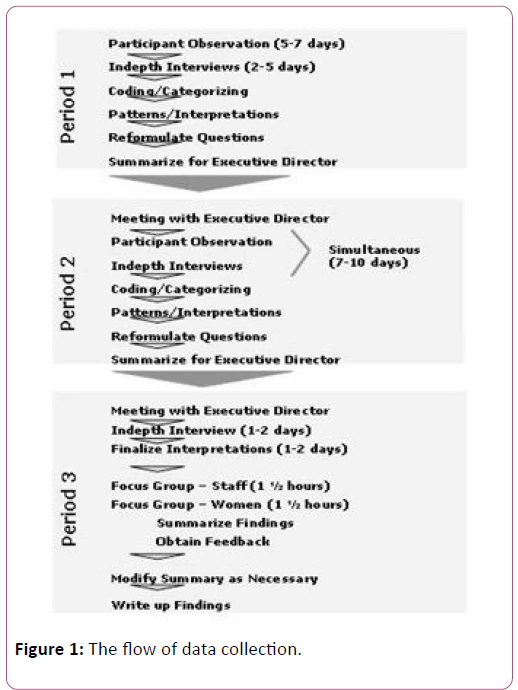
Figure 1: The flow of data collection.
Participant observation
Participant observation was continuous throughout the study, but the most intensive time occurring in the first data collection period. I arrived at breakfast time, followed the day’s routines, and usually left towards the end of the evening program. I studied interactions with the intent of revealing the meanings behind the interactions. I also attended group sessions and discussed the group interactions with staff members and clients separately afterwards. Staff also included me in their change of shift report, so I gained an understanding of the rationale behind some of their interactions with clients.
Although I took field notes, this process was hindered by the fact that I did not carry my field notebook with me. Prior to the study, concerns were raised that the presence of the notebook would hamper communication. It was agreed that I would observe and then go to an office to write observations. However, in this small center, private space was very limited, making this process more difficult. The lack of private space and the difficulty it imposed on the study process was one barrier that I reflected on. This led me to explore how the women who had even less private space and time were affected.
In-depth interviews
A semi-structured interview guide was used to seek information about how the women’s help seeking had brought them to this place, the history of their IPV, PTSD and alcohol dependence and their impression of the treatment center, interventions and the staff. These questions were shared with the informants at the beginning of each interview and were used with flexibility, such that the informant shared her experiences and I sought depth and clarity by asking probing questions.
Focus groups
In the final period of data collection, two focus groups, one for clients and one for staff members, were held to share a draft of the findings, to obtain feedback on the researcher’s understanding and to seek input about how the findings should be disseminated in the local community (i.e. to whom and in what format). Although all key client informants were invited, only five attended. However, all 25 staff members attended their focus groups. Nominal group technique [65] whereby each person has an opportunity to contribute was utilized at the closing of each focus group.
Analysis
NVivo8 software was used to index the data. Coding of the data was first completed using an ecological template in order to classify and describe the personal characteristics of the women and multiple systems of environment [66]. A second coding scheme was inductively developed to address each research question so that the data could be grouped into large files and studied for patterns and relationships. Although the analysis is described in phases, in reality, it was quite fluid, moving back and forth between descriptions, coding and interpretation, with all analysis influencing subsequent analyses. Data analysis proceeded from coding of individual cases, to comparisons across in order to identify and validate the emerging themes.
Authenticity
Authenticity was addressed by providing evidence that I remained open to the voices of the participants through informal interviews, second interviews and the focus groups. Providing diversity in the sampling of the informants and supporting interpretations with informant’s statements also adds to authenticity [62,67]. Verbatim transcriptions of the interviews and field notes were kept as an audit trail [59] and I maintained a reflective journal. I returned to data sources (either transcripts or informants) when questions arose within the analysis [62]. The process and the product and I were supervised by a group of experts who read the transcripts and reviewed the coding.
Findings and Discussion
Six main themes were identified from the data during the residential care. These are a place of sanctuary, living with the structure and the rules, understanding and handling of trauma, the spiritual nature of the program, the primacy of the group and the value of personal experience. Although these themes are described in separate sections, they intertwine and influence each other. The discussion is woven into the findings to present a more integrated perspective.
