- (2011) Volume 12, Issue 5
Vyacheslav Ivanovich Egorov1, Nina Ivanovna Yashina1, Tatyana Valentinovna Zhurenkova1, Maria Vladimirovna Petukhova1, Nataliya Sergeyevna Starostina1, Svetlana Alekseyevna Zarinskaya2, Kristina Anatolyevna Dmitriyeva2, Tatyana Valentinovna Shevchenko1, Roman Valeryevich Petrov1
1Vishnevsky Institute of Surgery; 2Department of Operative Surgery and Topographic Anatomy, Russia State University of Medicine. Moscow, Russia
Received March 16th, 2011 - Accepted July 24th, 2011
Context Knowing the collaterals is essential for a spleen-preserving distal pancreatectomy with resection of the splenic vessels. Objective To ascertain the sources of the blood supply to the spleen after a spleen-preserving distal pancreatectomy with resection of the splenic vessels. Methods Perfusion of the cadaveric left gastric and right gastroepiploic arteries with methylene blue after occlusion of all the arteries except the short gastric arteries (n=10). Intraoperative color Doppler ultrasound was used for the evaluation of the hilar arterial blood flow at distal pancreatectomy (n=23) after 1) clamping of the splenic artery alone, 2) clamping of the splenic and left gastroepiploic arteries and 3) clamping of the splenic and short gastric arteries. CT angiography of the gastric and splenic vessels before and after a spleen-preserving distal pancreatectomy (n=10). Results Perfusion of the cadaveric arteries revealed no effective direct or indirect (through the submucous gastric arterial network) communication between the left gastric and the branches of the short gastric arteries. In no case did intraoperative color Doppler ultrasound detect any hilar arterial blood flow after the clamping of the splenic and left gastroepiploic arteries. The clamping of the short gastric arteries did not change the flow parameters. In none of the cases did a post-spleen-preserving distal pancreatectomy with resection of the splenic vessels CT angiography delineate the short gastric vessels supplying the spleen. In all cases, the gastroepiploic arcade was the main arterial pathway feeding the spleen. Conclusion Experimental, intra- and postoperative instrumental investigations did not show the short gastric arteries to be engaged in the blood supply to the spleen after a spleen-preserving distal pancreatectomy with resection of the splenic vessels. In all cases, the left gastroepiploic artery was the main collateral vessel.
Angiography; Carcinoma; Pancreatectomy; Gastroepiploic Artery; Pancreatic Neoplasms; Pancreatitis; Spleen /blood supply; Splenic Artery; Tomography, Spiral Computed
It is general practice to remove the spleen at a distal pancreatectomy. Basically, this is done for pancreatic malignancy on principle and for intraoperative splenic parenchymal or vascular injury, and occasionally for technical considerations, with the aim of facilitating surgery and reducing the duration of the surgery [1, 2, 3, 4, 5]. Recently reported studies, confirming such detrimental splenectomy sequelae as an increased number of intra-abdominal abscesses [5, 6, 7, 8], a threat of overwhelming sepsis [9, 10, 11, 12, 13, 14, 15, 16, 17] in the aftermath of the procedure, compromised antitumor immunity [4, 18, 19, 20, 21] and a higher risk of diabetes mellitus [22, 23], have awakened interest in spleen-preserving surgery. An important aspect is that even though post-splenectomy sepsis occurs rarely, it is associated with a mortality rate of up to 50% and cannot be prevented by splenic slice autotransplantation. [13, 14, 15, 22, 24].
In 1943, Mallet-Guy and Vachon [25] were the first to give an account of a spleen-preserving distal pancreatectomy with splenic vessel conservation. Since then, many more authors have described the technique of a spleen-preserving distal pancreatectomy, indicating the painstaking exposure and conservation of the splenic vessels [26, 27, 28].
Sutherland et al. in 1980 [29] and Warshaw in 1988 [30] reported the technique of a spleen-preserving distal pancreatectomy with resection of the splenic vessels. They attributed the fact that the spleen retained its vital capacity to the reverse blood flow in the short gastric arteries.
