Research Article - (2015) Volume 23, Issue 3
Western Australian Centre for Rural Health, University of Western Australia, Geraldton, Western Australia
Emma Haynes
Western Australian Centre for Rural Health, University of Western Australia, Crawley, Western Australia
Shaouli Shahid
Western Australian Centre for Rural Health, University of Western Australia, Crawley, Western Australia
John A Woods
Western Australian Centre for Rural Health, University of Western Australia, Crawley, Western Australia
Tiew-Hwa Katherine Teng
Western Australian Centre for Rural Health, University of Western Australia, Crawley, Western Australia
Patricia Mary Davidson
School of Nursing, John Hopkins University, Baltimore, Maryland, United States
Judith Masha Katzenellenbogen
Western Australian Centre for Rural Health, University of Western Australia, Crawley, Western Australia
This paper explores some of the history and rationale for the Aboriginal Community Controlled Health Services (ACCHS) model of service delivery, and why it is difficult to compare their effectiveness directly with that of other primary health care services in Australia. ACCHS were pioneered over 40 years ago. Since then, they have been established across Australia as a model of primary health care to meet the needs of Australia’s disadvantaged Indigenous population which had been underserviced within mainstream health services. ACCHS are managed by Aboriginal boards, promote a model of holistic and comprehensive primary health care and are largely funded by government. Over recent years, additional funding has gone to ACCHS and mainstream services in an effort to close the gap in Aboriginal life expectancy. In this context, the authors were commissioned to examine the peer-reviewed literature to explore the question of the relative effectiveness of ACCHS compared with other primary health care services. In responding to the question, we were led to consider the historical experience of Aboriginal people, their social and economic disadvantage, the geographic distribution of Aboriginal people where there is market-failure of general practice, the predominant model of primary care in Australia, the complexity of Aboriginal people’s health needs, and the limitations of peer-review studies. We argue that the provision of effective health services requires that they are accessible and attentive to the needs of their client, not just that they deliver evidence-based medicine. Services exist on a performance continuum, so quality improvement approaches with appropriate measures of quality to assess performance for Aboriginal people are needed. We argue that partnerships between ACCHS and mainstream health care providers are essential to improving Aboriginal health outcomes given the complex nature of modern health care and the myriad of health and social problems experienced by Aboriginal people.
Aboriginal, Indigenous, health services, primary care, performance, quality, effectiveness
ACCHS-Aboriginal Community Controlled Health Services, AMS-Aboriginal Medical Service, QAIHC- Queensland Aboriginal and Islander Health Council
‘How this fits in with quality in primary care’
What do we know?
We know that the health outcomes of Aboriginal Australians are poor compared to the general population and that the major causes of health disparities arise from premature chronic diseases that are amenable to health interventions. Aboriginal Community Controlled Health Services are holistic primary care services established as a response to addressing Indigenous Australians health care needs to address health needs not being met by mainstream health care providers. However, governments invest in health care and want to know the relative effectiveness of different models of health care delivery
What does this paper add?
This paper explores the multiple reasons for why it is difficult to compare quality and relative effectiveness between different primary health care models given their different patient populations and areas of operation. It argues that delivery of high quality primary health care requires access to different and specialized services and that improvement approaches and use of a broad range of indicators are needed to assess service quality and outcomes rather than assessment based on a restricted range of biomedical indicators. There is an important role for service partnerships between Aboriginal primary care services and mainstream services to deliver effective health care to Aboriginal people
Although Australia has much in common with other developed countries with a past history of colonisation, it has a poorer record in terms of the health of its Indigenous minority groups, Aboriginal and Torres Strait Islander * people. Efforts to improve their health outcomes require action at the level of the social determinants of health but also access to good primary and specialist health care. Over the last few decades, there has been acceptance of the wrongs inflicted on Aboriginal people in the past, including as the result of misguided benevolent actions of government, and acknowledgement of the principles of self-determination. This has included endorsement of Aboriginal Community Controlled Health Services (ACCHS)** by Aboriginal communities and health service providers as well as in policy.
