Key words
dementia, South Asian and white older
people
Introduction
This study addresses South Asian and white older
people’s views about the nature of dementia, about
its causes and available treatments, and about who
should care for people with dementia. Over the last
decade the number of South Asians in the population has increased considerably, especially in London, and
the number of South Asians presenting with dementia
is therefore certain to increase, with major implications
for health services (Lowdell et al, 2000). Rait
et al (1996) graphically refer to the ‘triple whammy’ of age, ethnicity and socio-economic deprivation experienced
by older people from minority ethnic groups
and other researchers (Chaudhry and Au, 1994; Rait
and Burns, 1997) also note that minority ethnic groups
tend to be under-represented as users of psychiatric
services. The possibility that there are significant
hindrances to South Asian elders who might need
care for dementia is becoming all the more important.
The age structure is changing, and there is likely to be
an increase in the need for formal care in ethnic
minority communities that have hitherto been assumed
to be reliant on the informal care structures of extended
families (Department ofHealth, 1998).Although
some studies have shown that the majority of South
Asian older people do live with their children or
extended families (Bowes and Dar, 2000; Lowdell
et al, 2000) researchers note this way of life may be
diminishing, and also highlight changing intergenerational
relationships and the growing need for
assistance from outside the family (Chaudhry and
Au, 1994; Guglani et al, 2000; Rait et al, 2000).
Goldberg and Huxley’s framework for understanding
the recognition and treatment of mental health
problems describes a number of ‘filters’ that operate in
the ‘pathway to care’ (Goldberg and Huxley, 1980).
These operate at the level of the individual, the general
practitioner (GP) and the mental health service. Bhui
and Bhugra (2002) suggested a number of cultural
factors that should be considered when looking at how
these filters operate, and that have to be understood by
service providers. These filters include culture-specific
beliefs about when a mental health problem exists;
what stigma attaches to it; whom it is appropriate
to consult; language barriers; and perceptions of the
appropriateness of services. All these factors impact on
the individual-level filter, and some also may influence
the willingness of GPs to refer on to health or social
services (Donaldson, 1986; Beliappa, 1991; Chaudhry
and Au, 1994; Ebrahim, 1996; Bhui, 1997; Bhugra,
2002; Bhui and Bugra, 2002). Other research suggests
that current services may not be seen as acceptable by
the South Asian population, and that there is a considerable
amount of work to do in building culturally
sensitive services (Department of Health, 1998; Bowes
and Dar, 2000; Seabrooke and Milne, 2004).
There is little extant published research on dementia
in minority ethnic groups, less still on South Asians
(Adamson, 2001). A study in the United States identified
a variety of cultural understandings of dementia
in minority groups and found that the meanings that
different ethnic groups assign to dementia influence
their care-giving and help-seeking behaviour, for example
whether formal approaches to healthcare
providers such as the GP are seen as appropriate
(Dilworth-Anderson and Gibson, 2002). In the UK, a
small-scale qualitative study found that overall awareness
of dementia among South Asians was low, and explanations tended towards social conditions, other
medical conditions, the effect of medication, and
spiritual problems (Adamson, 2001). Another smallscale
study found that GPs thought that South Asians
perceived dementia as a normal part of ageing, and
therefore sought help late in the disease process. They
also thought that there was significant stigma attached
to dementia and a lack of culturally appropriate services
(Seabrooke and Milne, 2004). Adamson’s study (2001)
raises the question that this lack of understanding and
beliefs about dementia may also be prominent in the
white majority population. However, Rait and Burns
(1997) point out that because fewer people have lived
to old age in South Asian countries in the past and
people may have migrated before their parents grew
old, many South Asian older people may not have had
the experiences necessary to recognise dementia, and
may have a different appreciation of treatment. These
factors could compound reluctance on the part of
older people from minority ethnic groups and their
carers to seek help from mental health services.
Despite the recognition of these issues, the number
of studies of dementia involving people fromminority
ethnic groups remains low. It has frequently been stated
that more studies are needed in this area, particularly
studies with adequate numbers to allow meaningful
comparisons of white and non-white subjects
(Dilworth-Anderson and Gibson, 2002; Hinton, 2002;
Lampley-Dallas, 2002). Qualitative research methods
have been proposed as a useful way of achieving this
type of understanding, as such methods can allow
differences that matter to be seen both within and
between groups, but these methods have been underutilised
in the past (Hinton, 2002). This study adopted
a mixed method approach: using qualitative analyses
to gain a thorough understanding of participants’
views, but also utilising quantitative analyses in the
final stages to establish the magnitude of any differences
in views between the South Asian and white
older people. Hanson et al (2005) state that utilising
both quantitative and qualitative analyses in a study
can enrich results in ways that one method would not
allow.
Purpose of the study
The current study was part of South West London and
St George’s Mental Health NHS Trust’s programme
to improve services for people from minority ethnic
groups. The study aimed to provide more information
about the mental health needs of South Asian older
people, and to contribute relevant information to the
development of pathways to care for depression and
dementia as required by the National Service Framework
for Older People (Department of Health, 2001).
This qualitative study was part of a larger study, and used open-ended questions on dementia to investigate
whether South Asian older people have different views
from older people in the white majority population
about the causes of and treatment for dementia, and
whether this would lead them to consider that different
forms of help would be appropriate.
The following specific questions were tested.
• Will South Asian older people have different views,
in comparison to those of white older people, about
the nature of dementia?
• Will South Asian older people have different views,
in comparison to those of white older people, about
the causes of and treatments for dementia?
• Will South Asian older people see dementia as a
problem that should be managed by the family
rather than by the state?
Methods
Local research approval
Following South West London and St George’sMental
HealthNHSTrust procedure, the study was submitted
to both the local research ethical committee and the
research and development committee of the trust. The
trust accepted it onto its Culyer database.
Study design
The aspect of the research reported here was a qualitative
study of a community sample of South Asian
and white older people in two South London
boroughs, Merton and Wandsworth. Semi-structured
interviews using open-ended questions were used to
explore participants’ views about dementia. Interviews
were conducted in one of four Asian languages,
Gujerati, Hindi, Punjabi and Urdu, or in English.