Based on his experience, Romero-Torres suggested that the main arterial collateral feeding the spleen after a spleen-preserving distal pancreatectomy with resection of the splenic vessels is the left gastroepiploic artery, but his arguments were considered insufficient [31].
Our investigation was geared to ascertaining the pathways of the collateral blood supply after resection of the splenic vessels at distal pancreatectomy.
We applied the terms Michels had used for the arterial system of the spleen in his study of 200 cadavers which, to date, has remained the most comprehensive and elaborate study [32]. To avoid interpretation discrepancies, we deemed it wise to cite the author’s word for word description of the splenic artery and its branches (Figure 1) [32] in a supplement with reference to modern-day anatomical investigations [33].
Cadaveric Experiment
Experimental determination (on cadaveric organs) of the contributors to the collateral blood supply to the spleen following a spleen-preserving distal pancreatectomy with resection of the splenic vessels was carried out. The experiment was carried out in the post mortem examination unit at the Forensic Medicine Bureau at the Emergency Hospital in Scherbinka in the suburbs of Moscow, on the viscera of 20 individuals who had died from non-abdominal causes, within 24 hours of death. All the corpses had a normal (Michels type I) celiaco-mesenterial arterial anatomy.
The intent of the experiment was to evaluate the blood supply to the spleen via the short gastric arteries with the other arterial collaterals being ligated. For this purpose, in the experimental group (10 observations), the intensity of the staining of the spleen was assessed on perfusion of the left gastric artery with methylene blue. In doing so, the staining of the stomach was noted inasmuch as the gastric submucous arterial network could potentially have been one of the avenues for the collateral blood flow. We compared the results obtained with the findings of the absorption of the stain by the spleen in two control groups (5 observations each), i.e. in the groups where the stain injected into the arterial system (locked gastroepiploic arcade) was known to be obviously capable of reaching the splenic parenchyma anatomy-wise.
The exposure of the site of origin of the left gastric artery (i.e. where it arises the celiac axis) was followed by distal pancreatectomy and careful ligation of all the gastric arteries with the exception of the short gastric arteries in the 10 cases of the experimental group. Special care was given to left gastroepiploic artery identification and ligation at the very point of its origin from the splenic artery or the inferior terminal branch of the latter. The spleen and stomach were then taken out of the abdominal cavity and placed onto the backtable. The outside diameter and wall thickness of the left gastric, gastroepiploic, and short gastric arteries and their branches were measured with a micrometer (Caliber, Moscow, Russia).
The left gastric and right gastroepiploic arteries were cannulated with a PVC catheter. After the blood was washed out of the arterial bed of the stomach with saline within 3-4 minutes, it was uninterruptedly filled with methylene blue via the catheters under a constant pressure of 120 mm Hg for 20 minutes. The time required for the serous and mucous layers of the stomach and splenic parenchyma to absorb the stain was recorded. In 5 of the 10 subjects, which were seen as controls, the intensity of the splenic parenchyma staining was assessed on perfusion of the staining agent through the splenic artery and, in 5 cases, on perfusion through the right gastroepiploic artery by anastomosing directly with the left gastroepiploic artery. The staining was documented by taking photographs and obtaining imprints of the spleen section on filter paper.
For the spleen imprints, the intensity of the staining was defined as 0 when there was no staining at all, + if there were 1-3 small foci of methylene blue, ++ if multiple focuses were seen and +++ if there was pronounced diffuse staining of the surface. For the stomach, the staining of 1/3 of its surface was classified as +, staining of 2/3s as ++ and staining of the entire stomach as +++.