In mid-2013, we undertook a commissioned review aimed at exploring peer-reviewed published evidence on the relative effectiveness of ACCHS in Australia compared with mainstream health services and assessing the quality of the evidence.[1] The literature review was presumably commissioned because no previous critical and systematic review of the relative effectiveness of ACCHS compared with mainstream primary health care services had been undertaken and because of the commissioning agency’s commitment to improving Aboriginal health within constrained resources. Our interest in this assignment related to the potential for exploration of the concept
* For consistency we use the term Aboriginal Community Controlled Health Service (ACCHS) to refer to any of the various terms applied to these services, e.g. Aboriginal Community Controlled Health Organisation (ACCHO), Aboriginal Medical Service (AMS). We use the term Aboriginal to refer to people of Aboriginal and Torres Strait Islander descent, and in place of the term Indigenous.
** For consistency we use the term Aboriginal Community Controlled Health Service (ACCHS) to refer to organisations that are often described using other terms: Aboriginal Community Controlled Health Organisation (ACCHO) and Aboriginal Medical Service (AMS). Aboriginal Medical Service is a term historically and is still often used to refer to Aboriginal health services but does not necessarily imply control through an Aboriginal community board of effectiveness in health service delivery for Aboriginal people, a diverse underserved minority population which experiences disadvantage across many health and social indicators. At face value, it seemed that a scoping review of published papers and what was missing could help inform thinking about the nature and type of research and interventions that are needed to improve the effectiveness of service delivery.
Reasons for caution in accepting the task included our knowledge of this as contentious and politically contested space. We were also aware of the fundamentally very different aims, approaches and contexts of the services provided by ACCHS compared with other Australian primary health care providers, and mindful of the politics and perils of poorly conceived assignments.[2] The task was to identify and review a literature that made comparisons between inherently different services, that is, between services that operate in different circumstances, for a different population group and which have different criteria of success.
This paper considers the many limitations that arise from deeper consideration of the question of the relative effectiveness of ACCHS. It does not report the process, the framework or the findings from the review of literature. Instead, it provides a brief background on ACCHS, and argues that there are fundamental differences in aims and context of ACCHS and other primary care services that render making comparison problematic. The analysis has relevance for consideration of services for other indigenous populations and could also help with conceptualising the place which ACCHS offer in the Australian context and thinking around improving health care for Aboriginal people.
Putting Aboriginal Health in Context
It is essential to put the health of Aboriginal people into the context of socioeconomic disadvantage. There is overwhelming evidence that the distribution of wealth is the main determinant of the health of populations, with ill health more prevalent among lower income earners.[3-5] The equivalised mean gross income per week for Aboriginal households in the 2006 census was $460 and for non-Indigenous households $740; this much lower income impacts on access to quality food, housing, and health care, all of which are important in overall health and wellbeing.[6,7] Aboriginal people collectively have multiple social disadvantages aggregated across many domains—health, disability, housing access, income, justice, and education. The persistent gap in Aboriginal health outcomes underscores the link with these elements.[8]
However, explanations of poor health and health inequality restricted to these broader ecological determinants may result in health system factors, including those related specifically to primary health care, being overlooked.[8] Aboriginal people have had poorer access to primary health care for a long period, particularly when their worse health status is taken into account. One key contextual barrier relevant to accessing health care for the Aboriginal population is the continuing impact of past practices, often summarised as ‘colonisation’ referring to the collective subjugation and abuse of human rights which Aboriginal people have suffered since white settlement. Often manifesting as distrust in government agencies and non- Aboriginal people, this contributes “to high levels of stress among Indigenous people...an important barrier to accessing health care and…consistently associated with adverse health outcomes for Indigenous people”. [9]
Putting Primary Health Care in Context
It is accepted that primary health care is essential to the health and wellbeing of the community. Effective comprehensive primary health care supports health promotion and health education, enhances service access (particularly for vulnerable individuals and groups), facilitates timely diagnosis and treatment, and also enables the management of chronic and complex conditions in the community.[10,11] Increased availability of good primary care reduces health care costs in populations, and can reduce admission to hospitals, which provide care that is different in nature and more costly. [8,10] It has also been shown that groups of individuals using primary care as their first source of care have lower health expenditures than others. [12,13]
This has been recognised by successive Australian governments which have reiterated commitment to primary health care. The Australian Minister for Health at the time when the review was commissioned had stated:
“Primary health care is critical to Australia’s health system because it helps to keep people well and out of hospital. The better we are at primary health care, the better for patients and for our system … Research shows that good primary health care can reduce the need for medication and reduces hospital admissions by up to 25 per cent. The evidence also shows that countries with health systems built around strong primary care get better bang for their health buck”