A place of sanctuary
This residential center could easily be missed as one drives along the highway. There was a one-word name on the mailbox and a discreet, small white sign a few feet back from an unpaved driveway that went behind the woods. Off to the side of the driveway were two inukshuk (an Inuit rock structure that is used to mark a path) that provoked a sense that someone has gone before and left a beacon of hope for a successful journey. Beyond the trees was a small country house with a blue van. The backyard had picnic tables and further back, wooden bench swings. On one side of the door was a birdbath with a statue of Saint Francis, and on the other, a stained-glass window of an angel.
Inside, the house was old but warm and inviting. Seldom was anyone completely through the doorway, when a woman would peak her head around a corner saying, “Hi! How are you?” and if she didn’t know you, she introduced herself. The kitchen was clean and filled with appetizing smells as the meals were cooked on site.
Next to the kitchen was an area where staff members had their meals. Behind this room was a doorway that opened to the sleeping area with a single bathroom and four bedrooms; three of these had two twin beds and a fourth bedroom had four twin beds. Each room had a dresser with drawers that locked and bedside tables.
Across the hall from the kitchen was a large room where most of the group sessions took place. It had long rectangular tables; gray padded chairs, a television with a video player, a white board, a flip chart and the beautiful stained-glass angel. At the back of this room were supply cupboards and a bathroom. The walls were filled with posters that convey messages about the core tenants of the center. A flip chart listed the Group Goals, such as No cross talk; No gossip; Be open to feedback and change. A poster listed feeling words such as: anxious, depressed, happy, etc. There were also 12-step logos on the wall such as: Let go and let God; One day at a time and a plaque that read: Dance like there is no one watching; Sing like there is no one listening; Love like you’ll never get hurt; Live like there is heaven on earth.
At the back door were stairs going down to a large open room furnished with sofas and chairs. Unless it was group time, a few women were usually sitting here, talking or doing their homework. There were many doors leading to offices, bathrooms, and a small kitchenette where both clients and staff make tea, coffee or get a glass of water. Behind this room was the laundry area with a washer, dryer and shelves.
Such a bland description does not do the center justice, as on its freshly painted walls were displayed the values of the center, not in a mission statement, but in artwork and plaques that were gifts from previous clients simply signed Cycle 76 or Cycle 8 and the women’s first names. These provided a reminder of the spiritual nature of the center. There were also bulletin boards that contain the schedule for the week and other notices, including the one notifying the clients of this study. Clients appreciated the comfortable and inviting atmosphere. One commented, “It is a house and it feels like a home. It is a warm and welcoming environment. There is time for yourself, even if it’s only an hour and you can do what you want then, and they treat you graciously.”
This center began as a dream of four women who were in long-term recovery from alcohol dependence and who believed that women required a treatment center separate from men. They established a board of directors and worked with the local governmental agencies to make their dream a reality. The center was sobriety-based and followed a 12-step model. They offered residential treatment for a period of 24 days, aftercare for 24 months, outpatient services, an early childhood development program and educational sessions. During the 24 days in residence, the first 3 steps of the 12-step program were dealt with in detail. These steps are:
• 1) we admit that we were powerless over alcohol and our lives have become unmanageable;
• 1) we admit that we were powerless over alcohol and our lives have become unmanageable;
• 3) make a decision to turn our will and our lives over to the care of God, as we understood him [68].
Admissions came in on the same day and were scheduled one hour apart to allow time for each new client. All were welcomed with a hug by staff. On their bed was a welcome letter from the previous occupant, addressed to “Angel #1” for bed one, etcetera. These letters started something like, “Okay you are here now, so take a deep breath. I pray that you let the love and the healing power of this place lead you to where you need to go.”
Living with the structure and rules
The program was highly structured, the educational content was heavy and there were multiple rules. This was intentional as the program organizers felt that, in the early days of sobriety, people need to keep busy [69]. The days were booked with educational sessions, program videos or occasional physical activities such as swimming or yoga, with half hour breaks inbetween the sessions. During the stay, there was no TV, radio or newspapers and the clients were permitted few telephone calls. Clients had about one hour of individual time each day when they completed their chores around the house, wrote in their journals, went for a walk or just relaxed. Women were in their rooms at 10:45, lights were turned out at 11:00 pm, and the new day began at 7:00 am. Morning and bedtime routines took patience and cooperation, as there were only three bathrooms and 10 women. There was a schedule for showers, baths and the laundry, as water was at a premium.
