Review Article - (2023) Volume 8, Issue 1
Socioeconomics, Ethnogeriatrics, and Social Determinants of Health: Correlations in Hypertension Patients
Jared M Williams* and
Diana Garza
Department of Food Sciences, University of the Incarnate World, San Antonio, United States
*Correspondence:
Jared M Williams,
Department of Food Sciences, University of the Incarnate World, San Antonio,
United States,
Email:
Received: 23-Dec-2021, Manuscript No. IPJHCC-21-12149;
Editor assigned: 03-Jan-2022, Pre QC No. IPJHCC-21-12149 (PQ);
Reviewed: 10-Jan-2022, QC No. IPJHCC-21-12149;
Revised: 23-Jan-2023, Manuscript No. IPJHCC-21-12149 (R);
Published:
30-Jan-2023, DOI: 10.36846/2472-1654-8.1.8003
Abstract
This study explores the impact of Social Determinants of Health (SDOH): diet/nutrition, food insecurity, physical activity, ethno geriatrics, and socio economic factors on hypertension patients living in underserved, low income, and urban communities. Baseline data from January to May 31, 2021, was compared to post data in June and July 2021. This two fold research attempted to predict what cultural factors lead to compliance in achieving lower blood pressure levels. Investigations of the statistical differences between variables were used in a multivariate analysis and were compared amongst pre and post data. Research questions and hypothesis testing that guided this study included. Hypothesis testing for the research questions was completed to determine if we should reject or fail to reject the null hypothesis. Post data showed that there was a statistical significance in the patients’ race, ethnicity, age, FPL (Federal Poverty Level) status, food insecurities, and nutrition counseling. Additionally, the post data proved that blood pressure levels decreased tremendously from 169/90 to 130/80 after the implementation of SMBP devices. Limitations and additional research are discussed as well as considerations for future researchers when performing this research in the selected communities.
Keywords
Ethno geriatrics; Social determinants; Hypertension patients; Hypothesis testing; Urban
communities
INTRODUCTION
Hypertension (HTN) amongst racial and ethnic communities
has remained a persistent health concern worldwide,
especially in the United States. In the United States alone, it is
estimated that there are nearly 116 million people living with
a diagnosis of controlled or uncontrolled hypertension.
Amongst those living with this disease, Blacks have exhibited
a higher prevalence when compared with other races and
ethnic groups. Hypertension or blood pressure is the measure
of the force of blood pushing against the blood vessel walls
(WebMD, 2019). Hypertension (HTN) is known as “the silent
killer,” and affects millions of people in multiple age ranges
and ethnicities. This disease can be caused by several factors
such as smoking, lack of physical activity, being overweight,
excess salt consumption, and genetics. According to the
centers for disease control and prevention, high blood
pressure affects one in three adult Americans, but people do
not even know they have HTN with the aforementioned
factors that impact hypertension, there are other important
variables such as socio-economic status, ethno geriatrics,
social determinants of health, and compliance that play
bigger roles in the care of patients. Additionally, there is
another factor that has impacted the low-income and
underserved patients suffering with hypertension. The recent
outbreak of the novel Coronavirus (COVID-19) has swept
across the world and most heavily in the United States. As the
world passed the one-year mark for COVID-19, healthcare
professionals, especially those in low-income, under-served,
ethnic, and rural communities have seen great declines in
health outcomes within the populations they serve. Reported
data from 1,099 patients who were confirmed positive for
COVID-19; for 15% of this group, the single highest risk factor
of infection was hypertension. The relationship between
COVID-19 and hypertension remains unknown, but there are
preliminary data points that HTN is a prevalent comorbidity
among patients admitted with COVID-19. With few studies
conducted in HTN, COVID-19 and health disparities, the full
impact of the pandemic is unknown with only limited data
being released [1-5].
Statement of Problem
It is unknown to what extent COVID-19 has impacted patients
diagnosed with HTN living in low income, vulnerable, and
underserved communities. Hypertension (HTN) remains the
leading cause of premature death in the United States
(national center for health statistics, 2017). Risk factors such
as prediabetes and obesity increase the risk of HTN in all age
groups. Recent data has revealed that the use of
antihypertensive medication among patients with an HTN
diagnosis was only 62% effective. What is also unknown is to
what extent or level of rigor do patients follows a medication
regimen at home. Although we live in the age of technology,
Ostchega estimate that only 25% of U.S. adults with hypertension engage in some form of home blood pressure
monitoring. In April 2020, many insurance companies began
expanding coverage and defining reimbursement for
telemedicine services. In the U.S., at least 15% of physicians
work in practices that use telemedicine and adoption by
private insurers has increased by 50%. The approval of such
services became priority when Managed Care Organizations
(MCOs) began seeing an increase in patients who were not
receiving the recommended check ups and instead were using
emergency rooms and urgent care facilities for basic needs.
Funding for essential programs was launched so patients with
chronic care conditions could monitor their health from the
safety of their home. Some of the solutions to chronic care
conditions were the use of electronic processes and
communication technologies referred to as e-health; and mhealth
which is the use of telemedicine and mobile health.
The focus of the additional funding has been for the group of
patients who are unable to make regular doctor
appointments. In many cases, this group comes from a
socially complex and economically disadvantaged population
that faces cost, poor health literacy, and other social
determinant barriers. Improving hypertension control was the
focus for the population in this study. Specifically, to minimize
the number of individuals who could not achieve blood
pressure control, Self-Measured Blood Pressure Monitoring
(SMBP) was developed so that patients could evaluate their
measurement outside the clinic with additional support in an
effective manner. Many factors impact how this demographic
of patients will achieve holistic health while trying to coexist
in society. With a weakened economy that has extended
beyond health to encompass household incomes, individual
livelihoods, and nutritional intake, disadvantaged patients are
still projected to increase the cost on the healthcare system.