Intraoperative Color Doppler Ultrasound
After 23 distal pancreatectomies (6 males, 17 females; age mean±SD: 50.9±11.9 years), intraoperative evaluation of the arterial blood flow in the splenic hilum was carried out by intraoperative color Doppler ultrasound. Eight out of the 23 procedures were extended corporocaudal distal pancreatectomies for pancreatic cancer and 15 were standard distal pancreatectomies for chronic pancreatitis (n=2) and for cystic (n=9) or neuroendocrine tumors (n=4). In all cases, CT and CT angiography had shown normal (Michels type I) celiaco-mesenterial arterial architecture previous to surgery and, in three cases, the gastroepiploic arcade was not locked (there was not an immediate anastomosis between the left gastroepiploic artery and the right gastroepiploic artery). Laparotomy was performed using the L-shaped approach in all of the patients. The mean systolic velocity and blood flow volume were gauged on one of the terminal branches of the splenic artery in the vicinity of the splenic hilum distally to the site of origin of the left gastroepiploic artery. The tail and body of the pancreas were totally severed from the surrounding tissues, the gland was cut across in the region of the body or neck (as required by the extent of morbid involvement) with the splenic, short gastric and left gastroepiploic arteries being left intact. The transection of the gland precluded any chance of blood supply to the spleen through the transverse pancreatic artery, normally running within the parenchyma of the body of the pancreas and anastomosing with the arteria pancreatica magna. The measurements were made, while waiting for frozensection biopsy findings, through the splenic parenchyma with a transducer placed on its diaphragmatic surface and beamed along its longitudinal axis: 1) after clamping the splenic artery alone, 2) clamping the splenic and left gastroepiploic arteries and 3) clamping the splenic and short gastric arteries. Subsequent to declamping the left gastroepiploic artery and short gastric arteries, evaluation was carried out again with a clamp across the splenic artery, the short gastric arteries and the left gastroepiploic artery which were clamped in succession. The spleen was recognized as viable when its color and hilar arterial blood flow remained normal, as determined by intraoperative color Doppler ultrasound. The span of evaluation was 5 min from the clamping of the next artery in turn.
CT Angiography
Both prior and 10 to 30 days subsequent to the spleenpreserving distal pancreatectomy with resection of the splenic vessels, CT and CT angiography of the celiacomesenterial arterial system with 3D reconstruction were undertaken in 10 of these 23 patients (1 male, 9 females; age mean±SD: 52.2±8.9 years) with the aid of 64- or 256-MDCT scanners (Brillians-64® and Brillians iCT®, Philips, Cleveland, OH, USA) in order to reach a diagnosis, evaluate tumor resectability, detect possible complications, assess the viability of the spleen and trace the major blood supply to the spleen. All the CT angiography images were read by the radiologist and the attending surgeon.
Our institutional ethics committee approved this prospective review; our patients were not required to give any special informed consent other than standard one. The study protocol conforms to the ethical guidelines of the “World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004.
Descriptive statistics were applied: mean±SD and absolute and relative frequencies. Data were analyzed using the Wilcoxon matched-pairs test. The SPSS (version 13.0 for Windows, SPSS Inc., Chicago, IL, USA) statistical package was used for the statistical analysis. Two-tailed P values less than 0.05 were considered significant.
Cadaveric Experiment
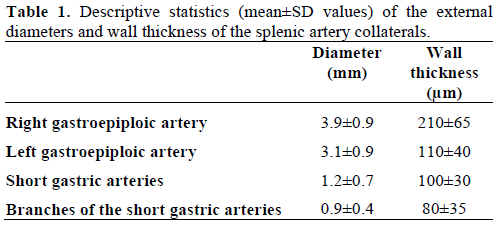
The number of short gastric arteries left intact after distal pancreatectomy varied from 3 to 7. The gastroepiploic arcade was locked (direct anastomosis between the left and right gastroepiploic arteries) in 18 of 20 cases (90.0%). The mean outer diameters and wall thickness of the splenic artery collaterals are presented in Table 1.