As the women arrived, they were orientated to the basic rules of the house. They spent most of the first day meeting the other women, feeling nervous, and learning the rules and routines. For example, the meal time routine included setting the table, eating together, saying grace before meals, participating in mealtime discussions, spending at least 20 min at the table before being excused, asking to be excused and clearing up the table.
There was concern from some staff that the number of rules and staff reminders of them set the stage for a parent-child pattern of communication that might have many unpleasant associations for clients [70]. Some also feared that reminders from staff members might trigger PTSD symptoms. In contrast, others reported that when women’s responses to the rules brought forth issues from the past, they could be addressed in a therapeutic situation. This is an area where staff required training and supervision in handling, not just unpleasant reminders, but also flashbacks from trauma experiences. However, staff education about responses to trauma was not provided. While other staff members raised concerns that too many rules did not empower clients to move forward, others argued that there is nothing more empowering than being clear from a chemical on which you were dependent.
Some of the clients had difficulty with the rules. Even getting up early in the morning and being on time for meetings was a challenge for some. The pressure of the group and their own motivation for coming usually helped them conform, or, if not, they left the program early. However, in the four months of the study, only one woman left for this reason. Most of the women liked the rules because it gave their lives order and predictability that was not previously present. One woman wanted more rules, explaining that procedures for such things as dish washing should be described explicitly and not left to individual judgment. The group confronted women who broke the rules or did not do their chores, which provided an opportunity for discussion within the peer group.
Residential treatment for alcohol dependence is intended to be a corrective experience for clients [58] and it is clear that the women in this study saw this treatment center in that light. However, as warm and loving as all the staff were, tension between staff members regarding the main principles of the program were evident. Still, despite the staff having varying views about the rules, most clients seemed to obtain comfort and security from them. Structure and predictability in the early stages of recovery are important, decreasing anxiety for the clients and allowing them to focus on self-care and selfexploration [58,71].
Understanding and handling of trauma
The key informants all scored between 5 and 12 on the SPAN test and reported PTSD symptoms, which included flashbacks, startle reflex, social anxiety, panic attacks, numbness, feeling different from other people and being unable to have any emotion, unless they had been drinking. Interestingly, most had no understanding that these symptoms might make recovery more difficult. When asked, women responded that they knew of nothing they could do when these symptoms occurred. In many cases, women reported that they drank to control these symptoms. Avery described her inability to have loving feelings as a difficult symptom. “It is the loving feelings that I am unable to have; I make jokes about myself being like the tin man.” Another woman’s nightmares forced her to relive her beatings again and again, “I am very sore, and I had terrible nightmares all night, last night. I woke up and I felt like my body had just been beaten.”
Staff members were briefed about women’s trauma histories in the preadmission conference and, in fact, many had experienced violence in their own lives. When asked about their understanding of PTSD, most staff members admitted to having no understanding and commented that this had not been part of their education. One staff member stated that she did not have an academic understanding but gave the following description from her personal experience:
“A traumatic event occurs. The individual, or I, is left with anxiety, fear and a sense of not being safe. I am not safe in the world, so I need to be careful. There is a sense of always looking over your shoulder, because something is coming. I don’t know what is coming, but I know something is coming. There is a startling effect. I am startled easily, and now I don’t trust, I don’t trust the world. When I am navigating myself throughout the world, I have to judge what is safe and what is unsafe. I don’t know, so now I am always in navigation mode. I have to figure everything out, so that I am never quiet. I am never at peace. I am hypersensitive…and because of that, in order for me to navigate in a way that is bearable, I now stop living from the neck down. I have to get out of my body because it is unbearable. When I say I stop living in my body, it is because if I move into my body, I feel everything. If I get out of my body and stay in my head then it becomes bearable for me. I don’t have to navigate so much and now I am free to just engage in the intellectual experience of my world.