This cascading effect impacts the patient’s ability to afford
medications, attend medical appointments, or eat a healthy
diet to keep blood pressure levels below 140/90 which is
considered an optimal level. Qualifications to participate in
this study included non-compliant nutritional and medication
patients, patients who required SMBP devices due to missed
appointments, and at least three consecutive readings above
140/90. This research will contribute to clinical practice by
giving health care providers data on patient compliance based
on their culture to adhere to small scaled lifestyle changes
such as home based self-blood pressure monitoring and
following a nutritional, patient educational, and medication
regime [6-10].
Purpose Statement
The purpose of this quantitative research study is twofold;
first to evaluate whether the following social determinants of
health: diet/nutrition (food insecurity), physical activity, ethno
geriatrics, and socio economic factors impact hypertensive
diagnosed patients living in underserved and vulnerable
urban communities. Second, this study will also attempt to predict what cultural factors lead to compliance in achieving
lower blood pressure levels. Compliance meaning patient
medication after study enrollment. Adherence and selfmonitoring
of HTN. Changes were measured from baseline to
2 months
Definition of Terms
For a better understanding of this study, the following terms
are operationally defined.
Hypertension and Uncontrolled Hypertension.
The current definition of Hypertension (HTN) is Systolic Blood
Pressure (SBP) values of 130 mmHg or more and/or
Diastolic Blood Pressure (DBP) more than 80 mmHg.
Uncontrolled hypertension is defined as an average systolic
blood pressure of 130 mmHg or an average diastolic blood
pressure of greater than 80 mmHg amongst those with
hypertension.
Self-Measured Blood Pressure
This refers to Self-Measured Blood Pressure (SMBP)
monitoring by the patient outside the clinical setting, either at
home or elsewhere.
Social Determinant of Health
Social determinants of health or SDOH refers to the
conditions in the environments in which people are born, live,
learn, work, play, and worship, and affect a wide range of
health, functioning, and quality of life outcomes and risks.
Ethno Geriatrics
This term refers to components of geriatric care that
considers the influence of ethnicity and culture on the health
and well being of older adults.
Patient Compliance
This refers to the process whereby the patient follows the
prescribed and dispensed regimen as intended by the
prescriber and dispenser.
Food Insecurity
Food insecurity is defined as the disruption of food intake or
eating patterns because of a lack of money and other
resources.
Literature Review
A literature review was conducted to provide a foundation of
knowledge on the causes of hypertension linked to food
insecurity, health factors, ethno geriatrics, and culture based
compliance and social determinants of health.
Food Insecurity and Hypertension
Food insecurity is defined as limited or inadequate access to
food, often related to individual factors such as poverty, disability, and systematic factors like transportation or grocery
store access. There is a complex relationship between Social
Determinants of Health (SDOH), food insecurities, and health
disparities which needs to be understood. The premise of
healthcare has always been looked upon as being within a
clinical setting, whereas societal wellbeing is contingent upon
health being a factor outside of the clinical walls. There is a
lack of current research focusing on elements such as SDOH,
COVID-19, and chronic care conditions such as hypertension
used a population based sample to evaluate associations
between food insecurities and risk factors including
hypertension, hyperlipidemia, and diabetes. Using laboratory
data to confirm results, the researchers were able to quantify
the prevalence for each condition. The study was conducted
from 1999-2004 on 31,126 individuals that were over the age
of 18 but less than 65 years old. The study found that Latino
households were more likely to be food insecure than White
households. Additional analysis found that low educational
attainment, low household income, lack of health insurance,
and tobacco use was associated with these individuals. This
study provided evidence and linkage to household incomes of
below 200% of the Federal Poverty Level (FPL) contributing to
the clinical evidence of hypertension found that as the
likelihood of food insecurity increased, health disparities also
increased. Ultimately, the health outcomes were linked to
inadequate access to fresh fruits and vegetables (food
insecurity). Individuals in these areas could either not afford
to purchase necessary food for the desired lifestyle change, or
there was not a location nearby or accessibility to local
neighborhoods or communities [11-14].
Health Factors, SDOH, and Hypertension
In the United States, nearly 50% of adults are living with
hypertension. Research on the SDoH factors and the impact
on HTN levels are still not well understood. Despite various
efforts to understand and improve the unique and complex
health behaviors, researchers have chosen to examine
individual provider and patient characteristics. One
characteristic that is not fully explainable is medication
adherence. Hensley, et al. found that social support, food
insecurity, poverty, and lack of transportation are associated
with hypertension and medication adherence in patients. A
study by Donneyong, et al. uncovered four major categories
relating to health factors, SDoH, and HTN. The factors
included poverty, weak social support, healthy built
environment, and food insecurity. Each of the factors within
this study had sub topics that were used for measuring factors
of social determinants of health. Factors of measurement
included percent below the poverty line, uninsured
percentage, residential segregation, severe housing problems,
food insecurities, limited access to healthy foods, and food
environment index. The study findings highlighted the
following factors as having an impact on HTN and medication
adherence: poverty/food insecurity, weak social support,
unhealthy built environments, and African American females
who live in rural counties. This study reinforces the theory
that SDoH play a critical role in an individual’s ability to
achieve compliant or non-compliant HTN levels. Individuals without the resources were found to be less complaint in
adhering to medical instructions involving antihypertensive
medication. It is important to learn more about the patients
and tailor an approach that fits each individual need. While
tailoring an approach may seem cumbersome, it is necessary
when looking to achieve total health. A Study by Dawson,
Walker, Gregory, and Egede studied the relationship between
Social Determinants of Health (SDoH) and systolic blood
pressure in United States immigrants. SDoH includes factors
such as where people are born, live, work, and age that
contribute to several health inequities and preventable
disparities, many of which can be prevented. Such lifestyles
affect a person’s risk for developing chronic diseases such as
hypertension. Due to limited research in the area of SDoH and
its link to poor health outcomes, the study used a theory
based model that incorporated SDoH and specific factors to
examine the relationship between antecedent factors (region/
country of origin, ethnicity/race, life course socioeconomic
status), predisposing factors (i.e. age, sex, marital status,
education, employment, household income, subjective social
status, homelessness, and immigrant stress), enabling factors
(i.e. healthcare access, insurance status, perceived
discrimination, perceived stress, health literacy, self-efficacy,
acculturation), and need factors, and blood pressure control
in a diverse population of immigrants in the Midwestern
United States. The study found that socioeconomic status,
age, sex, and being homeless to be associated with increased
systolic blood pressure. This study is consistent with prior
literature by Howell. Where age and male sex were found to
be positively associated with higher levels of HTN [15-17].