Participants and sample populations
There were 192 participants, 96 South Asian and 96
white older people, between the ages of 58 and 85 years
living in the community. The South Asian population
comprised people who defined themselves as originating
from the Indian subcontinent and Sri Lanka, but
because of routes of migration may have been born
elsewhere such as East Africa. The white population
only included people born in Great Britain whose first
language was English. They were chosen from GP lists
to be approximately similar to the South Asian sample
with respect to sex, age and area of residence.
The South Asian sample was recruited through two
local South Asian organisations and three local GP
practices. The white sample was recruited through the same GP practices as the South Asian sample. Only
one person from any household was interviewed.
None of the participants was known to have a diagnosis
of dementia.
Procedures
Translation, user consultation and pilot
work
In order to translate the questions from English to the
four Asian languages, a careful process of translation
and back-translation was completed by an assistant
psychologist working with a number of people from
the South Asian community. For each language the
important issue was to find the most appropriate term
for ‘dementia’. This was clarified through pilot work,
which was mainly in the form of consultation with
South Asian older people. The interview as a whole
was piloted with two older people.
Conduct of interviews
The interview was completed face to face with participants
by a trained interviewer fluent in the participant’s
preferred language, and most were conducted
in the participants’ homes, unless otherwise requested.
Interviews were only completed after a consent form
was signed. Seven open-ended questions about dementia
formed part of the interview schedule and a
verbatim written record of the responses was made.
Analysis
All 192 responseswere transcribed as they were recorded
on the interview schedule. The analysis incorporated
three steps. Firstly, a thematic analysis was carried
out, which drew on the procedure of Interpretative
Phenomenological Analysis to identify the main
themes from the transcripts. These themes were then
entered into NVivo software in order to conduct a
content analysis. Finally, the Z test for difference in
proportions was employed to assess the differences
between the two groups from the content analysis.
Thematic analysis
A thematic analysis attempts to glean the main themes
from interview responses, to give an overall summary
and representation of sayings, feelings, beliefs and
metaphors expressed by respondents. These themes
can incorporate sub-themes, and can be titled to best
reflect the views they are encompassing. The themes
then form the categories by which the text can be
indexed. The steps taken to identify the emerging
themes from the interview responses were based on
the process of interpretative phenomenological analysis
(Smith, 1996a). This methodology is committed
to understanding and foregrounding respondents’ perspectives through the interpretation of the investigator.
The outcome is therefore considered a coconstruction
between the participant and the researcher
as it emerges from the researcher’s engagement with
the transcripts (Smith, 1995). The steps of the thematic
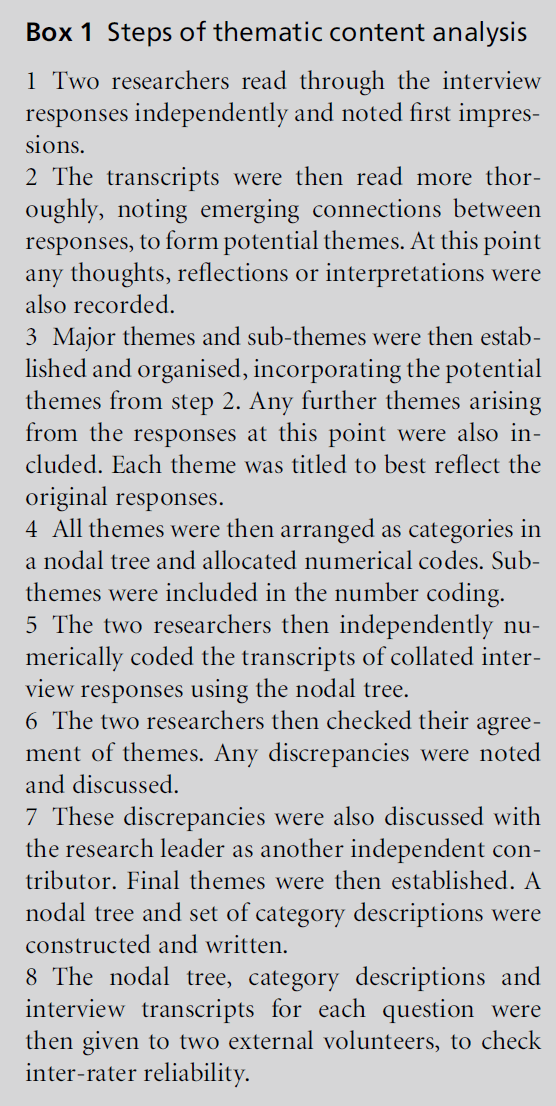
analysis are delineated in Box 1.
Box 1 :Steps of thematic content analysis
Validity and reliability
Validity can be improved in a number of ways in
qualitative research, all of which require the exercise of
judgement by both the researcher and the reader
(Mays and Pope, 2000). Two suggested methods of
assessing internal validity and reliability of qualitative
research are internal coherence and the presentation
of evidence (Smith, 1996b). It is also important to
consider personal and intellectual biases of those
conducting the study (Mays and Pope, 2000).
INTERNAL COHERENCE
Internal coherence refers to whether the themes
interpreted from the transcript are internally consistent
and are justified by the original responses.
Throughout the process of the analysis, two researchers
worked independently on the transcripts and discussed
the emerging themes.
RELIABILITY
While analysis based on Interpretive Phenomenological
Analysis does not normally include a test of interrater
reliability, the researchers thought it was important
to ascertain the degree to which the transcripts
would consistently be assigned to themes/categories
by independent readers unconnected with the study or
its hypotheses. It was thought important to establish
reliable themes, as the analysis was to be continued
using a content analysis and statistical tests. Inter-rater
reliability was determined: for a quarter of the responses,
two external raters were allocated to look at
each question and were provided with details of the
themes and the transcripts. Inter-rater reliability was
set at 75% (Krippendorff, 1981). If this level was not
reached, themes were adapted or merged and sent out
to a further two raters. This formed part of the
evolving process of the analysis. Eventually a final set
of themes was reached for each question.
PRESENTATION OF EVIDENCE
The presentation of evidence suggested by Smith
(1996b) allows the reader to make some assessment
of the interpretation made by the researchers. The
themes and nodal trees are presented in boxes, and the
text and quotes from respondents are included with
notes of the theme they illustrated.