At perfusion of the stomach with methylene blue via the left gastric and right gastroepiploic arteries the submucosal gastric arterial network filled up in approximately one to two minutes, which then manifested itself with absorption of the stain in the entire stomach in 9 subjects and the staining of twothirds of the stomach in one (Figure 2bc and Table 2). Three to five minutes after the perfusion was induced, swelling of the gastric wall was noticed, and the stain was noticed oozing through the mucosa into the gastric lumen. In the control groups the degree of staining of the stomach was immaterial. Within 20 minutes, the splenic pulp was intensely stained in 5 controls with the perfused splenic artery (control group A; 5 cases: +++; Figure 3a) and in all 5 controls not having the left gastroepiploic artery ligated (control group B; 3 cases: +++; 2 cases: ++; Figure 3b). With all the arteries other than the short gastric arteries being ligated, there was pronounced staining of the spleen in one case (++), observed small sporadic spots of staining (+) and no staining at all (0) (Figure 3c) in 2 and 7 cases, respectively (Table 2). In 2 cases, the branches of the short gastric arteries were seen to absorb the stain but the staining of the spleen did not take place (Cases #2 and #6).Closer scrutiny of the marked spleen staining case with all the arteries except the short gastric arteries, being ligated permitted the discovery of a subsidiary arterial branch (up to 2 mm across) on the posterior gastric wall; it was found to course from the left gastric artery, anastomosing directly with one of the short gastric arteries (an accessory left gastric artery).
Figure 2. a. Contrast X-ray examination of the submucosal arterial network of a removed stomach (P: main anastomotic channels; S: subsidiary
anastomotic channels; M: mucosal arteries). b. Staining of the submucosal arterial network of a cadaveric stomach at perfusion of the left gastric and
right gastroepiploic arteries with methylene blue after all the arteries pertinent to the spleen except the short gastric arteries were ligated. The radius
(R) of the “main anastomotic channels” is approximately 0.3 mm, which corresponds to [52]. c. The staining of gastric submucous arteries took place
within 1-2 min. There was no staining of the spleen during a 20-min period.
Figure 2a was published as Figure 5 in: Barlow TE, et al. Arteries, vein and arterio-venous anastomoses in the human stomach. Surg Gynecol Obstet
1951; 93:657-7 [52]. Copyright Elsevier, 1951. Published with permission of the publisher.
Figure 3. Staining of the cadaveric spleen on perfusion with methylene blue through: a. the splenic artery (+++); b. the left gastroepiploic artery (++); and c. the left gastric and right gastroepiploic arteries after all the arteries pertinent to the spleen except the short gastric arteries were ligated (0). Right: spleen longitudinal section; left: imprint of the section surface.
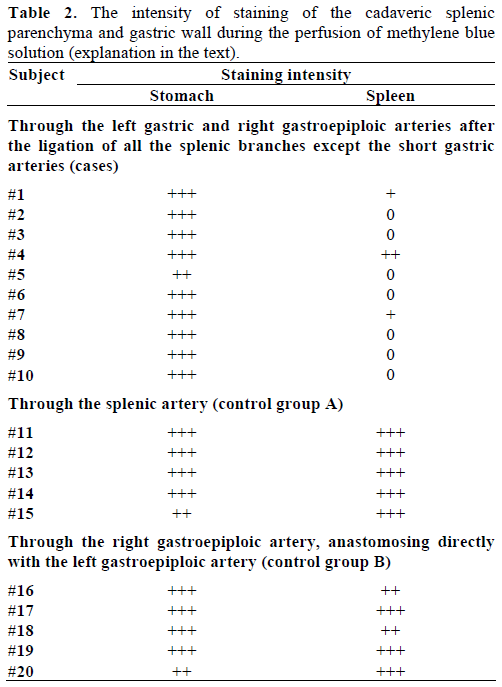
Thus, perfusion of the cadaveric gastric arteries revealed the marked staining of the spleen with the splenic or left gastroepiploic arteries being left intact. With all the arteries, except for the short gastric arteries, being ligated, no distinct staining of the splenic parenchyma (0 or +) was present in 9 out of 10 cases, that is to say, no adequate blood supply to the spleen via the gastric submucosal network or the anastomoses between the branches of the left and the short gastric arteries was detected. The one exception (Case #4) was a rarely encountered variant of the direct anastomosis of an accessory left gastric artery with one of the short gastric arteries.