Ethno geriatrics
Ethno geriatrics refers to the influence of culture, race, and
ethnicity on health care for older people from diverse ethno
racial populations. Taking this into consideration, medical
providers need to have cultural competence when addressing
health disparities within the community health setting. It has
been shown that multi-cultural patients experience higher
comorbidities, shorter life expectancies, and disabilities than
non-hspanic Whites performed a study examining the
differences in self-care behaviors for hypertension, the results
showed African American women were more likely to
consume recommended amounts of fruits and vegetables but
less likely to engage in physical activity to manage
hypertension than white women. Furthermore, African
American elders are more likely to incorporate nontraditional
self-care strategies such as home remedies for chronic illness
management than White elders. Three out of four adults
older than the age of 65 have three or more chronic
conditions such as Diabetes (DM), obesity, cardiovascular
disease, congestive heart failure, renal insufficiency, and not
the least of which is hypertension sought to address the
complexities of hypertension in individuals who are older and
have several additional considerations. Their study focused on
blood pressure target levels and comorbidities. The study
reviewed the epidemiology of the aging process and found
that normal HTN in men and women will increase by 85% at
the age of 55, or the patient will develop hypertension over the next 20 to 25 years. This prevalence amongst older
Americans is due to factors that are generally not considered.
The main consideration was vascular changes in patients. The
structural changes as a person ages contributed to the arterial
pulse wave velocity. This is interesting as this suggests an
answer to the issue of hypertension development within this
unknown phenomenon. The ethno geriatric implications of
hypertension have heightened with COVID-19. The
disproportionate impact of COVID-19 exposed some of the
manifold disparities with social determinants of health.
Higher rates of preexisting conditions such as diabetes,
hypertension, and other chronic medical conditions amongst
the geriatric population are often ignored if the patient is
uninsured and within the group of population that is
vulnerable and underserved.
African American Culture
When examining the cultural dynamic of ethno geriatrics, age
and culture impact HTN levels. There has been insufficient
evidence to support those lifestyle modifications,
socioeconomic factors, and genetic factors correlate to
developing or living with HTN. The two populations with the
highest prevalence of HTN are Hispanic and African American.
A study by Peters examined Hispanic and African American
cultures to determine correlations between the Theory of
Planned Behavior (TPB) and patient compliance. The
researchers concluded that the attitude, subjective norms,
and perceived behavioral control of these groups played a
major part in the future patterns and habits of the individuals.
Perceived behavioral control will ultimately predict actual
health behaviors. The examination of culture and medication
compliance must be segmented, as different cultures have
different attitudes, normative beliefs, and control beliefs
formed focus groups and collected data based on the TPB
model. Results of the analysis found that African Americans
possess a “circle of culture” mind set. This mind set
symbolizes what is acceptable and provides boundaries based
on heritage and culture as well as separates insiders from
outsiders. Beliefs regarding strategies to prevent and or
reduce HTN resulted in self-care measures. When focusing on
the main reasons for medication adherence, participants
expressed that there was a lack of trust in physicians and
reluctance to seek medical care. This generational distrust of
the health care system can be linked to the Tuskegee
experiment, where black men were denied treatment for
syphilis so doctors could study the disease’s progression. This
distrust was also linked to HTN control claiming that patients
are getting conflicting HTN readings and suspicious motives
for prescribing antihypertensive medications. Similar to
research the relationship between adherence to diet and
physical activity using socio cognitive approaches (self-efficacy
and social support). These study findings addressed the
dietary culture that inhibited decreased adherence for diet
and physical activity. This portion of adherence is related to
social support. As African Americans are less likely to receive
medical care due to mistrust and racial bias amongst
physicians, many individuals find themselves seeking support
from family members, friends, and associates to reach goals.
This is culturally unacceptable due to various factors, such as
misguided health recommendations.
Hispanic Culture
The hispanic population in the United States is comprised of
various genetic backgrounds and distinct cultures. This
population has consistently shown a lower prevalence of HTN
compared to non-hispanic whites and blacks. A study by the
National Health and Nutrition Examination Survey (NHANES)
examined data on this population that was comprised of HTN
data: Age, sex, race/ethnicity (Mexican American, white,
black), and BMI. Compared to blacks and whites, Hispanic
subjects were not receiving treatment for hypertension. While
examining BMI and age, it was noticed that the prevalence
increased with Hispanic women and men who were from
Puerto Rico and the Dominican Republic; this population was
2.6 times more likely to have hypertension. Researchers found
that because this disease is asymptomatic, it goes
undetected. When detected and treated, Mexican Americans
had significantly lower HTN control rates than whites and
blacks. Although the rates were lower, the decreases
suggested that that the advances in antihypertensive
medication are not meaningful. Understanding the distinct
culture in this study meant understanding that most subjects
did not have a primary care physician and used the
emergency room as their primary source of care. Machismo
image amongst men was heavily sought to be projected, while
any signs of illness was culturally unacceptable. Finally, it was
seen as being fatalism (e.g., “It is god’s will”) within this
cultural community as a large contributor to not seeing a
physician for health related factors, especially hypertension.
Ultimately, culture plays a huge role when examining
medication adherence and assessing the impact of medical
care. The medical distrust and beliefs patients display speaks
volumes and translates to a person’s health status and
wellbeing.