RESEARCHER CHARACTERISTICS, PRIOR
ASSUMPTIONS AND EXPERIENCES
It is noted that the researchers and raters were all from
a different age group from the participants and from
different ethnic backgrounds from the South Asian
participants in the study. Therefore, it is likely that
differences existed in the assumptions and world views
of the researchers and participants. The researchers
also approached the transcripts with an existing contemporary
framework of older adult psychology, and
were interested in any differences between the two
groups. While the dataset was analysed for themes as a
whole and without necessarily knowing the ethnicity
and sex of the participants, it is acknowledged that the
researchers’ assumptions will have influenced theme
development to some degree.
Content analysis
Once the themes from each question achieved interrater
reliability of 75% or above, the nodal trees were
constructed in the QSR NVivo program. Seven nodal
trees were constructed in total. The transcripts were
also entered into the database and coded by theme/
category. NVivo permitted a comparison of patterns
and frequencies between the South Asian and white
samples. Attributes of the interviewees such as personal
experience could also be factored into this
analysis. Although considerable variation in the patterns
and frequencies within the two groups is highly
likely, the current focus was on patterns and frequencies
between groups.
Quantitative analysis and statistical tests
In the final stage of analysis a quantitative method of
analysis was applied.Where, through content analysis,
the frequencies of themes appeared different between
the South Asian and white older people, statistical
comparisons were conducted to allow some understanding
of the magnitude of the differences. This
quantitative analysis was seen as augmenting the
qualitative analysis: thematic content analyses enable
a thorough understanding of participants’ responses;
quantitative analyses then enable some understanding
of the generalisability of findings from samples to
populations (Hanson et al, 2005). The large sample
sizes were seen as contributing to the appropriateness
of this final-stage analysis. When comparing responses
between the two groups, the Z test for difference in
proportions was used to test for a significant difference
(P < 0.05). When the difference was significant this is
stated in the text. A table of the Z values is included at
the end of the results.
Findings
Demographic information
The participants were selected so that the groups were
similar in age (average = 69 years) and gender mix
(49 men and 47 women in each). Almost 80% of the
South Asian sample was Muslim (47.9%) or Hindu
(31.3%); 96.9% of the white sample was Christian.
The South Asian participants practised their religion
more frequently. The majority of the South Asian
sample described themselves as Indian (42), Pakistani
(31) or Sri Lankan (7); the largest language groups
were Urdu (29), Gujerati (21) and Punjabi (19). Participants
had lived in the UK between 4 and 56 years
(average = 30 years), and most came into Great Britain
from either Pakistan (34), East Africa (32) or India (17).
South Asians were less likely to be single (3%
compared with 18%), and more likely to be widowed than their white counterparts. They were no more
likely to live alone than white participants (27.1% in
each sample), but were more likely to live as part of an
extended family (41.6% compared with 9.4%). Similar
proportions in each group were educated beyond
secondary level (South Asians 39.6% and white participants
38.5%), but South Asians were more likely to
have had either no formal education or to have only
attended primary school (11.5%compared with 0%).
Almost 80% of all participants were retired. More
from the South Asian sample had never been in paid
employment (15.6% compared with 2.1%), and more
of the white group remained in employment (14.6%
compared with 3.1%). From the South Asians who
had worked, more were homemakers (16.7% compared
with 4.2%) and professional/managerial workers
(43.8% compared with 29.2%), and fewer were manual
workers than the white participants (11.5%compared
with 32.3%). Although this information provides an
overall comparison of the two groups, it is also
acknowledged that there was diversity within both
groups.
Thematic content analysis
Nature of dementia: what do you think
are the kinds of things that happen
to people who have dementia?
What do people with dementia
have difficulty with?
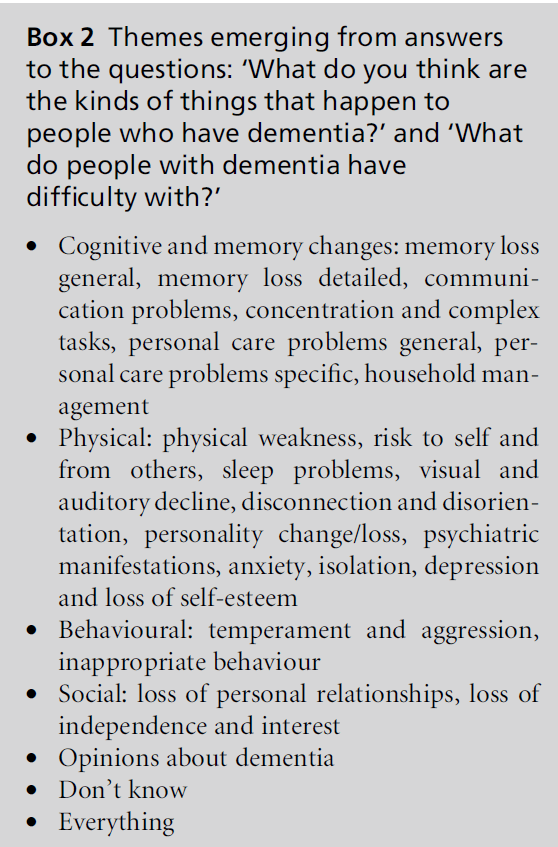
As similar themes emerged in the answers to both
questions (Box 2), these answers were analysed together.
Both South Asian and white older people commonly
mentioned memory problems. Many people
just used general terms such as ‘forgetfulness’ or ‘loss
ofmemory’ without elaborating (32 South Asian (SA),
33 white respondents), but more people from both
groups mentioned specific memory problems such as
forgetting names, no longer recognising people, or
forgetting to eat meals or take medication (45 SA, 61
white respondents).
[They] forget about things that happened in their lives,
lack of recognition of their own relatives, don’t remember
anything about past and present ... (SA man; theme:
memory loss detailed)
[They] forget. [They] don’t remember people or places
they’ve been or things they’ve done ... (white woman;
theme: memory loss detailed)
Overall, however, significantly more white (94) compared
with South Asian (77) older people mentioned
memory problems.
Both South Asian and white older people also
frequently mentioned personal care problems, and
these were also more likely to be described by the
respondents in specific ways such as problems with cooking, washing and toileting (29 SA, 45 white
respondents) rather than in more general terms such
as stating ‘they cannot take care of themselves’ (14 SA,
17 white respondents). For both memory and personal
care problems, white respondents were significantly
more likely than the South Asian group to
describe the effects of dementia in a detailed way
(45 SA, 61 white (memory); 29 SA, 45 white (personal
care problems)).