Intraoperative Color Doppler Ultrasound
According to the changes in US findings after the above-mentioned successive clampings of the arteries supplying the spleen and stomach, the patients were divided into two groups. In Group 1 (20 cases, 87.0%), there was a direct anastomosis between the left and right gastroepiploic arteries and, in Group 2 (3 cases, 13.0%), the gastroepiploic arcade was disconnected. In Group 1, the splenic artery clamping was followed by a 1- to 3-fold fall in blood flow volume brought about by the drop in mean systolic velocity, but the spectrum of the Doppler shift corresponded to the arterial wave with a large diastolic component (Figure 4a). In all cases except one (#8, Table 3), upon the splenic artery being clamped, left gastroepiploic artery clamping, even of a collateral type, caused the arterial blood flow to cease (Figure 4b). Upon the splenic artery being clamped, clamping of the short gastric arteries before or after the left gastroepiploic artery cross-clamping did not alter the qualitative or quantitative parameters of the flow. In the case of the sole exception (#8), after the clamping of the splenic artery and the left gastroepiploic artery, hilar collateral flow was detectable but it was decreased fourfold and was accompanied by marmoreal staining of the spleen (Table 3).
Figure 4. Intraoperative color Doppler ultrasound of the splenic hilum at distal pancreatectomy in cases of a direct anastomosis between the left and right gastroepiploic arteries. a. A 3-fold fall in blood flow volume after splenic artery cross-clamping (arrow). b. Upon the splenic artery being clamped the left gastroepiploic artery clamping (arrow) caused the arterial blood flow to cease. Upon the splenic artery being clamped, the clamping of the short gastric arteries before or after left gastroepiploic artery cross-clamping did not alter the flow parameters.
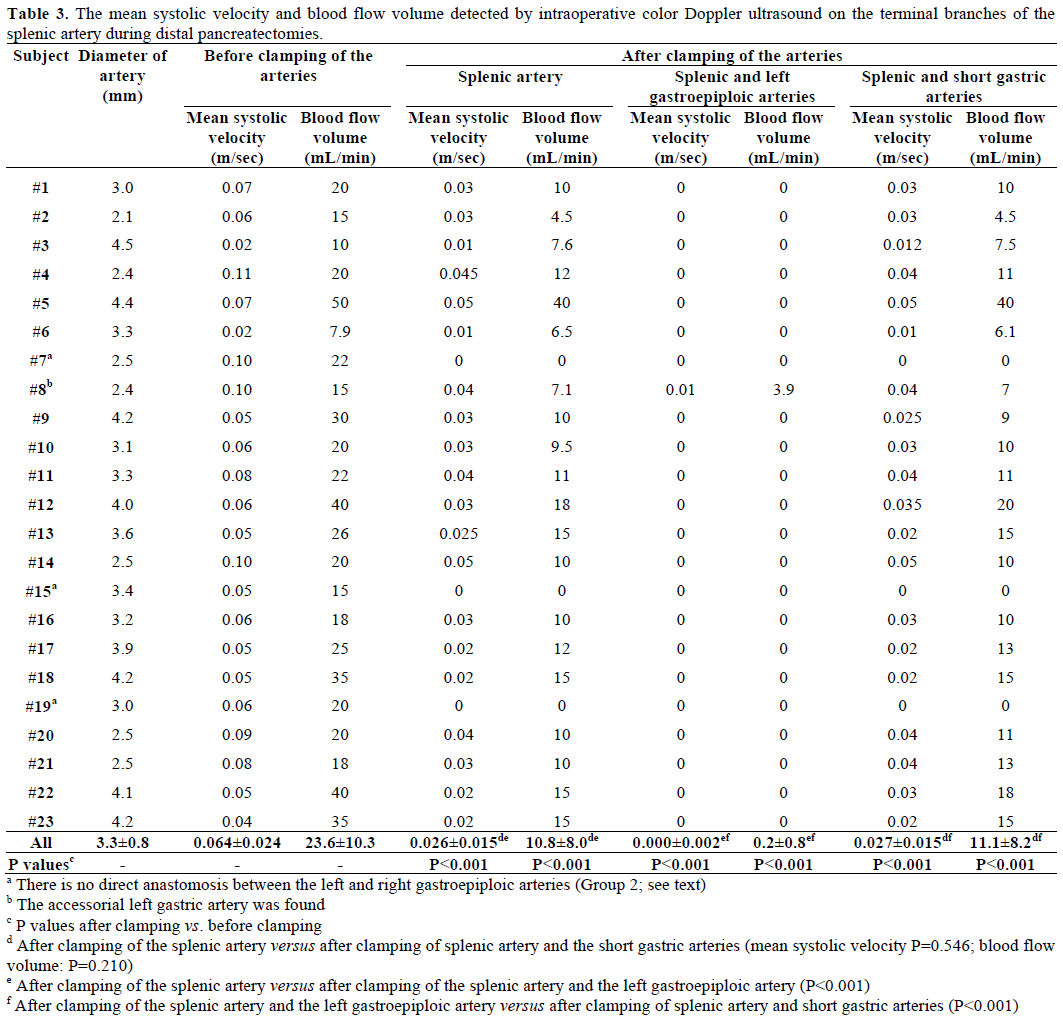
In Group 2 (3 cases, 13%), the splenic hilar arterial blood flow disappeared after the clamping of the splenic artery (Table 3), and it was unaffected by the subsequent clamping of the short gastric and leftgastroepiploic arteries, irrespective of the order in which they were clamped (Figure 5).
Figure 5. Intraoperative color Doppler ultrasound of the splenic hilum at distal pancreatectomy in cases of an interrupted gastroepiploic arcade. The arterial blood flow disappeared after splenic artery cross-clamping. It was unaffected by the subsequent clamping of the left-gastroepiploic artery and the short gastric arteries irrespective of the order in which they were clamped.