Social Determinants of Health and Hypertension
Social determinants of health are conditions in places where
people live, learn, work, and play that affect a wide range of
health risks and outcomes. There are five main areas as
defined by healthy people 2030:
• Healthcare access and quality: the connection
between people’s access to and understanding of
health services and their own health. This area also
includes health insurance coverage and health literacy.
• Education access and quality: the connection of
education to health and wellbeing. Included within
this topic is graduating from high school, higher
education enrollment, educational attainment, language
and literacy, and early childhood development.
• Social and community context: This context is two-fold.
Positive relationships help reduce negative impacts. These
include relationships and interactions with family, friends,
co-workers, and the community. Negative relationships
include not being able to control factors such as discrimination, unsafe neighborhoods, incarceration,
and/or being unable to afford the basic needs.
• Economic stability: The connection between
financial resources people may have. This includes
income, cost of living, and socioeconomic status-and
their health. Key areas are also highlighted such as
poverty, employment, food security, and housing stability.
• Neighborhood and built environment: The
connection between where a person lives and their
wellbeing. Topics include quality of housing, access
to transportation, availability of healthy foods, air and
water quality, and neighborhood crime and violence.
These conditions are typically observed from a community
centered aspect. This model is often referred to as the
community centered health home or CCHH model. Using the
CCHH model, the patient is screened at the clinic for social
determinants of health factors that can impact health outside
of the clinical walls. The defining attribute of the CCHH is
translating high priority medical conditions into active
involvement in community advocacy and change. Using the
Protocol for Responding to and Assessing Patients Assets,
Risks and Experiences (PRAPARE) tool, data elements are
collected such as employment, food insecurity, housing, utility
needs, substance abuse, transportation, education, and
physical activity to help meet the patient’s population needs.
The issue with this model and study is that it is not deployed
into all communities that need it. With the unavailability of
this model, there is an oversight of need; this is an element
that is often overlooked within studies concerning SDOH.
Therefore, while this approach is appropriate, it will not be a
complete study unless all elements are fulfilled for patient
total wellbeing. When examining issues with hypertension as
it relates to SDOH, the state of Texas puts patients in a unique
situation. The medicaid eligibility expansion of the Affordable
Care Act (ACA) was ruled not to be required by the US
Supreme Court. This ruling impacted millions of low income
patients from being able to access affordable and timely care.
Angier, Hogue, Marino, Green, Holderness examines the
impact of this ruling and how it affects healthcare access and
services for patients at risk, diagnosed, and undiagnosed with
hypertension. This study also examines these factors as it
relates to social determinants of health at both the individual
and community level which also influences diagnosis and
care. This study had four aims as it compared prevalence,
hypertension incidence, screening, treatment, and
management. The researchers used a similar dataset to this
study from community health centers. The study’s period
range was from January 1, 2012, to December 31, 2016. This
span of study allowed for understanding from a short,
medium, and long term impact of the ACA. Social
determinants of health metrics within the study included built
in environment, race/ethic composition, neighborhood
resources, neighborhood socioeconomic composition, and
social deprivation index (poor access to healthcare and poor
health outcomes than a measure of poverty). While this study
was able to pull in the largest dataset relevant to this project,
the study had several limitations that prevented confidence in
the data. This study was unable to identify patients who died during the study’s time period as well as missing data from
services documented in inaccessible parts of the electronic
medical record. A major limitation included data not collected
from other providers that patients may have visited such as
emergency rooms or other healthcare providers. This
limitation is common for researchers as most areas have not
developed a health information exchange mechanism
amongst all healthcare providers. After reducing errors in the
data, this study can be used to tailor treatment plans and
healthcare access for low income and vulnerable populations.
Methodology
A two group, pre and post intervention design was selected to
assess the success of SMBP (self-measured blood pressure)
devices with interventions such as compliance (medication/
appointment), diet/nutrition and exercise, socio economic
factors, and SDOH (cohort 1). Cohort 2 included patients who
were not participating in the SMBP device program. Pre
intervention data was collected beginning January 1, 2021,
and ending May 31, 2021. Post intervention data began June
1, 2021, and was collected weekly. The project is on going and
expected to be completed when patients have achieved
consistent compliance with blood pressure readings.
Design
The aim of this study was to find relationships between
hypertension, socioeconomic factors, social determinants of
health, and ethno geriatrics. This study will use a pre and post
design to measure the outcomes of interest prior to
administering the SMBP device and addressing SDOH and
ethno geriatrics. Variables in the study include blood pressure
levels, socioeconomic factors, social determinants of health,
and ethno geriatrics. Each variable, except for ethno
geriatrics, has additional categorizations that are associated
for further identification. Those are:
• Blood pressure levels
• Compliant: Less than 140/90.
• Non-Compliant: Greater than or equal to 140/90.
• Socioeconomic Factors:
• Federal Poverty Levels (FPL): Determined by
salary, number of members in the household,
and the department of health and human services FPL
scale.
• Social Determinants of Health (SDOH)
• Food insecurities
• Diet and exercise
Participants
The data set included existing patients of the clinic. Patients
were asked if they were willing to participate in the study of
the use of SMBP devices at their medical appointment or
through clinical outreach via phone call or push message.
Informed consents and appointments were scheduled for
patients who confirmed interest in participating in the
program. During the medical appointment, the medical staff educated each patient on how to use the device, who to call if
there was an error, how to pair the device with their phone,
and the interventions that are recommended while in this
program. Participation in this study required that clinic
patients be 18 years or older and have a diagnosis of HTN.
Demographics for the eligible 3,200 patients include 60%
hispanic, 30% African American or black, 5% white, and 5%
other (Asian, more than one race, native American, or Pacific
Islander). While there are only 3,200 patients, there is a
potential of an additional 2,000 patients who are almost in
pre hypertension stage.
Research Questions/Hypothesis
The following research questions/hypothesis will guide this
study.
• R1: Is there a relationship between socioeconomic factors
and hypertension levels in patients?
• H₀: Socio-economic factors do not have a statistically
significant effect on HTN.
• Ha: Socio-economic factors have a statistically significant
effect on HTN.