Box 2 :Themes emerging from answers
to the questions: ‘What do you think are
the kinds of things that happen to
people who have dementia?’ and ‘What
do people with dementia have
difficulty with?'
The other differences in the responses between the
two groups were that white older people were significantly
more likely than the South Asian group to
mention the presence of other difficulties, for example
that people with dementia may become disorientated
and disconnected from reality (12 SA, 23 white respondents),
a risk to themselves and from others (11,
22), or lose their independence and interest (5, 13).
‘My mother would go out in the night. [She would] forget
to turn the kettle off and burn it [and] cook dinner at the
wrong times of day. People outside don’t understand ...’
(white woman; themes: disconnection and disorientation,
risk to self and from others, inappropriate behaviour)
Significantly more South Asian (27) than white older
people (1) stated they did not know what happened to
people with dementia or did not know what people
with dementia would have difficulty with. Twelve of
these South Asian respondents answered that they did
not know in response to both the questions.
What do you think are the things that
cause dementia?
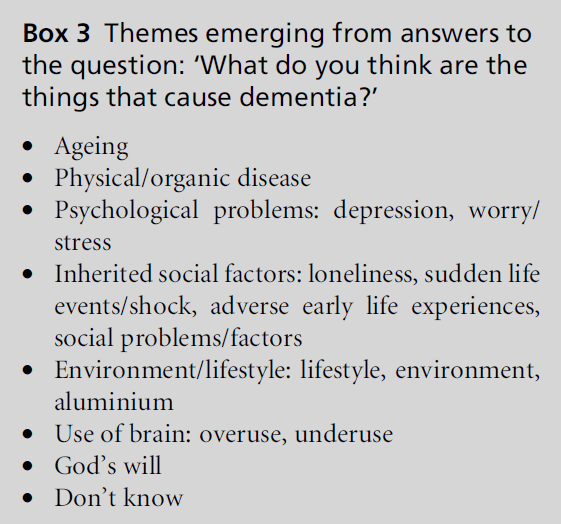
Most people interviewed were able to give some
account of what they believed caused dementia (83
SA, 86 white older people). Themes that emerged are
shown in Box 3.
Box 3 :Themes emerging from answers to
the question: ‘What do you think are the
things that cause dementia?'
South Asians (47) were much more likely than white
older people (22) to see dementia as part of the normal
ageing process.
‘... when you grow old certain parts of your body go,
similarly your brain has this ... it loses stimulation, brain
cells die ...’ (SA woman; theme: ageing)
‘[It is the] natural process of decay and people becoming
old ...’ (SA man; theme: ageing)
White older people (45) mentioned physical disease/
organic causes without mentioning ageing much
more frequently than South Asians (17).
‘... cells connected with memory cease to function, not
getting messages or dying off, chemical lack or physical
loss ...’ (white woman; theme: physical/organic disease)
‘... can’t be old age because it happens to young people
too. Something in the brain, something breaks down.
Wouldn’t say it was a way of life or anything like that ...’
(white woman; theme: physical/organic disease)
Far fewer South Asian and white older people mentioned
other causes such as sudden life events or shock
(9, 12), loneliness (8, 8) or worry and stress (12, 6).
Do you think that there are any
treatments for dementia?
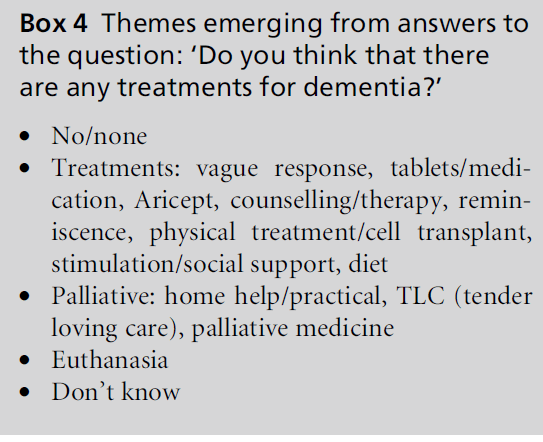
One-third of all South Asian respondents (32) stated
they did not know if there were any treatments for
dementia; this compared with just under one-sixth
(15) of the white respondents. Almost another third of
the South Asian respondents (28) believed there was
no treatment for dementia. A similar number of white older people also believed there was no treatment
available (23). Themes that emerged are shown in Box 4.
Box 4 :Themes emerging from answers to
the question: ‘What do you think are the
things that cause dementia?'
‘... don’t know, don’t think anything can be done. People
just go downhill. I’ve never seen anyone ever come out of
it ...’ (SA woman; theme: no/none)
‘... don’t think so. I’ve never heard of anyone getting it and
being cured ...’ (white man; theme: no/none)
Twenty-two white older people mentioned medication
as a treatment for dementia. This contrasted
with only seven South Asian respondents. However, it
is noted that the health authority agreement that
donepezil could be used locally was reported in the
newspaper in January 2001. The NICE guidelines
(National Institute for Clinical Excellence, 2001) recommending
donezepil as a treatment for dementia
were published in mid-January 2001 and reported in
the newspapers at the end of January 2001. These publications
could have influenced respondents’ attitudes
towards whether dementia was treatable and what
type of treatment was available for dementia, since
more white respondents interviewed after the publications
compared with those interviewed before the
publication date stated that they believed medication
was a treatment for dementia. Also, more white than
South Asian respondents interviewed after the publication
date mentioned medication as a treatment, and
this may reflect differences in reading of the publications
between the two groups. Interviews with 81
South Asian and only 18 white older people had been
completed by this time.
‘... Yes, finding [the] right medication to replace what’s
decreasing in the body, so memory is aided ...’ (white
woman; theme: tablets/medication)
‘What I read about, yes, drugs to control the brain cells
from dying off too quickly ...’ (white man; theme: tablets/
medication)
Twelve South Asian and 14 white older people gave
responses indicating that they did believe there was treatment available, but they did not state what that
treatment was or did not know what it might involve.
‘... think they can, why not? I can’t say what they are ...’ (SA
woman; theme: treatments, vague response)
‘... they try to treat people. Don’t know of any particular
treatment. They are in the stage of trial and error because
they don’t know enough about it ...’ (white man; theme:
treatments, vague response)
Both groups discussed other types of intervention,
such as counselling, social support and palliative
medicine, much less frequently.