In the spleen-sparing cases neither US nor CT demonstrated any splenic infarctions, disturbed blood supply or impaired hematologic pattern. Thus, in none of the cases did intraoperative color Doppler ultrasound of the splenic hilar arteries at distal pancreatectomy demonstrate the short gastric arteries to be capable of providing a sufficient blood supply to the spleen after splenic and left-gastroepiploic artery clamping (Figure 6).
Figure 6. Summarized alterations in the hilar arterial blood flow
volume at distal pancreatectomy. There was a two/three-fold
decrease in the blood flow volume after splenic artery (SA) crossclamping.
The subsequent cross-clamping of the short gastric arteries
(SGA) did not influence the blood flow which discontinued after left
gastroepiploic artery (LGEA) clamping when the splenic artery was
clamped. The chart is plotted on the basis of the data from Table 3.
* All pairwise differences were significant (P<0.001) except the
clamping of the splenic artery versus the clamping of the splenic
artery and the short gastric arteries (P=0.210) (Table 3).
CT Angiography
Preceding surgery, the splenic artery was always seen on CT angiography as a thick stem with no other branches travelling to the spleen (Figures 7a and 8a). As a consequence of splenic artery resection, the whole or the bulk of its trunk were no longer available for evaluation by CT angiography after a spleenpreserving distal pancreatectomy with resection of the splenic vessels and, in all 10 cases, the gastroepiploic arcade was seen to have become the “highway” to the spleen within 7-30 days after surgery (Figures 7b, 8b, and 9). In two cases, due to technical reasons, 3D CT angiography was only carried out postoperatively but, in both cases, there were no doubts about the source of the blood supply to the spleen (Figure 9). In none of the 10 cases was any appreciable blood flow through the short gastric arteries visualized.
Figure 7. Celiaco-mesenterial anatomy in а 53-year-old man with chronic pancreatitis of the distal type. 3D CT angiography after the renal artery
images were eliminated. Vertical view. a. Before surgery: the splenic artery thick trunk with no collaterals is shown. b. Fourteen days after a spleensparing
distal pancreatectomy with resection of the splenic vessels: the spleen is fed through the gastroepiploic arcade. There are no other detectable
major arteries to feed the spleen.