What happens then is that I will become startled and I will be forced into my body and when I am forced into my body, I am in panic mode, so I have to go quickly back into my head. It is very hard to engage me because I am constantly defended. I now live with this bubble around me and it becomes very hard to get to me. Not only is it hard for you to get to me, but also it is hard for me to get to me. I am in this huge plexiglass bubble. No, I guess it would be more like steel; it is like a jail that you can’t get out”.
Hearing this, one can appreciate the value of personal experience in understanding PTSD at a very visceral level, yet staff members did not have an understanding that is based on current knowledge and, consequently, did not address these symptoms as part of the treatment plan. This description also describes the difficulty that some women with PTSD have with relationships, even relationships with themselves. The extent, to which the PTSD symptoms interfere with relationship development and maintenance, varies from person to person, as do the other PTSD symptoms; however, this would have a direct influence on their ability to seek help.
Staff members were not directed to observe for and assess PTSD symptoms. Thus, when symptoms occurred, they sometimes reframed these as post-acute withdrawal symptoms (PAWS), which they are taught to look for. When a recovering person is in a highly stressed state, she or he may suddenly show confusion, loss of emotional stability, and memory impairment and this is called PAWS that is managed by structured living, eating well-balanced high protein meals, and avoiding excessive amounts of sugar, caffeine and nicotine. These symptoms vary in severity and are directly related to the amount of central nervous system damage from the alcohol. However, there is a direct correlation between episodes of PAWS and the risk of relapse. The symptoms of PAWS bear a resemblance to some symptoms of PTSD, especially the confusion and memory impairment. Moreover, since PAWS escalates anxiety, it could possibly act as a trigger for PTSD. The problem with confusing these symptoms is that PAWS will subside in time without intervention [72] while PTSD may not and, in fact, may escalate.
An example of the misunderstanding of trauma and its sequelae was demonstrated in one group. A client was given a Styrofoam bat and asked to express her anger while she beat a chair. This client and others in the group had difficulty engaging in and witnessing this act. For women with a history of violence, their response is understandable. Venting anger was previously thought to diffuse anger and aggressive tendencies. However, more recent research has found that the opposite is true [73]. In this same group, the client expressing the anger was cautioned not to provide details about what caused her anger but only to express her feelings about it. The explanation given for this approach was to not traumatize other members of the group. In fact, this approach seemed to retraumatize the person attempting to diffuse anger in two ways:
• 1) by saying what happened was so traumatizing that hearing about it would traumatize others, and
• 2) by silencing her experience, reinforcing her shame and the need to keep it secret.
This approach was not effective as the clients heard the details after the group without the counselor’s presence. In this case, the peers provided support so the client was able to grieve.
Women with alcohol dependence and PTSD symptoms require emotional support and coping mechanisms to maintain their sobriety and to deal with PTSD symptoms [70]. Most of the time, these symptoms do not dissipate on their own and some of these symptoms may interfere with their ability to get help or even get to an AA meeting for example social anxiety. Despite their symptoms, clients showed little understanding of PTSD and the impact it might make on recovery. They tended to blame themselves for relapsing rather than review what might contribute to the relapse, further impeding their progress. Lynn, like the other clients, sensed from the staff that traumas and life problems should be set aside to be dealt with at a later time. She reaffirmed this idea after a group meeting, “I am here to work on the addiction and I want to concentrate on that. That's what I'm here for, but those other things that come up in my memory. It's like; I start then I disconnected then I shut it down.” This is an example of memories being triggered, and the client suppressing them rather than dealing with them in the therapeutic situation. Suppression reinforces PTSD symptoms. If staff were informed about women’s responses to trauma, other mechanisms could be put in place so that these moments could be transformed into therapeutic opportunities where women could share their experiences and develop new coping skills. Staff did, however, recognize that because of the extent of trauma, some clients required more treatment time than others. Susan, a long-term staff stated, “Sometimes the most difficult time for me is when a client is so defended and is just getting started when the 24 days are up and we have to send her out whether she is ready or not.” All staff and many of the clients felt that the program should be longer, especially for women who had extensive trauma in their lives. It is concerning that, although there is recognition of the violence in the lives of the clients, there is nothing formal in the program that directly addresses that trauma. This suggests that there is little understanding of the intricate connection between these two areas.