• R2: Is there a relationship between SDOH factors and HTN
levels in patients?
• H₀: SDOH factors do not have a statistically significant
effect on HTN.
• Ha: SDOH factors have a statistically significant effect on
HTN.
• R3: Is there a relationship between cultural backgrounds
and HTN levels in patients?
• H₀: Cultur al backgrounds do not hav e a statistically
significant effect on HTN.
• Ha: Cultural backgrounds have a statistically significant
effect on HTN.
• R4: Is there a relationship between patient compliance
and HTN level in patients?
• H₀: Patient compliance does not have a statistically significant effect on HTN.
• Ha: Patient compliance has a statistically significant effect
on HTN.
Data Collection
Access health community health center, Inc. is based in
Richmond, Texas with 5 satellite locations in Brookshire,
Stafford, Sugar Land, Missouri City, and East Missouri City
(EFB). Each of these locations, except for Stafford, treats adult
patients. Each year access health reports clinical quality
measures to the Health Resource and Service Administration
(HRSA) within the Uniform Data Systems Report (UDS). Within
this reporting, there is a focus on hypertension and
compliance rating. For a patient to be counted in this
measure, patients must be age 18 or older, with the diagnosis
of hypertension (including essential hypertension) and have a
medical visit during the measurement period. Data is
recorded and reported through the nurse triage process and
the Electronic Medical Record (EMR) or through transmission
from the SMBP device to the patient portal, then to the EMR.
From this point, data can be extracted with reporting tools
that will enable additional fields of data collection to be
analyzed. Examples of additional fields are appointment
information (no shows, kept appointments, and
cancellations), additional services used such as dental and
behavioral health, and if the patient was referred to an
outside entity for additional services. The Health Resources
and Services Administration (HRSA) generally want the data
grouped by race and ethnicity so that trends and action items
can be targeted. Blood pressures are taken to determine if the
diastolic and systolic are below or above 140/90. Whether in
the clinic or the home, it is encouraged to retake the blood
pressure after an abnormal reading. The goal is to ensure that
the patient has a lower blood pressure reading at the visit
closest to the end of the measurement year. This gives the
clinicians time to work with the patient to get readings under
control. It is also important to note that quality assurance is
audited and discussed monthly at Quality Improvement
meetings with medical staff. Plan Do Study Act (PDSA) model
is continuously used to look for areas of improvement.
Sociodemographic Variables
Sociodemographic data is collected and are made available
monthly for executive leadership and quality improvement/
performance improvement committee members. This study
included the following Sociodemographic variables: Age,
income level, education, race and ethnicity, city of origin, and
zip codes, and SDOH survey results. Blood pressure readings,
socio economic factors, SDOH, ethno geriatrics, and medical
appointment compliance/patient compliance were used as
dependent variables for this study.
Data Analysis
A multivariate analysis was used to determine how each of
the factors impact blood pressure readings. The four
categories for research include:
• Socio-Economic Status
• Insurance Status/type
• Percentage under the Federal Poverty Level
• Social Determinants of Health (SDOH)
• Food Insecurity
• City of origin
• Cultural Background
• Age
• Race
• Ethnicity
• Gender
• Patient Compliance
• Nutrition
There have been previous studies conducted on samples of
500 patients or less but are not focused on one geographical
location limiting what can be done to mitigate high HTN levels
in underserved and vulnerable communities. This study
addresses each of the factors that were previously addressed
as well as adds to previous literature. Lastly, this study
observes blood pressure readings from inside the clinical
setting (pre data) and in the patient’s setting of the home
(post data).
The data was analyzed using STATA with controlled variables.
An initial overview of the data in the multivariate model was
examined. Additional analysis was used to determine if the
data had multicollinearity and heteroskedasticity.
Preliminary Analysis
The following tests were conducted to determine
multicollinearity:
• Examining VIFs (Variance Inflation Factors) to determine if
the VIF exceeded four, which warrants further
investigation. VIFs greater than 10 will require correction.
• Regression analysis (pre and post data) to determine
statistical significance.
Using these steps as well as examining the multivariate
regression, it was determined that VIF values were less than
four, which indicated that there is not
multicollinearity present in the data (Table 1).
| Variable |
VIF |
1/VIF |
| Ethnicity |
3.76 |
0.266 |
| Race |
3.84 |
0.26 |
| Sex |
1.06 |
0.94 |
| Age |
1.19 |
0.838 |
| FPL |
1.13 |
0.886 |
| Food Insecurity |
1.07 |
0.935 |
| Nutrition |
1.09 |
0.92 |
| Insurance |
1.08 |
0.929 |
| BMI Ratio |
1.09 |
0.915 |
| City |
1.05 |
0.95 |
Table 1: Variance Inflation Table (VIF).
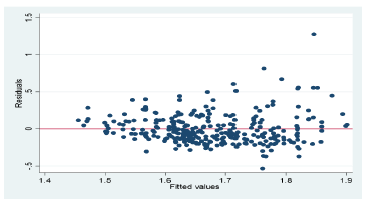
Heteroscedasticity
Additional analysis was conducted to test for
heteroscedasticity. If heteroscedasticity was present in the
data, the model violates the assumption, thus unreliable and
bias data will be present. The initial investigation of the data
will be performed by running a fitted residuals graph on
residuals. Because the residuals were roughly the same size
for all values of X, it was concluded that heteroskedasticity is
not severe enough to warrant concern (Figure 1). For each of
the research questions, the null hypothesis assumes no
statistical significance or correlation on hypertension levels.
For additional analysis in this model, p-values, f-statistic value,
t-value, and r-square values were also observed. This analysis
was conducted with a 95% confidence interval and alpha level
of 0.05.
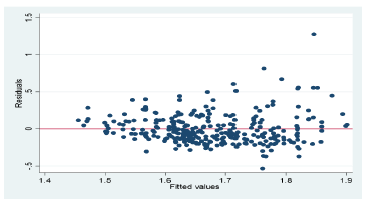
Figure 1: Heteroscedasticity testing.