The predominant model of primary health care delivery in Australia, a large country where the majority of the population lives in cities based on or near the coast, is general practice which is characterised by private business ownership and feefor- service remuneration. However, a ‘tyranny of distance’ contributes to market failure in primary care delivery, with rural, remote areas and some outer urban areas less attractive to health providers. The diseconomies of scale which result from large distances and small dispersed populations have been particularly evident in areas where Aboriginal people constitute a greater proportion of the population.[14] The low doctor-to-population ratio in these areas potentially compounds a situation where doctors are already under disproportionate pressure dealing with patients and circumstances that are more difficult and stressful. [15] The consultations needed to deal with the physical and psychosocial problems that Aboriginal people experience at a higher rate means that standard general practice/mainstream models are poorly suited to improving the care of Aboriginal people.[16,17] For doctors, dealing with the whole person within their complex social context diminishes remuneration compared with consultations in which one or two clinical problems are managed in isolation.[18,19]
Health care practice is challenged by the contradiction between a ‘market driven’ health care environment based overwhelmingly on fee for service in primary care and the espoused values of person-centred practice.[20] There was recognition of this in Australia’s First National Primary Health Care Strategy:
“[f]or many individuals, the primary health care services they access and the quality of care that results has depended on where they live, their specific condition, and the service providers involved, as much as their clinical needs and circumstances. Many patients, particularly those with complex needs, have either been left to navigate a complex system on their own or, even when supported by their GP, have been affected by gaps in information flows, and a limited ability to influence care decisions in other services… Primary health care is strategic, focusing on equity, access, empowerment and intersectoral partnerships as essential elements for maintaining health”.[21]
The origin and development of Aboriginal Community Controlled Health Services
Pioneered by the Aboriginal community, ACCHS have become a targeted initiative by Australia’s Federal Department of Health to meet the needs of the most disadvantaged, socioeconomically and most geographically isolated Australians by an increased focus on locally planned and delivered services which improve accountability and responsiveness.[22] As a reflection of the aspirations of Aboriginal people for selfdetermination, the first community-controlled Aboriginal Medical Service (AMS) in Australia was established at Redfern in 1971 by Aboriginal community activists, with an aim to improve access to health services for local Aboriginal people by creating a culturally appropriate environment. The initial catalyst for the establishment of this service and other ACCHS was the failure of mainstream services to meet the needs of Aboriginal people, and their initial establishment was by volunteer health staff working with Aboriginal community leaders without any government funding. A hallmark of these early days was the providers’ commitment to working with and supporting Aboriginal people in their aspiration to have access to services able to meet their health needs in a culturally appropriate/safe manner. As Marles (2012) wrote, “[back then] Medicare did not exist and the only option for most Aboriginal and Torres Strait Islander families living in inner Sydney was to attend an emergency department or rely on the goodwill of local general practitioners. Many Aboriginal and Torres Strait Islander people experienced racism in the health system and wider community, and poverty was a major barrier to attending general practice or purchasing medicines.” [23]
Within a year of opening, the AMS at Redfern became so popular that it was unable to meet the demand for its services. Federal government funding was allocated in the following year, and since then, the number of ACCHS has increased markedly, so there are now over 150 Australian government-funded ACCHS in Australia. [23] ACCHS themselves have become incorporated and sizeable organisations, some with substantial budgets and receiving considerable government funding for the services that they deliver. Substantial diversity exists within the sector in terms of infrastructure, funding, governance structure, staffing and resource allocation, and consequently in the range of services offered. [24] ACCHS are governed by Boards of Management elected from the local Aboriginal community. Many ACCHS operate in areas where private practitioners are reluctant to establish a practice, however, there is evidence supporting the model of primary care provided by ACCHS in rural and remote areas. [14]
In accordance with the paradigm of primary health care and Aboriginal community control, ACCHS advocate a philosophy of community-initiated and -led solutions to the socio-political and economic conditions that need to be addressed, while delivering essential health care to Aboriginal people in a manner that prioritises holism, comprehensiveness and cultural appropriateness.[10,16,17] ACCHS provide treatment for clients with complex physical and psychosocial issues who often lack the education, health literacy, resources and networks of influence that many other Australians have as a result of being more affluent, better-educated and residing in areas with greater access to support and resources. The aspirational aim of ACCHS is to provide comprehensive primary care, including medical, dental, public health and outreach services. Locating a primary health care service within a community also provides context that facilitates activities beyond individual patient care, including quality improvement and population health programs, benefiting the community and enhancing service capacity.[25]
Doctors working in ACCHS must “engage in empowerment strategies with Indigenous patients, ... a big part of the job is advocacy on behalf of patients, helping them to negotiate parts of the health system compromised by institutionalised racism”.[19] The work of doctors is complemented by multidisciplinary teams; in particular, Aboriginal Health Workers, whose knowledge of both the cultural and social aspects of a patient’s background assists with patient management, including communication with visiting specialists and allied health professionals.