D: drainage tube; GEA: gastroepiploic arcade; RGEA: right gastroepiploic artery; SA splenic artery; SAR: splenic artery remnant
Figure 8. Celiaco-mesenterial anatomy in а 59-year-old woman with a neuroendocrine tumor of the pancreatic body and tail. 3D CT angiography
after the renal artery images were eliminated. a. Before surgery: the splenic artery thick trunk with no collaterals is shown. b. Ten days after a spleensparing
distal pancreatectomy with resection of the splenic vessels: the spleen is fed through the gastroepiploic arcade. There are no other detectable
major arteries to feed the spleen. c. After surgery, vertical view: the arrow is pointing to the gastroduodenal artery, i.e., the site of origin of the
gastroepiploic arcade.
GEA: gastroepiploic arcade; LGEA: left gastroepiploic artery; SA: splenic artery
Figure 9. Celiaco-mesenterial anatomy in 57 (a.) and 51 year old females (b.) women with mucinous cystic tumors of the pancreatic body and tail. 3D CT angiography 7 and 30 days, respectively, after a spleen-sparing distal pancreatectomy with resection of the splenic vessels without the renal artery images. The only vessels feeding the spleen are the gastroepiploic arcades (arrows). There are no other detectable collaterals of value. 3D CT angiography images were not obtained before surgery.
Thus, 3D CT angiography after a spleen-preserving distal pancreatectomy with resection of the splenic vessels did not reveal any reliable blood flow via the short gastric arteries. In all cases, the dominant role of the left gastroepiploic artery serving as the main blood supply to the spleen through the gastroepiploic arcade was observed.
In 1980, Sutherland et al. from the University of Minnesota Health Sciences Center gave an account of 5 spleen-preserving corporocaudal pancreatectomies with resection of the splenic vessels in living donors for transplantation to related recipients [29]. By 1984, spleen-preserving distal pancreatectomies with resection of the splenic vessels had been performed in 35 living-related donors [34], and in 2001 111 such operations were reported to have been carried out in living-related donors [35]. According to procedure, the blood supply to the spleen during surgery was delivered by the short gastric arteries, notwithstanding the fact that it is obvious from the accompanying illustrations [36] that the left gastroepiploic artery was left untouched in all cases. In 1988, Warshaw from Massachusetts General Hospital reported 22 spleenpreserving distal pancreatectomies with resection of the splenic vessels carried out for pancreatic tumors, and acute and chronic pancreatitis [30]. By 2007, the number of such cases had grown to 74 [37] and by the beginning of 2011 to 158 [38, 39, 40].
Over the years, the spleen-preserving distal pancreatectomy with resection of the splenic vessels has received wider acceptance and a series of studies has validated its simplicity, safety and efficacy when compared to a spleen-preserving distal pancreatectomy with splenic vessel conservation or a distal pancreatectomy with splenectomy [11, 41 42, 43, 44, 45, 46, 47, 48]; some of the authors have had a higher occurrence of splenic infarctions after resection of the splenic vessels [4]. Even though some concerns have been voiced about damaged venous drainage in the context of both splenic vessels being resected, there have only been a few clinical presentations with sinistral portal hypertension [39, 40, 49, 50].
In all the papers addressing the interventions being discussed here, the authors have emphasized the critical role of the short gastric arteries in the blood supply to the spleen after splenic vessel excision but have also recommended preserving the left gastroepiploic artery [30, 37, 38, 39]. To be aware of these subtleties is of great concern considering the favorable prognosis in essentially all the patients undergoing such interventions and, keeping in mind that further surgery is probable when the collaterals pertinent to the spleen are damaged. Among these interventions are fundoplication, gastric, duodenal, subtotal and total pancreatic head resections, right and transverse colectomies and other gastroepiploic arcadesacrificing procedures (interestingly, to save the left gastroepiploic artery at the pancreatic head, resection and total pancreatectomy are feasible, if the operation is not undertaken as a sequel to a Whipple procedure but as a continuation of a pylorus-sparing segmental duodenectomy [51, 52]).