Note: Initial test on a scatter plot to determine
heteroskedasticity.
Results
Prior to testing the hypothesis, baseline data was analyzed to
gain an understanding of the results and consistency
amongst the populations. This analysis found that the factors
of ethnicity, race, age, and insurance status had a
statistical significance to blood pressure readings. Overall
summary statistics for the pre cohort showed that there were
1,221 participants with a mean blood pressure of 1.865 or
169/90. Participants who identified as hispanic and white as
well as not hispanic and black or African American were
found to have the highest prevalence of high blood pressure
within the cohort (Table 2). Table 3 shows the
participant’s demographic breakdown.
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| Ethnicity |
3.41 |
0.001 |
0.047 |
0.173 |
| Race |
5.94 |
0 |
0.041 |
0.082 |
| Sex |
-0.91 |
0.363 |
-0.081 |
0.029 |
| Age |
13.33 |
0 |
0.013 |
0.018 |
| FPL |
1.04 |
0.297 |
-0.007 |
0.022 |
| Food Insecurity |
0.8 |
0.426 |
-0.02 |
0.047 |
| Nutrition |
0.75 |
0.454 |
-0.093 |
0.207 |
| Insurance |
3.48 |
0.001 |
0.016 |
0.058 |
| BMI Ratio |
0.95 |
0.342 |
-0.002 |
0.006 |
| City |
4.42 |
0 |
0.002 |
0.005 |
Note: Number of studies=1,221, R-square=.9408. CI=Confidence Interval; LL=Lower Limit; UL= Upper Limit
Table 2: T-Values and P-Values relating to blood pressure.
| Baseline characteristic |
Full sample |
| n |
% |
| Gender |
| Male |
484 |
40% |
| Female |
737 |
60% |
| Age |
| Group 0 (18-30) |
8 |
1% |
| Group 1 (31-45) |
160 |
13% |
| Group 2 (46-64) |
670 |
55% |
| Group 3 (65+) |
383 |
31% |
| Ethnicity |
| Hispanic |
577 |
47% |
| Not Hhispanic |
642 |
53% |
| Other |
2 |
0% |
| Race |
| American Indian |
5 |
0% |
| Asian |
143 |
12% |
| Black or AA |
391 |
32% |
| Declined |
6 |
0% |
| Native Hawaiian |
2 |
0% |
| White |
674 |
55% |
Note: N=1,221. Participants were on average 59 years old. Average blood pressure=160/90
Table 3: Demographic distribution of patients cohort 1.
Post data analysis was used to test the research questions as
well as similarities in disparities for post data participants.
Overall summary statistics for post cohort data shows 298
participants who opted into the program with a mean blood
pressure of 1.67 or 130/80. Leading these participants were
patients w ho identified as his panic (white) and non-hispanic
black or African American and Asian (Table 4).
| Baseline characteristic |
Full sample |
| n |
% |
| Gender |
| Male |
99 |
33% |
| Female |
199 |
67% |
| Age |
| Group 0 (18-30) |
7 |
1% |
| Group 1 (31-45) |
64 |
21% |
| Group 2 (46-64) |
188 |
63% |
| Group 3 (65+) |
39 |
13% |
| Ethnicity |
| Hispanic |
185 |
62% |
| Not Hispanic |
11 |
4% |
| Other |
2 |
1% |
| Race |
| American Indian |
3 |
1% |
| Asian |
36 |
12% |
| Black or AA |
64 |
21% |
| Declined |
2 |
1% |
| Native Hawaiian |
1 |
0% |
| White |
192 |
64% |
Note: N=298. Participants were on average 57.98 years old, average blood pressure 130/80
Table 4: Demographic distribution of patient’s cohort 2.
Findings for Research Question One
• R1: Is there a relationship between socio-economic factors
and HTN levels in patients?
• R1: Is there a relationship between socio-economic factors
and HTN levels in patients?
• Ha: Socio economic factors have a statistically significant
effect on HTN.
As shown in Tables 5 and 6, a multivariate analysis was
employed to examine the relationship between patient’s
socio economic factors (insurance status/type and FPL) and HTN levels. No statistical significance was found for patients
who had CHIP, commercial, medicare, and Texas marketplace.
A statistical significance was found for patients who had
Medicaid at p=.03. Additional analysis for patients who were
100% or below the FPL showed a statistically significant effect
on HTN levels at p=.0047. With all combining factors, the null
hypothesis was rejected as FPL .047<0.05. For the variable off
insurance, we fail to reject the null hypothesis as
Insurance Status/type=.665>0.05.
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| FPL |
2 |
0.047 |
0.003 |
0.051 |
| Insurance |
0.43 |
0.665 |
-0.019 |
0.03 |
Note: Number of studies=298, R-square=.9838. CI=Confidence Interval; LL= Lower Limit; UL= Upper Limit; FPL=Federal Poverty Level; Number of studies=298; R-square=.9838.
Table 5: T-values and P-values relating to blood pressure and socioeconomic factors.
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| FPL |
| 100% or below |
4.41 |
0 |
0.62 |
1.63 |
| 101-150% |
5.28 |
0 |
0.86 |
1.89 |
| Over 200% |
2.92 |
0.004 |
0.34 |
1.75 |
| Unknown |
4.81 |
0 |
0.71 |
1.7 |
| Insurance |
| CHIP |
-0.29 |
0.769 |
-0.49 |
0.36 |
| Commercial |
1.3 |
0.194 |
-0.04 |
0.2 |
| Medicaid |
2.14 |
0.033 |
0.01 |
0.25 |
| Medicare |
-0.2 |
0.841 |
-0.15 |
0.12 |
| Self-Pay |
1.19 |
0.235 |
-0.03 |
0.13 |
Note: Number of studies=298; R-square=.9838; CI=Confidence Interval; LL=Lower Limit; UL= Upper Limit; FPL=Federal poverty level
Table 6: Detailed look at FPL and insurance status.