Caring for people with dementia
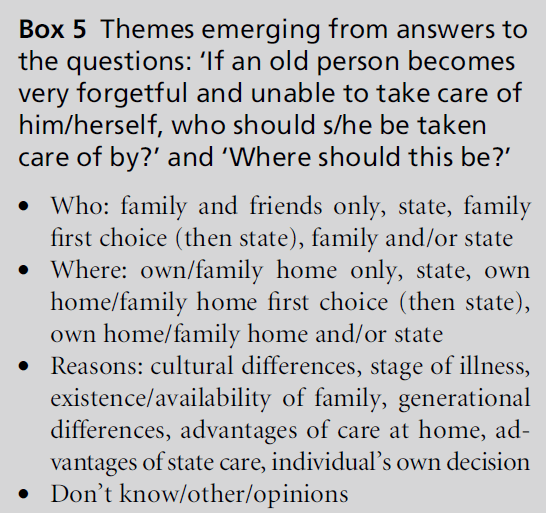
The respondents were asked two separate questions:
‘If an old person becomes very forgetful and unable to
take care of him/herself, who should take care of him/
her?’ and ‘Where should this be?’. There were clear
differences between the South Asian and white older
people’s responses and this was true for their responses
to both questions. Themes that emerged are
shown in Box 5.
Box 5 :Themes emerging from answers to
the questions: ‘If an old person becomes
very forgetful and unable to take care of
him/herself, who should s/he be taken
care of by?’ and ‘Where should this be?’
Over one-third (37) of the South Asian older people
said that only family or friends should care for people
with dementia. This compared to under a tenth (9) of
the white respondents.
‘... if the family is there, they should look after them and
also close friends ...’ (SA woman; theme: family and
friends only)
Following a similar pattern, nearly one-half of all
South Asian respondents (45) believed care should
only be provided in the person’s own or family home,
a significantly greater number than the white respondents
(18).
‘[They should be cared for in their] home, either by family
or by outside carer[s] coming into the home ...’ (SA
woman; theme: own/family home only)
Twenty-seven South Asian older people stated that the
family was the first choice in terms of caring for the
person with dementia, followed by the state as second
choice. Thirty-nine white older people gave this response,
the most frequent response by the white
group. There was no significant difference between
the two groups.
‘... family. If family is not there it is the duty of the state ...’
(SA woman; theme: family first choice, then state)
‘[They should be cared for] firstly by the family, afterwards
[by] social services. [It is] hard for family to deal
with dementia so [they should do] as much as they can,
then [the person should be] put into care ...’ (white man;
theme: family first choice, then state)
Similarly, over one-third (34) of the white respondents
believed the person’s own home or family home
should be the first choice for where they are cared for,
but that other options were available. One-quarter
(24) of South Asian respondents believed this. There
was no significant difference between the two groups.
‘[It] depends on [the] circumstance. If they can be treated
in [their own] home it is preferable ... even if they don’t
know where they are they can sense where they are ...’
(white man; theme: own home/family home first choice,
then state)
Twenty-six of the white respondents believed the state
should care for people with dementia, the second most
frequent response by white older people. Only nine
South Asian older people gave this type of response.
‘... they should be taken into care where they can get
medical needs and day-to-day needs taken care of ...
somewhere where they can have 24-hour care. I don’t
think family should necessarily be burdened with them
unless they volunteer ...’ (white man; theme: state)
Following a similar pattern, almost one-third (29) of
white older people believed care should be provided in
state facilities, a significantly greater number than
South Asian respondents (10).
Some respondents also gave reasons for their answers.
When discussing who should care for the person with
dementia, only South Asian older people mentioned
cultural reasons (8 and 0 respectively).
‘... family. In our culture family is responsible. In this
country the government is responsible ...’ (SA woman;
themes: family and friends only, cultural differences)
‘[It] depends on the circumstances. [If you] think of our
background, we think it should be the family, but young
[people] have jobs and problems [and you’re] not always
living together, so it’s difficult ...’ (SA woman; themes:
family and friends only, existence/availability of family)
White older people (15) were more likely than South
Asian older people (2) to mention the stage of the
illness as being a contributing influence to their views
both about who should take care of the person with dementia and about where this care should be provided.
What things would make it difficult to
care for an old person who had dementia
living in their own home or living with
their family?
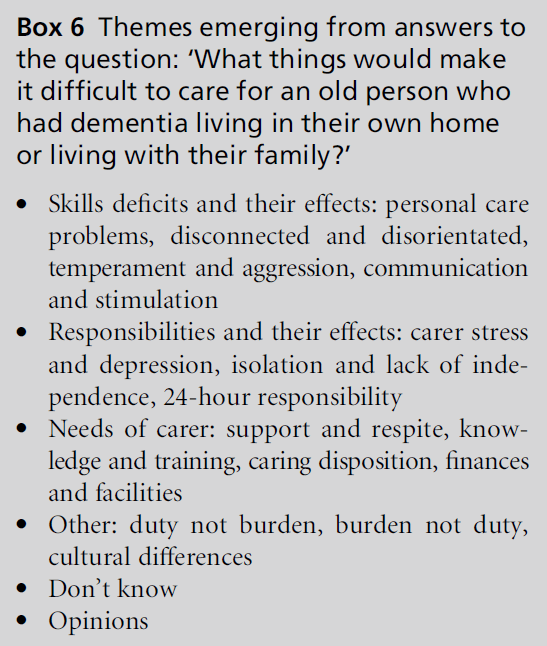
The perceptions of factors that may make it difficult to
care for a person with dementia were very similar
between the South Asian and white older people: there
were more similarities in the answers of the two
groups than there were differences. Themes that
emerged are shown in Box 6.
Box 6 :Themes emerging from answers to
the question: ‘What things would make
it difficult to care for an old person who
had dementia living in their own home
or living with their family?’
Approximately two-thirds of both South Asian (64)
and white (62) respondents thought that difficulties
with personal care would make it difficult for a person
with dementia to be cared for in their own home.
Almost half of the white respondents (45) and onethird
of the South Asian older people (34) also stated
that itwould be a 24-hour responsibility. There was no
significant difference between the two groups.