However, factors can also affect or compromise the ability of ACCHS to provide effective services. Effective healthcare for those with different belief systems may also be challenged by exclusive use of treatment modalities from a Western medical model, even within ACCHS.[26] Doctors employed by ACCHS across Australian are predominantly non-Aboriginal, and many are international medical graduates who experience challenges working cross culturally, often in rural and remote settings.[27,28] This is compounded by the health and social difficulties faced by Aboriginal people, so that medical consultations within ACCHS involve challenges because of the number, complexity and interaction of problems presenting simultaneously, potentially further complicated by subtleties in communication. Additionally, primary care services need to interface with the broader health system, but effective interfaces between tertiary services and primary care are still often underdeveloped. Only recently have large hospitals been attentive, often in a limited way, to the needs of Aboriginal people and to ACCHS as significant providers of primary health care services to Aboriginal people.[29] This has undoubtedly compromised optimal follow-up and management in primary health care following admissions for serious illness.
Evaluating effective health care in the Aboriginal context
The definition and measurement of effective health care can be contentious and inherently dependent upon context. Thus, what is considered “best practice” in a predominantly white urban setting may not be best practice in a different setting with a different community.
Furthermore, our understanding of what is effective has changed over time, with formal appraisal of health services effectiveness being a relatively recent phenomenon. Considerations of effectiveness are inevitably intertwined with those of quality, safety and efficiency. Donabedian, the “grandfather” of health service quality critique, in 1966 published a framework for assessing quality across the health care system and in a range of settings; this was based on structures and processes contributing in an orderly and linear way to achieving outcomes.[30] The framework resulted from the need for a greater emphasis on quality and safety, as health services had become more sophisticated, complex and expensive. Further understanding of the determinants of health care and outcomes has since emerged, with recognition of additional important determinants of the quality of care redundant. These include patient characteristics (including genetics, socio-demographics, health habits, beliefs and attitudes, and management preferences); broader environmental factors (including the patient’s cultural, social and political context); and factors related to the health profession itself, an element now considered to have been inadequately incorporated into Donabedian’s original framework.[31] These factors are now recognised as making a significant contribution to poor health and are often very different in the settings and populations in which ACCHS operate from those in general primary health care.
In the context of modern medicine, effectiveness may be considered to be related to the delivery of evidence-based health care with its emphasis on the use of evidence from well designed and conducted research in healthcare decision-making and delivery. But effective health care delivery is more than just prescribing evidence-based treatments. For example, Murray has argued that the concept of performance centres around three fundamental goals: improving health, enhancing responsiveness to the expectations of the population, and assuring fairness of financial contribution so that improving health means both increasing the average health status and reducing health inequalities.[32] And for the individual patient, an effective health system has been argued to be one which “provides timely access to the full array of needed services, efficacious and safe care leading to improvement in health, continuity of care, and respect”.[33] Whatever definition is used, the challenge of how to measure, monitor, and improve the effectiveness of agencies delivering care to Aboriginal people is central to the question of the relative effectiveness of ACCHS.