When they leave the treatment center, some clients may return to an abusive partner, yet during the four months of the study, the researcher never heard anyone review a safety plan with a client who was preparing to leave. The women who came received help with their alcohol dependency but not with their PTSD or their IPV, two conditions that may be strong triggers for relapse. These conditions are so intertwined that they can no longer be considered secondary to alcohol dependency [6,42]. Lack of attention to these conditions not only interferes with the client’s ability to remain sober but also very likely limits her ability to ask for help or talk about the trauma. In some situations, the women were left alone with their nightmares and memories of the past; even if they were sitting in a group, if they were not talking about their fears or nightmares, they were still alone.
The spiritual nature of treatment
The care in this center revolved around spiritual awareness, acceptance and expression through daily practice. Unlike traditional religious dogma, there was an emphasis on angel’s messages, nature and the spiritual power of groups. Some staff members believed that one of the founders was a native healer and that she chose the property because of the healing energy of the ground. Others believed that the place became spiritual and becomes more so every day because of the healing that has occurred since the center was established.
The notion of spirituality was introduced early; it permeated the grounds and the house and in the first group, a staff member mentioned that this was a spiritual place. She talked about the day she first arrived as a client and how she felt about the place. If clients felt tense or uneasy, she encouraged them to step outside for a few minutes, take a few breaths of fresh air and try to feel the special vibrations of the place, or just appreciate the beauty. The spiritual focus was woven throughout the program. Groups and educational sessions ended in the Serenity Prayer, grace was said at all meals, there was morning and evening meditation and the content of the education program focused on the understanding of the first three steps of AA that demanded a reflection and a dialogue about a higher power and the influence that has in one’s daily life. At times, the spirituality was hard for the clients to understand, particularly if they had little prior exposure to it in their personal life. Some were resistant because of previous negative experiences such as being taught only about an angry and punishing God. Others struggled with the concept of a higher power, because it was too ambiguous. One client, who was resistant, grabbed onto the idea that the higher power could be open to various interpretations and proclaimed that the ladybug on the windowsill was her higher power. Others were offended by this and several sessions were needed to resolve bad feelings and misunderstandings evoked by this remark. Despite incidents like this, most of the clients valued this component of the program. One young client stated:
“I’ve been cursing God for many years because I was so frustrated with my life. But I didn’t know what spirituality was; here you have the freedom to believe in what you can. It makes a world of difference, Now, I always have someone to talk even if I can’t see them and I have had my moments, little moments, and I’ve never before had that in my life, so it’s just wonderful. This place has totally changed my life”.
A counselor who was a former client also reflected on her understanding of the role of spirituality in treatment:
“I have my own personal stuff around the angelic stuff. I think it works for some clients, and I think others buy into it because they think they are supposed to. I think it brings a warm aspect to engaging women. It is loving and tells a woman she is special. I would love it if that could come from the client, not from us, not imposed by us. Love can be conveyed in just your presence. However, as a client, that part was very beneficial to me. It was very loving and I needed someone to love me because I hadn’t a clue how to do that myself. But when I look at it as a clinician, I am more critical”.
This demonstrates the value that the staff member placed on this aspect of the program, despite her inability to explain it from a treatment perspective. One of the possible dangers of relying too heavily on the spiritual component is expecting change to happen naturally and easily when recovery, even with spiritual support, is a difficult journey, where one has to commit to daily practice. Counselors also need to ensure they are offering the most current best practices. However, to move from dependency to a life of intentional sobriety demands a profound change in attitude and behavior that some people call a spiritual awakening.
A video [74] was shown where a priest talks about spirituality. He said that when most people think of spirituality they think of a vertical relationship between God and themselves, but that this is only part of the concept. There is another part, which is a horizontal relationship between the person and other people. He described how to develop those loving relationships with others. This video produced a change of perspective for some of the clients and stimulated reflection on the part of the researcher, then and during analyses. What was real for both the women and the researcher was the horizontal relationship and the experience of being valued by the staff members that led to a deep feeling of connectedness. This was a feeling that all women, even those who left early, took with them. The spiritual nature of the center was valued and supported by all staff members and many of the clients. With the view that spirituality can be expressed through relationships with others, the few clients who initially resisted the idea were convinced of its value for recovery.