‘... they need someone there all the time to make sure
medicines are taken on time, feed on time, hygiene and
safety. You need someone there all the time ...’ (SA man;
themes: personal care problems, 24-hour responsibility)
‘... carers have to be young and committed to looking after
[the] person 24 hours a day [and] devoted to the task of
keeping them fed and clean and getting them up ...’ (white
woman; themes: caring disposition, 24-hour responsibility,
personal care problems)
Temperament and aggression were also mentioned a
number of times by both South Asian (14) and white
(18) respondents.
‘... they have to be very tolerant as sometimes the older
person can be rude and aggressive ...’ (SA woman; theme:
temperament and aggression)
White older people (23) also considered carer stress
and depression to be a factor that would make caring
for a person with dementia difficult; this compared
with only nine South Asian respondents.
Although the numbers are small, significantly more
white (7) than South Asian (1) older people also mentioned
that lack of appropriate knowledge and training
on the part of the carer would make caring
difficult. Three South Asian older people mentioned
cultural differences. None of the white respondents
mentioned this subject.
‘[The] attention of the family [would make it difficult]. In
western societies strong family ties don’t exist.’ (SA man;
theme: cultural differences)
‘... in Asian countries it is possible to look after an
individual, but not here as no one has time ...’ (SA man;
theme: cultural differences)
When might someone go into a nursing
home?
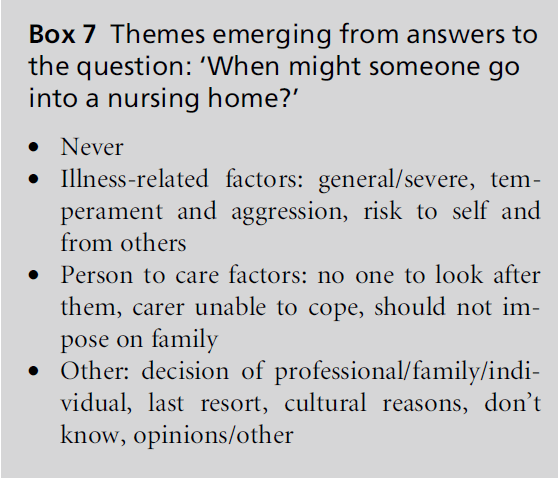
Themes that emerged in response to this question are
shown in Box 7.
Box 7 :Themes emerging from answers to
the question: ‘When might someone go
into a nursing home?’
The three most frequent responses were the same for
South Asian and white respondents. Firstly, both
South Asian (33) and white older people’s (39) most
frequent response was that people were most likely to
go into a nursing home in the later stages of dementia.
‘... when their condition gets very bad and no one is able to
take care of them and they need very specialised care ...’
(SA woman; theme: illness-related factors general/severe)
‘... in the later stages, when the person gets so bad they
need someone to watch over them 100% of the time ...’
(white man; theme: illness-related factors general/severe)
Secondly, one-third of South Asian older people (32)
believed people were most likely to go into a nursing
home if there was no one to look after them. Under
one-quarter (21) of white older people stated this.
Thirdly, 33 white older people believed that people
might go into a nursing homeif the carer was unable to
cope; significantly fewer South Asians (19) gave this
response.
‘... when you know that you can no longer cope. When it’s
affecting you, your health. When they become a worry to
you ...’ (white woman; theme: carer unable to cope)
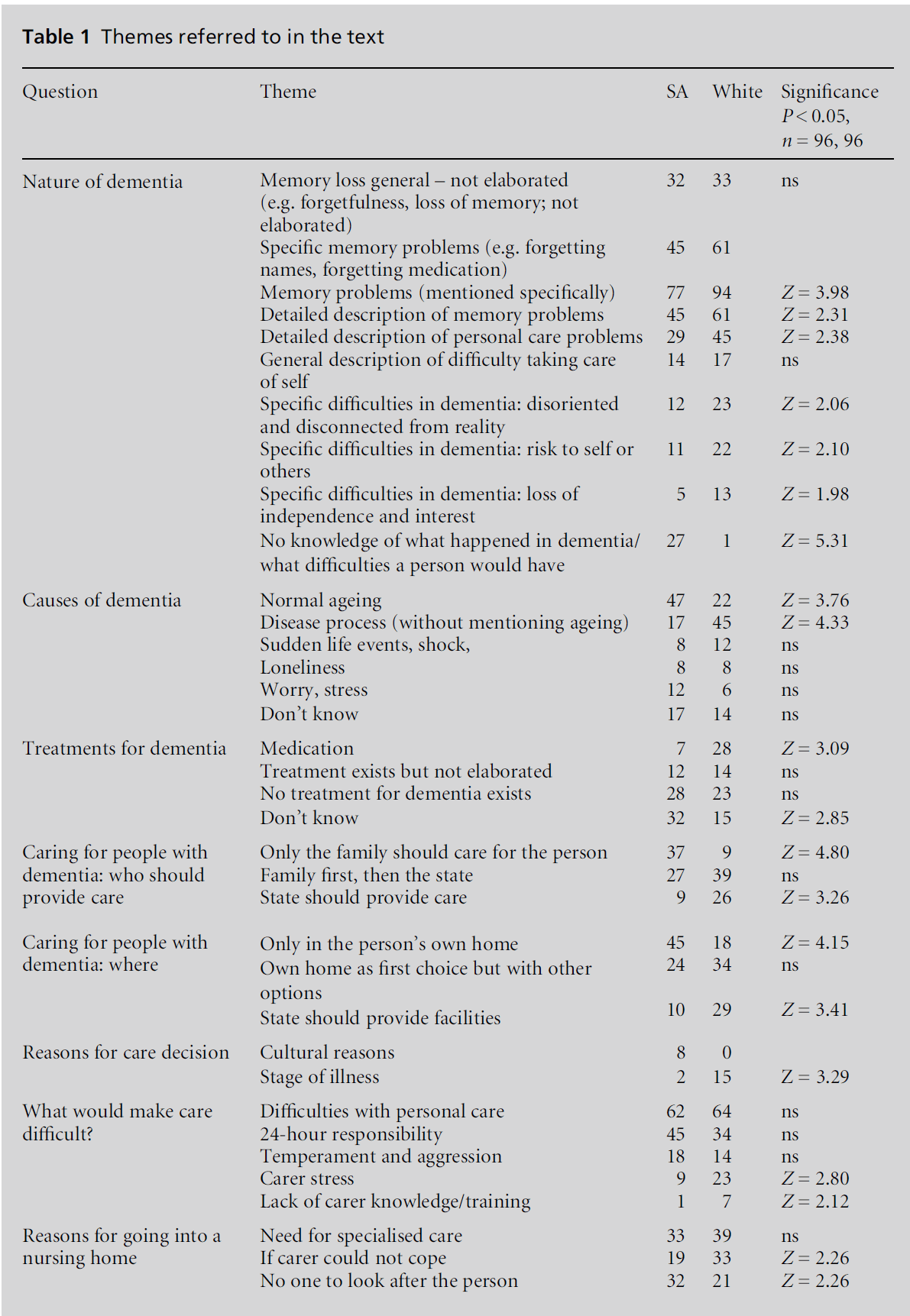
The themes referred to in the interviews are summarised
in Table 1.