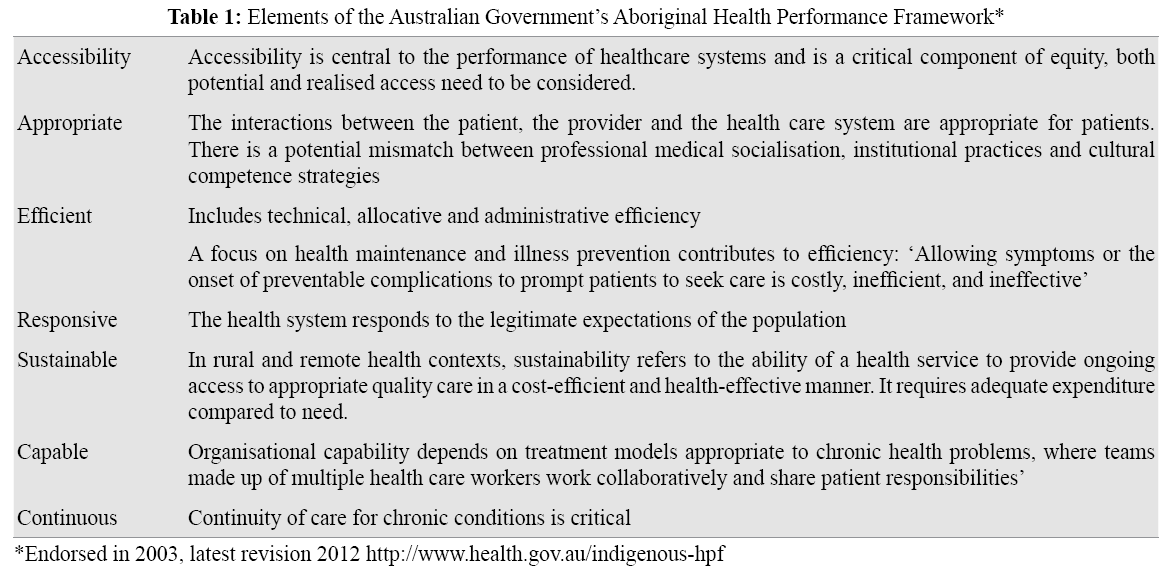
Consideration of effectiveness must also consider the funding and performance signals provided to ACCHS. For the last decade, Aboriginal health performance and improvement has been underpinned by the Australian Government’s Aboriginal Health Performance Framework (endorsed in 2003, latest revision 2012 https://www.health.gov.au/indigenous-hpf), a conceptual framework that supports a system-wide approach to performance measurement aligned with nationally agreed strategic goals.[34] The framework identifies specific indicators for each component of effective care, essentially defining its elements – that services should be accessible, appropriate, efficient, responsive, sustainable, capable and continuous (Table 1). Within this nationally endorsed policy framework with multiple elements, it could be asked how well the broad range of other primary care services performs against each of these components of effectiveness, many of which will favour ACCHS over other primary care for Aboriginal people.