Primacy of the group
The emphasis on connections with others leads to a natural belief in the primacy of the group. Although each client was assigned a primary worker, the emphasis was on the group. This focus fits with the objective of the program, as the staff members felt that the 12-step model is the best resource for women after treatment. Clients who had previous experience with AA meetings felt comfort being back. One young client stated, “Getting back into AA meetings was big for me. I had forgotten how much I enjoyed them, so I have that renewed joy”. The clients felt safer at the all-female meeting as they did not have to confront their conflicted feelings regarding men. These meetings are recommended for women in the early stages of recovery [58]. Clients who were new to AA were nervous about speaking but were appreciative of the other women’s sharing.
The cohesiveness of the group was enhanced by the same arrival day, lack of outside contact, closeness of the living quarters, the buddy system and the sharing of household responsibilities. Working together in this manner built on the group processes and easily got into routines of daily life that triggered their issues, thereby providing therapeutic opportunities. These issues were discussed in peer group that was held three times a week in which the staff facilitated clients in talking about group dynamics. The focus was on the here and now, I-statements, and containment, (i.e. getting the women to stay in the room and not leave when conflict arises, as their usual reaction was to flee from conflict). It is important for the clients to become aware of how they are affected by such conflicts and the influence it has on their feelings, cravings and use of alcohol. In the group, they also had an opportunity to try out different responses and to practice the new skills.
A buddy system was set up to counteract the isolation the women might choose. Buddies spend non-group time with each other, went on walks together and looked out for each other. Buddies changed each week, thereby acting as a deterrent to pairing and splitting the group and allowing the client to gain an understanding of the diversity of the women in treatment by hearing different perspectives. One client stated,
“I was afraid to talk about the lying and sneaky behavior, things that you’re ashamed of. But what I see here is a bunch of beautiful, good-hearted women who have those same problems.
You know, looking at them, I don’t think any less of them when they tell me those things.”
Sharing their story with a buddy helped women prepare for sharing their stories with the group. Hearing stories from others also helped them, because they were more forgiving of others and, as they forgave others, they became more tolerant of themselves. This increased their self-worth so that they trusted enough to share their secrets and, in turn, receive forgiveness. This buddy relationship provided the skills to build other relationships in the future.
Avery, who achieved her sobriety at this treatment center and maintained it through her involvement with AA, shared her understanding of the importance of the group:
“The most help that I got was through the experience with my peers. I thought that I was smarter than everyone else; I am not like you guys. I don’t do those kinds of things. I am like the counselors. So that kind of alienated me from the group and they called me on it. They said, “If you are so fucking smart why are you here?” So I started to cry. I had a problem, because I didn’t like being alienated from them, but I had done that to myself, because I didn’t know how to connect with them. It was suggested to me that I go back and tell them that I needed them. I said. “I don’t need them”, and my counselor said, “you do need them and I think that you might not make it.” So I went to the group and I remember sitting in front of the group and the break for me was telling them that I needed them, because I broke down. I had never told anyone that I needed them. That was the most therapeutic moment that I had right there. There I was telling these people that I had totally separated myself from that I needed them. I asked for help, it was offered and I took it. It was because of having to ask for help here that gave me the strength to ask for help later in the AA group. I was so beaten emotionally that I did not know how to live my life and get what I needed”.
At times the group was seen by the women as supportive and at other times, some women felt that they were being scapegoated within the group. It took very experienced staff members in-group work to help reverse this situation and to create a group where the women felt free to discuss in an open, honest and caring manner their issues with each other. However, these skills are important in order to prepare the women be able to function in post treatment recovery. Some women isolated themselves even in the presence of groups, because of stigma, shame, fear of rejection and not knowing how to ask for help. With the help of the staff, they were able to learn new ways to deal with their issues and ask for help. This group work, not only takes clinical knowledge but also expert supervision [73]. Although the center was advertising for a manager to do this supervision, the bare-bones budget did not allow sufficient funds to attract an expert group clinician.