Discussion
This study specifically tested three main questions:
will South Asian older people have different views
compared with white older people about (1) the
nature of dementia; (2) the causes of and treatments
for dementia; and (3) who should care for people with
dementia? The findings outlined above are discussed
here.
Knowledge about the nature of
dementia
Overall, these findings corroborated those of Adamson
(2001) demonstrating that South Asian older people
do have a poorer understanding of the nature of dementia
compared to white older people. Interestingly,
the South Asian and white older people did not have
different views about how dementia presents, with the
majority of both groups mentioning memory and
personal care problems; rather, the South Asians had
an overall poorer understanding. On the one hand this
lack of knowledge could be interpreted in line with
Rait and Burns’ (1997) ideas that, because many South
Asian older people may have migrated before their
parents grew old, they may not have had experiences
of dementia. On the other hand it could be argued
that it is the effect of a culture more influenced by
western science that has enabled the white older
people to have a greater understanding of and more
familiarity with dementia. In addition, as people from
the same majority western culture in which the study
was conducted, the white older people may just have
been those most able to explain the nature of dementia
in a manner congruent with the western, medical
understanding of it. However, this still has important implications for how to detect dementia in South
Asian older people living in western societies.
Table 1: Themes referred to in the text.
The causes of dementia
The South Asian respondents were significantly more
likely than the white older people to perceive dementia
as being caused by the ageing process, whereas the
most frequent response by the white group was that
dementia was caused by a physical, organic disease,
again reflecting a much clearer understanding about
dementia. These findings provide support for the GP’s
beliefs in Seabrooke and Milne’s (2004) study and
previous research that found people from non-western
cultures are likely to attribute dementia to the ageing
process (Dein and Huline-Dickens, 1997). Low numbers
of South Asians mentioned social factors as a
cause of dementia, in contrast with Adamson’s (2001)
and Beliappa’s (1991) findings that South Asians are
likely to attribute the causes of dementia to social
factors, intra-familial problems or loss events. It was
noticeable in this study that only eight South Asians
mentioned social problems; however, all of these
referred to family issues, for example ‘being let down
by your family’. The one white person who felt social
problems contributed to the onset of dementia mentioned
employment rather than family stressors.
The treatment of dementia
Both South Asian and white older people demonstrated
little understanding of available treatments.
From the minority of people who did believe there
were treatments, more whites mentioned medication,
indicating some differences in views about treatment
between South Asian and white older people. The
South Asian older people did not appear to think
medication was not appropriate, as Beliappa (1991)
found when questioning South Asians about mental
distress in general; their responses appeared more
indicative of a lack of knowledge about the available
treatments and perhaps about dementia in general. It
is plausible to consider that if an illness is considered
part of the ageing process, rather than caused by an
organic disease, then treatment with the use of medication
may be considered less relevant or just not
considered.
Caring for people with dementia
Most South Asian respondents felt that only family or
friends should care for people with dementia. Most
white older respondents felt that while family should
be the first choice, the state should also be available to
provide care. The South Asian responses could reflect
the tradition in South Asian families to ‘look after their own’ (Department of Health, 1998), but may also
reflect the fact that the South Asian older people did
not perceive dementia to be caused by an organic
problemamenable to medical treatment. On the other
hand, thewhite older people who did believe dementia
was caused by a physical problem that could be treated
medically were significantly more likely to think
people with dementia should be looked after by the
state, that is to say the medical and nursing professions.
It is also possible that the South Asian older
people were expressing unwillingness to access services;
as Bowes and Dar (2000) found. However, although a
number of South Asian older people qualified their
responses about who should care for a person with
dementia, with discussions about the duty of the family
and the differences between cultures in care-giving
practices, no respondents directly mentioned an unwillingness
to access services. In all, only eight South
Asians mentioned cultural factors.
In this study the beliefs of both the South Asian and
the white older people appear to be logically linked to
beliefs and knowledge about causes and available treatment.
We therefore conclude, in line with Dilworth-
Anderson and Gibson (2002), that the meanings
assigned to dementia are derived from cultural beliefs
and also relate to values and beliefs about care-giving
practices and who is seen as appropriate to provide
care and why, and that the latter may follow from the
former.
Implications for practice
In the context of Goldberg and Huxley’s (1980)
framework, this study demonstrates that in considering
a pathway to care for people with dementia, there
are clear filters operating at the individual level, and
that these are culturally related, demonstrated by the
difference in responses between the South Asian and
white older people. This supports Bhui and Bhugra’s
(2002) assertion that service providers need to acknowledge
culture when considering access to services.
South Asian older people are unlikely to present
to mental health services with concerns about dementia
if they believe that it is caused by the normal
ageing process; that is to say, that they do not perceive
it as a health problem and in addition they have
cultural beliefs that people should be looked after
within the family, and so do not perceive it as appropriate
to consult professional help and support. It is
important to emphasise that the South Asian older
people in this study did not perceive health services as
inherently inappropriate or culturally unacceptable;
rather, they were not seen as appropriate to the
problem of dementia. This has clear implications for
increasing education about dementia within minority
ethnic populations, particularly about its causes and available treatments. If knowledge about its organic
nature is increased, so too early presentation to health
services may increase. In addition, health providers,
particularly those in primary care, may need to be
more active in screening for dementia in minority
ethnic groups, and not expect difficulties associated
with dementia to be raised unprompted. Increased
education is also necessary within the majority population:
in this study there was also a lack of knowledge
about dementia among the white older people, particularly
about available treatments.