Accessibility and trust are critical to effective primary health care for Aboriginal people
Accessibility is central to the performance of healthcare systems. Given the treatment of Aboriginal people historically, as well as in recent and contemporary Australia, many Aboriginal people have a distrust of government institutions including health services, so the issue of trust looms large in the provision of health services for them. No matter how caring the individual doctor or other health practitioner, it is the patient’s experience of their encounter within and their trust of the health service overall that will affect their willingness to attend, their adherence to the advice they receive and re-attendance. This trust depends in part on health providers being aware of the historical and ongoing background to Aboriginal health and its impacts on Aboriginal patients, as well as how their own cultural background, privilege, assumptions and values impact on how they relate to people.[29,35] Barriers to Aboriginal people’s access within mainstream primary care can occur in multiple ways, including cultural security, communication, financial barriers and service availability.[36-38]
Patients are often left to navigate a complex system on their own and have been “affected by gaps in information flows, and a limited ability to influence care decisions in other services”; these are issues that particularly affect Aboriginal people given their complex care needs.[21] This diminishes continuity of patient care, which is an important factor for improving health outcomes and a hallmark of good and effective primary health care. Personal continuity not only improves individual health outcomes, but also saves the health system money and appears to have even greater importance to vulnerable populations who in turn have greater difficulty achieving it.[39,40] An environment dealing with patients with complex care needs requires access to different and specialized services and this highlights the important role of service partnerships between Aboriginal primary care services and mainstream services to deliver effective health care to Aboriginal people.[41]
Limitations and biases of evidence from peer-reviewed publications
While the prioritising of peer-reviewed publications in examining evidence is established because of the relative rigour to which authors’ claims are subjected, we were concerned from the start about the limitations of this approach. It is well known that there is considerable suspicion among some Aboriginal people of research.[42] Research and publishing in peer-reviewed journals has historically been an academic endeavour and not a high priority for most primary health service providers or managers. This is generally the case in mainstream services and has even more reason to be true in ACCHS where community members who are elected to Boards may place very little value on peer-reviewed publication and be disinterested or dismissive of this form of knowledge, particularly if undertaken by non- Aboriginal researchers.[43] This is reflected in the relatively small number of publications dealing with Aboriginal health, the low frequency of citations of such publications and the paucity of studies that describe or evaluate interventions in Aboriginal health care settings.[44,45] Research projects and publications involving ACCHS have typically involved partnerships with researchers and academic institutions. While the National Health and Medical Research Council (NHMRC) has committed to developing more Aboriginal health researchers and more research in Aboriginal health settings, this has occurred relatively recently, and Australia does not have a long legacy of building research capacity among Aboriginal people or within Aboriginal organisations.[46]
Publication bias may operate in a number of ways. Firstly, journals are generally based upon Western knowledge systems and values, and inevitably value what—in Aboriginal eyes— may be considered an inappropriate epistemology. ACCHS may not support publication of their data, particularly if findings are adverse, and publication favours good news stories. Aboriginal Health Ethics Committees add an additional requirement for approval, research in Aboriginal settings may be more difficult or impractical, and there can be a veto over what gets published or interference in how it is reported, whether it is positive or negative. Local health services research may be of limited interest internationally, an important consideration for editors keen to maximise the relevance of publications to their readers and to increase the impact factor and ranking of their journal. Reviewers and editors of journal papers may reject manuscripts or shape the conclusions and recommendations of articles. Small subject sample sizes (given that Aboriginal people are only 3% of the population) and gatekeeping the involvement of Aboriginal people in research or their reluctance to participate create challenges in producing research that shows a significant difference between groups, services or interventions.
Making Comparisons of Services
Huge variation in the effectiveness of care operates within and across services (both ACCHS and mainstream) and that effectiveness can change over time.[47] Panaretto and colleagues have stated that “currently, there are no well-considered standards for performance or weighting models to enable comparison between services and sectors in Australian primary healthcare” and argued that “supporting a robust comparison of services cannot be done without a consideration of the variety of factors that impact on performance data at the service level”. [48] This undoubtedly contributes to reluctance for researchers to engage in direct comparisons given the difficulties accounting for the impact of a multitude of factors in the service environment, and the potential consequences that ACCHS and mainstream services alike anticipate from critical performance appraisals and comparisons.
Nevertheless, it has been recognised that “sensitive, careful interpretation of the variation in performance at the individual service level and comparison of performance between services over time are essential for both planning health service delivery and action to support improvement at the local, regional and state levels”. [48] The approach by Bailie and colleagues, based on multiple Aboriginal primary care services which are undertaking collection of data by standardised audits for continuous quality improvement purposes, provides some basis for evaluating comparative performance of Aboriginal primary health care services across several jurisdictions in Australia. Arguably, this is the most unbiased means of comparing ACCHS with other services in their standard daily practice, as opposed to evaluation only when a special initiative has been put in place. [49] This research looking at Aboriginal primary health care services noted the variability in quality of data collected at various sites.[50]
Arguing for the importance of developing appropriate measures to help prevent inappropriate comparisons between services that operate in very different contexts, the approach taken in the ACCHS sector in Queensland towards service improvement across the sector, led by their peak body the Queensland Aboriginal and Islander Health Council (QAIHC) offers one way forward.[25] Participating ACCHS in Queensland systematically collect performance data that demonstrate what they do in terms of patient access and delivery on key care activity. As Panaretto and colleagues argue:
“The limited information available suggests that performance in the ACCHS sector on some key care activities is at a higher level than for mainstream general practice providers. It is consistently higher for single clinician care activities such as BP measurement across all services than for team-based activities, where there is much greater variation in the completion of health checks and care plans.” [25]
ACCHS have played a crucial role in demonstrating effective approaches to health care delivery for Aboriginal people, and in advocating for and changing other health services to be more responsive to the needs of Aboriginal people. Their holistic model of care has much to offer Aboriginal patients who have complex care needs indisputably greater than those of other Australians at the same age.