The group process helped prepare the women to conquer many of their social fears and helped prepare them for 12-step groups and other treatment programs. However, is this enough if their trauma and their PTSD symptoms, particularly the social anxieties, are not addressed? The tradition in alcohol treatment centers is to consider the alcohol dependency primary and trauma secondary. However, the connection between trauma and dependency is so intricate that they must be considered equally. For this reason, researchers and clinicians have recommended a more integrated approach for treatment of dependence and trauma [6,42].
Value of personal experience
A cornerstone of early treatment centers was the hiring of persons in long-term recovery from alcohol dependence as the primary counselors [75]. The founders of this center followed that guideline, hiring women who were in long-term recovery and who were applying the 12 steps in their daily life. Three long-term staff members who were key informants in this study were invited to work at the center based on that criterion. They supplemented their personal experience with courses in addiction counseling and obtained certification. Recently, the center started to hire women who had been educated at the community college level as social workers or addiction counselors, but who had no history of personal recovery. This change of practice caused some tension among the staff. Those without personal recovery felt devalued and not appreciated as fully as staff with this history. This valuing of the, been there experience was also acknowledged by the clients. The experience of restoring a life of chemical dependence to one of intentional sobriety created instant credibility, quickly establishing trusting relationships, and provided an example of what life like this could be. Disclosure by staff members offered women hope that this could be possible for them. As one client stated, “the nature and the facilitation of the staff; the fact that they themselves have been in recovery, I think is amazing. Being certified as an addiction worker is nice but having gone through it is completely different. Having both is a bonus”. The staff who did not have the personal history realized that they needed to work harder to establish a rapport with clients but they also brought important skills and a desire to do this work. One young staff stated, “Personal recovery is not a counseling skill and I have lots of counseling skills that I can utilize with the clients that come into my care.”
The belief that experiencing and overcoming a dependency bestows certain powers to understand and heal others similarly afflicted is widespread within the addiction field [75]. The danger in this perspective is that directors of programs may assume that counselors have skills that they don’t posses, or that exist only on an intuitive level, and, therefore, cannot be used consistently or taught to newer counselors. This was evident in the staff’s ability to intervene so superbly yet be unable to articulate their intervention techniques.
Certainly, recovering staff could challenge clients about their ploys and avoidance with more credibility than other counselors. One client remarked on this ability:
“The positive bluntness of the counselors I think is imperative; at least it was for me. I had to have them looking me straight in the eye and not moving their gaze when they challenged me, otherwise it would have just rolled off my shoulders. And to have those emotions moving from your chest up to your heart, where you feel it and up to your mouth where you speak it was very difficult and they make me feel safe here, emotionally, absolutely 100% safe”.
In this type of counseling, more use of self, and more selfdisclosure is required than other counseling might utilize [76,77]. With the high relapse and mortality rate in this field, staff must also protect themselves and be able to absorb losses without losing hope. Considering these elements, clinical supervision in this field is critical. All of the staff wanted good supervision and recognized that they and their clients suffered when it was not there. Although a few staff talked about ways to disengage emotionally, most seemed to thrive on intense heart to heart interpersonal group and individual work. Grace, a recovering staff member, who had worked at the center for 15 years said,
“It is very gratifying. I feel somewhat privileged to be able to do this work. I can’t think of a better way to make a living than serving others in this way. I know that the reason that I gravitated to this work is because I was looking for deep meaning and purpose in my life, for something meaningful, some kind of work that came from the heart, that connectedness, heart to heart, that’s a huge piece of why I do this”.
Susan, another staff member stated, “It is fantastic to work here actually watching women’s lives change, actually witnessing and being part of something important, real and purposeful.” This idea of witnessing was stronger for counselors with a personal history of addiction. They seemed to have faith in unseen forces outside of the therapeutic relationship that guided and sustained the clients. Perhaps this is because of the role that spiritual awakening had in their recovery. The person in long-term recovery from substance dependence is living proof of the hope that recovery is possible, as Lynn stated,
“I like the staff; I think they're wonderful when they share, and they say, “I’ve been an addict or an alcoholic. They are right up front. I find that hopeful. It gives hope for me. Somebody that's been through it, understands what it's like, understands what I'm going through right now”.
This testimony and proof of change not only had a powerful impact on the clients and their families but also provided enduring hope for their fellow counselors.