Conclusion
This study has added to the small body of research on
dementia in minority ethnic groups. The use of a
qualitative research approach has allowed meaningful
comparisons between samples from the minority and
majority populations, and facilitated exploration of
the reasons for people’s responses. Importantly, this
study has furthered understanding as to why South
Asians are under-represented in mental health services,
and revealed the areas of hindrance that will
need to be targeted to change this representation in
services for older people with dementia. These implications
are even greater with likely future changes in
family structure. Notable in this study was that 27.1%
of the South Asian sample, the same proportion as the
white sample, were living alone; a far greater percentage
than that found by previous researchers (7–8% in
Lowdell et al’s (2000) study).
Acknowledgment
We would like to thank a number of people for help
with this study. The Asian Elderly Group of Merton
(AEGM) and the practice managers of the Alexandra
Road Surgery, the Church Road Practice and the
Southfields Practice all offered invaluable help for
recruiting the South Asian and white samples. Members
of the AEGM and others helped with translation.
Assistant psychologists completed interviews: Kajal
Patel, Jo Steer, Anita Arora, Michelle Babbs, Jenny
Candy, Jo Crockett, Emma Haworth, Naomi Horton,
Rahat Rafiq, Hazel Rayner and Lucy Vento. Lucy
Vento and Jo Crockett also helped with coding. We
should also especially like to thank all of the older
people who were interviewed for this study. Dr Chris
Gilleard offered advice with initial design of the study.
Tables at a glance

Table 1
References
- Adamson J (2001) Awareness and understanding of dementia in African/Caribbean and South Asian families. Health and Social Care in the Community 9:391–6.
- Beliappa J (1991) Illness orDistress? Alternativemodels ofmental health. London: Confederation of Indian Organisations (UK).
- Bhugra D (2002) Ethnic factors and service utilization. Current Opinion in Psychiatry 15:201–4.
- Bhui K (1997) London’s ethnic minorities and the provision of mental health services. In: Johnson S, Ramsay R, Thornicroft G et al (eds) London’s Mental Health. London: King’s Fund, pp. 143–66.
- Bhui K and Bhugra D (2002) Mental illness in Black and Asian ethnic minorities: pathways to care and outcomes. Advances in Psychiatric Treatment 8:26–33.
- Bowes A and Dar N (2000) Family Support and Community Care: a study of South Asian older people. Edinburgh: Scottish Executive Research Unit.
- Chaudhry S and Au A (1994) The usage of the mental health service by the elderly from ethnic minorities. PSIGE Newsletter June 1994, 40–43.
- Dein S and Huline-Dickens S (1997) Cultural aspects of aging and psychopathology. Aging and Mental Health 1:112–20.
- Department of Health (1998) ‘They look after their own, don’t they?’: inspection of community care services for Black and minority ethnic older people. London: Department of Health.
- Department of Health (2001) National Service Framework for Older People. London: Department of Health.
- Dilworth-Anderson P and Gibson B (2002) The cultural influence of values, norms, meanings, and perceptions in understanding dementia in ethnic minorities. Alzheimer Disease and Associated Disorders: an international journal 16:S56–S63.
- Donaldson LJ (1986) Health and social status of elderly Asians: a community survey. British Medical Journal 293: 1079–82.
- Ebrahim S (1996) Ethnic elders. British Medical Journal 313:610–13.
- Goldberg D and Huxley P (1980) Mental Illness in the Community: the pathway to psychiatric care. London: Tavistock.
- Guglani S, Coleman PG and Sonuga-Barke EJ (2000) Mental health of elderly Asians in Britain: a comparison of Hindus from nuclear and extended families of differing cultural identities. International Journal of Geriatric Psychiatry 15:1046–53.
- Hanson EW, Creswell JW, Clark VL, Petska KS and Creswell JD (2005) Mixed methods research designs in counseling psychology. Journal of Counseling Psychology 52:224–35.
- Hinton L (2002) Improving care for ethnic minority elderly and their family caregivers across the spectrum of dementia severity. Alzheimer Disease and Associated Disorders: an international journal 16:S50–S55.
- Krippendorff K (1981) Content Analysis: an introduction to its methodology. New York: Sage.
- Lampley-Dallas VT (2002) Research issues for minority dementia patients and their caregivers: what are the gaps in our knowledge base? Alzheimer Disease and Associated Disorders: an international journal 16:S46–S49.
- Lowdell C, Evandrou M, Bardsley M, Morgan D and Soljak M (2000) Health of Ethnic Minority Elders in London: respecting diversity. London: The Health of Londoners Project.
- Mays N and Pope C (2000) Qualitative research in health care. Assessing quality in qualitative research. British Medical Journal 320:50–2.
- National Institute for Clinical Excellence (2001) Guidance on the Use of Donepezil, Rivastigmine and Galantamine for the Treatment of Alzheimer’s Disease. London: National Institute for Clinical Excellence.
- Rait G and Burns A (1997) Appreciating background and culture: the South Asian elderly and mental health. International Journal of Geriatric Psychiatry 12:973–7.
- Rait G, Burns A and Chew C (1996) Age, ethnicity, and mental illness: a triple whammy. British Medical Journal 313:1347–8.
- Rait G, Burns A, Baldwin R, Morley M, Chew-GrahamCand St Leger AS (2000) Validating screening instruments for cognitive impairment in older South Asians in the United Kingdom. International Journal of Geriatric Psychiatry 15:54–62.
- Seabrooke V and Milne A (2004) Culture and Care in Dementia: a study of the Asian community in North West Kent. London: Alzheimer’s and Dementia Support Services.
- Smith JA (1995) Semi-structured interviewing and qualitative analysis. In: Smith JA, Harre R and Van Langerhove L (eds) Rethinking Methods in Psychology. London: Sage.
- Smith JA (1996a) Beyond the divide between cognition and discourse: using interpretative phenomenological analysis in health psychology. Psychology and Health 11:261–71.
- Smith JA (1996b) Evolving issues in qualitative psychology. In: Richardson J (ed.) Handbook of Qualitative Research Methods for Psychology – the social sciences. Leicester: British Psychological Society.