The question of relative effectiveness of different models of primary health care, at first blush a reasonable question, fails to recognise that ACCHS are not treating the same population group or operating in the same places as mainstream primary health services, such that ACCHS operate in much more challenging environments. Any investigation of effectiveness must firstly make explicit (and justify) the range of outcomes addressed by researchers and evaluators compared to those valued by Aboriginal people, and acknowledge the different nature of “evidence” and value placed on it by Aboriginal people. Health and wellbeing are culturally determined concepts and cultural security factors may influence an Aboriginal person’s choice of service provider, even when equivalent ‘health’/biomedical outcomes for Aboriginal clients are potentially achievable by a different provider.[51] This is not to suggest that improvement in biomedical health outcomes is unimportant, but rather to highlight that it is only one component of a broad range of effectiveness measures considered, measured and evaluated to ensure health system objectives are realised.
At the request of the commissioning agent, our review of the evidence was restricted to peer-reviewed literature to meet their time frame and needs. However, a huge amount of additional information of varying quality exists within the grey literature and within reports on key performance indicators to government and other funding agencies. Validation and the assessment of the quality of this information was outside the scope of this review, but undoubtedly such reports contain information which sheds light upon the performance and effectiveness of health services for Aboriginal people. It is likely that those managing funding contracts for ACCHS are aware of which services are performing at a high or low level. Learnings gleaned from peer-reviewed literature on effectiveness cannot replace the need for sensitive and fair contract management to ensure accountability that the dollars being invested by government to deliver health services to Aboriginal people are funding the high quality health care that they need.
Policy making occurs in a complex environment and must take into account the challenges of context. Excellence in health care delivery for Aboriginal people is likely to relate to both the management and clinical capability of the particular service rather than the underpinning governance model, provided that Aboriginal people are involved in and respected at all levels of decision making. In this regard, useful questions are what factors have contributed to the successes or failures of ACCHS and what might be appropriate measures of effectiveness given the different objectives of ACCHS compared to mainstream services. At issue is not whether ACCHS can deliver effective high quality care, but rather what alternatives exist for ensuring that underperforming services improve to meet acceptable levels of health care practice in contemporary Australia. Supporting services to improve care processes and health outcomes based upon understanding and using their own data, and not using data to penalise or single out poorer performing services, acknowledges that services exist somewhere on a continuum and allows services opportunities to improve their effectiveness. Such an approach to improving Aboriginal primary health care can occur at individual health service level or at a sector level and is needed given the complex nature of the problem of improving Aboriginal health. [25,52,53]
Improved and effective health sector access for Aboriginal people can facilitate the appropriate health-seeking behaviours which are critical if the disproportionate burden of morbidity in Aboriginal communities is to be overcome through primary prevention and earlier intervention. Studies demonstrate that when a service is resourced adequately, designed to meet the needs of Aboriginal people and operates out of an ACCHS, Aboriginal people use the service.[54-57] Robust partnerships with mainstream services working together with ACCHS to assist patients across the interface between different services are essential to improving Aboriginal health outcomes. The means for augmenting access to, quality of and partnerships between health care services for Aboriginal people warrant greater attention.[58,59,60]
The authors have no competing interests to disclose
All authors contributed to the review of the literature on effectiveness referred to in the paper and to the development of the paper and the position that it takes. All authors have reviewed and approved the final manuscript.
The literature review was commissioned through the Deeble Institute as a third party. We acknowledge Anne-marie Boxall of the Deeble Institute for her brokering of the funding contract referred to in the paper. Only the authors have had input into the writing of the current manuscript and it does not seek to represent the views of any other parties who were associated with the project that was the catalyst for this paper.