Findings for Research Question Two
• R2: Is there a relationship between SDOH factors and HTN
levels in patients?
• H₀: SDOH factors do not have a statistically signif icant
effect on HTN.
• Ha: SDOH factors have a statistically significant effect on
HTN.
As shown in Table 7 a multivariate analysis was employed to
examine the relationship between SDOH factors of food
insecurity and city of origin, and HTN levels. With HTN ratios
increasing by one point, food insecurity negativity rates
decreased by 042. Speci ically, patient’s readings post
intervention proved to be statistically signi icant. Patients who
resided in speci ic cities such as Beasley Hempstead,
Needville, and Rosenberg, Texas showed high correlations
with SDOH factors with the highest factor being food
insecurity identi ication. With all combining factors we reject
the null hypothesis of SDoH which was furthered categorized
into city of origin and food insecurity. Statistical signi icance
was found at p=.009 for city of origin and p=.04 for food
insecurity.
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| City of origin |
2.63 |
0.009 |
0.001 |
0.007 |
| Food insecurity |
-1.97 |
0.049 |
-0.084 |
0 |
| Note. Number of studies=298; R-square=.9838; CI=Confidence Interval; LL=Lower Limit; UL= upper limit. Each city and food insecurity status that was report was below p <.05, which proved significance. |
Table 7: City of origin and food insecurity status.
Findings for Research Question Three
• R3: Is there a relationship between cultural background
and HTN levels in patients?
• H₀: Cultural background does not have a statis tically
significant effect on HTN.
• Ha: Cultural background factors have a statistically
significant effect on HTN.
A multivariate analysis was employed to examine the
relationship between patients with diverse cultural
backgrounds (race, ethnicity, age, and gender), and HTN
levels. Patients who identified as white, black, or African
American, Asian, American Indian, and other all showed a
statistically signi icant p value of 0.00. Age of the patients
showed signi icance amongst all age groups with a collective
statistically signi icance of p=0.00. Gender did not show a
statistically signi icant effect on HTN levels (Table 8).
Therefore, the research question of cultural background
in luencing HTN levels found correlations for patients based
on age and ethnicity. With all combining factors we fail to
reject the null hypothesis based on gender (p=.440), and
reject the null hypothesis related to race (p=0.00), ethnicity
(p=0.001), and age (p=0.00).
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| Ethnicity |
3.41 |
0.001 |
0.05 |
0.207 |
| Race |
3.87 |
0 |
0.022 |
0.07 |
| Sex |
0.77 |
0.44 |
-0.033 |
0.075 |
| Age |
7.32 |
0 |
0.115 |
0.201 |
Note: Number of studies=298; R-square=.9408; CI=Confidence Interval; LL=Lower Limit; UL= Upper Limit
Table 8: T-Values and P-Values relating to blood pressure and ethno geriatrics.
Findings for Research Question Four
• R4: Is there a relationship between patient compliance
and HTN level in patients?
• H₀: Patient compliance does not have a stat istically
significant effect on HTN.
• Ha: Patient compliance has a statistically significant effect
on HTN.
As shown in Table 9, a multivariate analysis was employed to
examine the relationship between patient compliance and
HTN levels. Patient compliance with nutrition counseling
showed a statistically significant impact on HTN levels.
Patients who did attend nutrition classes showed a statistically
significant effect with a p value = 0.00. Patients who did not
attend nutrition counseling were shown to be non-compliant
in their BMI status. Therefore, patient compliance was
a significant predictor of optimal HTN levels. With all
combining factors we must reject the null hypothesis relating
to nutrition counseling (p=0.00) and fail to reject the null
hypothesis relating to BMI (p= .051).
| Variable |
T-Value |
P-Value |
95% CI |
| LL |
UL |
| Nutrition |
3.87 |
0 |
0.253 |
0.777 |
| BMI |
-1.63 |
0.103 |
-0.002 |
0 |
Note: Number of studies=298; R-square=.9408; CI=Confidence Interval; LL=Lower Limit; UL= Upper Limit
Table 9: T-Values and P-Values relating to blood pressure and patient compliance.
Discussion
This study was conducted with the purpose of evaluating the
impact of whether the following social determinants of
health: diet/nutrition (food insecurity), ethno geriatrics, and
socio economic factors impact hypertensive diagnosed
patients living in underserved, vulnerable, and urban
communities. Second, this study attempted to predict what
cultural factors lead to compliance in achieving lower blood
pressure levels. The SMBP (Self-Measured Blood Pressure)
program was initiated in community health centers in 2021
with the goal to reduce blood pressure levels in the
underserved, vulnerable, and low income communities.
Medically diagnosed hypertension patients with three or
more readings that were above 140/90 were included in the
study. Patients with SMBP devices received an advantage as
care teams and continuous monitoring took place to ensure
compliance. With the additional factors present, patients with
the devices experienced lower blood pressure levels as
multiple blood pressure readings were allowed for inclusion
into the study. The decrease from 169/90 to 130/80 is
indicative that patients can control their hypertension rates
regardless of race, ethnicity, or socio economic status. Not having to physically take time off from work, pay a deductible,
or worry about missing an appointment, the SMBP devices
are free and are monitored by the care team on a frequent
basis. Notably, there were strong correlations between race,
ethnicity, FPLs (Federal Poverty Levels), nutrition counseling,
city of origin, age, and food insecurity. This significance
addressed all three research questions but ruled out some
aspects of the study that included specific insurance coverage,
BMI percentage, and gender. Findings of this study illustrate
those programs such as the SMBP program, increase
participant’s motivation to monitor their BP levels and lead
healthier lifestyles.
Influencing Ethno geriatrics
The intervention of giving patients a SMBP (Self-Measured
Blood Pressure) device addresses the main concerns
surrounding hypertension and health factors. The Theory of
Planned Behavior (TPB) with the overarching themes of “circle
of culture,” attitude, perceived behavioral control, and
subjective norms play a large role in how individuals in
different cultures view and choose to believe in certain topics.
Although the theory of planned behavior was not studied
directly, the topic proved to be heavily embedded within the topic of Ethno geriatrics. The circle of culture theme
embodies the collective identity of a person. This theory,
proposed by Icek Ajzen has been applied to healthcare to
determine important variables that affect self-care behaviors
in the control of hypertension. Future research should include
the TPB model for a deeper understanding of patient beliefs
and behaviors.
Conclusion
The approach to hypertension in the low income,
underserved, and vulnerable communities are highlighted
amongst those patients who have additional factors that
affect their overall HTN levels. Race and ethnicity are not
modifiable risk factors, but other factors could be amenable
to intervention. Risk factors that emerge and impact
compliance are within the ethno geriatrics topic. Further
discoveries on topics such as theory of planned behavior gives
the researchers a guidebook to understanding more about
individuals who may have incurred or passed down trauma
from previous experiences. These experiences shape the
cultural viewpoint of individuals and their respective
communities. This project increased the understanding of
SDOH and economic barriers of individuals who need
additional assistance and will reach beyond the clinical walls.
Although the needs may differ from patient to patient, there
is a tremendous opportunity to expand on the Community
Centered Health Home (CCHH) model. This model requires
traditional silos to be broken down so that the patient’s needs
can be addressed. There is a tremendous opportunity to
expand on this scope of work and dive into these
communities to further investigate this disease and causes of
it. Challenging as it may be, data is still needed from large,
randomized control groups so that the approach taken can be
inclusive of patient care.
Limitations
With the population being low-income and underserved,
there are various disadvantages that hindered participation.
While smart phones are common, patients would need access
to Wi-Fi, cellular signals that are not limited, and the
capability to know how to work the device. These three items
alone can eliminate 50% of the eligible population.
Additionally, patient education is critical when discussing the
benefits of the SMBP program. With the ever changing
landscape of telehealth and technology, patients who are not
familiar or comfortable with this type of data sharing most
likely opted to not participate.
References
- Angier H, Huguet N, Marino M, Green B, Holderness H, et al. (2019) Observational study protocol for evaluating control of hypertension and the effects of Social Determinants. BMJ Open. 9(3):025975
[Crossref][Googlescholar][Indexed]
- Beltran S, Pharel M, Montgomery CT, Lopez-Hinojosa IJ, Arenas DJ, et al. (2020) Food insecurity and hypertension: A systematic review and meta-analysis. Plos One. 15(11):0241628.
[Crossref][Googlescholar][Indexed]
- Booth JN, Li J, Zhang L, Chen L, Muntner P, et al. (2017) Trends in prehypertension and hypertension risk factors in US adults. Hypertension. 70(2):275–284.
[Crossref][Googlescholar][Indexed]
- CDC (2021) About Social Determinants of Health (SDOH). Centers for Disease Control and Prevention.
- Donneyong MM, Chang TJ, Jackson JW, Langston MA, Juarez PD, et al. (2020) Structural and social determinants of health factors associated with county level variation in non adherence to antihypertensive medication treatment. Int J Environ Res Public Health. 17(18):6684.
[Crossref][Googlescholar][Indexed]
- Dorsey ER, Topol EJ (2020) Telemedicine 2020 and the next decade. The Lancet. 395(10227):859.
[Crossref][Googlescholar][Indexed]
- Fang J, Gillespie C, Ayala C, Loustalot F (2018) Prevalence of self reported hypertension and antihypertensive medication use among adults aged ≥ 18 years United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 67(7):219-224.
[Crossref][Googlescholar][Indexed]
- Gabriel AC, Bell CN, Bowie JV, LaVeist TA, Thorpe RJ (2020) The role of social support in moderating the relationship between race and hypertension in a low-income, urban, racially Integrated Community. J Urban Health. 97(2):250–259.
[Crossref][Googlescholar][Indexed]
- Hensley C, Heaton PC, Kahn RS, Luder HR, Frede SM, et al. (2018) Poverty, transportation access, and medication Nonadherence. Pediatrics. 141(4):20173402.
[Crossref][Googlescholar][Indexed]
- Ho PM, Bryson CL, Rumsfeld JS (2009) Medication Adherence. Circulation. 119(23):3028–3035.
[Crossref][Googlescholar][Indexed]
- Iqbal AM (2021) Essential hypertension. Lancet. 370(9587):591-603.
[Crossref][Googlescholar][Indexed]
- James H Jones (1982) Bad Blood: The Tuskegee Syphilis Experiment. New York: Free Press. Am Hist Rev. 87(2):-558.
[Crossref][Googlescholar]
- Kang A, Dulin A, Risica PM (2020) Relationship between adherence to diet and physical activity guidelines and self-efficacy among black women with high blood pressure. J Health Psychol. 27(3):663-673.
[Crossref][Googlescholar][Indexed]
- Kithas PA, Supiano MA (2015) Hypertension in the Geriatric Population. Med Clin N. 99(2):379-389.
[Googlescholar][Indexed]
- Kountz DS (2004) Hypertension in ethnic populations: Tailoring treatments. Clin Cornerstone. 6(3):39-48.
[Crossref][Googlescholar][Indexed]
- Malayala SV, Vasireddy D, Kadali RAK, Alur RS, Koushik K (2020) Healthcare Access in Medically Underserved Areas During the COVID-19 Era: An International Medical Graduate Perspective From a Rural State. Cureus. 12(12):12254.
[Crossref][Googlescholar][Indexed]
- McNeely CL, Schintler LA, Stabile B (2020) Social Determinants and COVID‐19 Disparities: Differential Pandemic Effects and Dynamics. World Med. 12 (3):206-217.
[Crossref][Googlescholar][Indexed]
Citation: Williams JM, Garza D (2023) Socioeconomics, Ethno geriatrics, and Social Determinants of Health: Correlations in Hypertension Patients. J Healthc Commun. 8:8003
Copyright: © 2023 Williams JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.