Taking the fact that the short gastric arteries are the main spleen supplying collaterals after a spleenpreserving distal pancreatectomy with resection of the splenic vessels as a basis, it would be of value to know which arteries supply blood to the short gastric arteries. What would be the result of the ligation of the left gastroepiploic artery in addition to that of the splenic artery? Would the volume of the blood conveyed through these vessels suffice in order to sustain the vital capacity of such a sizable parenchymal organ as the spleen?
Michels answered these questions in his study[32]; the reverse blood flow through the short gastric arteries towards the splenic hilus is theoretically possible by one of three variants: 1) the anastomoses of the left gastric artery branches and one or several short gastric artery branches on the anterior or posterior gastric wall, 2) the anastomoses of the branches of the left inferior diaphragmatic artery with one or several short gastric artery branches on the anterior or posterior gastric wall and 3) transit via the gastric submucosal arterial network.
It is well to bear in mind that, anatomically speaking, variants 1 and 2 are not found consistently (from human to human) and, even when they are found they involve vessels less than 1 mm in diameter. The submucosal arterial network vessels range in diameter from 0.2 to 0.6 mm (Figure 2a) [53, 54].
Romero-Torres speculated that the left gastroepiploic artery was the principal spleen feeding collateral subsequent to excision of the splenic vessels [31]. And yet, the arguments he brought forward were only considered mere conjecture. His anatomic studies yielded evidence in favor of Michels’ findings regarding left gastroepiploic artery topography [31]. At the same time, from 1981 to 1989, Romero-Torres reported 75 cases of splenic salvage after surgery for portal azygos disconnection which was introduced by him for portal hypertension [55, 56]. That intervention included the ligation of the splenic and the left gastric arteries with the transection of all the short gastric arteries. The spleen survived after the splenic and short gastric arteries were ligated, which would dramatically have demonstrated the role of the left gastroepiploic artery as the chief spleen-supplying collateral in this setting if there had not been an intact transverse pancreatic artery normally appearing as a robust trunk going to the hilum of the spleen through the arteria pancreatica magna [33, 57].
Given that the left gastroepiploic artery is not easily identifiable either intraoperatively (Figure 10) or on section [32], and is usually conserved in a spleenpreserving distal pancreatectomy with resection of the splenic vessels, this alone makes it unreasonable to credit the short gastric arteries with being the primary spleen-supplying collaterals. Anticipating that the short gastric arteries should be the primary spleen-supplying collaterals is, to a large degree, intrinsically conceptual since none of the studies has shown the direction of the blood flow in these vessels following splenic artery resection. We were prompted into carrying out our investigation by the supposition that such a large parenchymal organ as the spleen could be amply supplied with blood through collaterals less than 1 mm in diameter.
Figure 10. View of the operating field after a spleen-sparing distal
pancreatectomy with resection of the splenic vessels. The left
gastroepiploic artery is of the same diameter as the terminal portion
of the splenic artery (arrow).
LGEA: left gastroepiploic artery; S: stomach; SA: splenic artery’s
terminal portion; Spl: spleen
Anatomic studies alone fail to enable one to appreciate the rate and specifics of the function of the available spleen-supplying arterial collaterals after resection of the splenic vessels. Not having a ready tool at hand for sensing the direction of the blood flow in the arteries of interest during the operative procedure, we resorted to other means. Our experimental procedure is simple and easy to replicate. While post-mortem perfusion experiments may not accurately portray the channels open in vivo due to the fact that all the vascular anastomoses are open, and the pressure within the system is fixed and above normal; such a setting is, in a sense, more revealing and representative than it would be in vivo. The anastomoses between the branches of the inferior diaphragmatic artery and those of the short gastric arteries are not truly representative since they would be severed as a result of the excision of the organs.
Surgeon-performed color duplex evaluation of the splenic hilum arteries [58] and identification of the left gastroepiploic artery are comparatively easy to carry out. A “sine qua non” for the accurate estimation of the hilar blood flow quantitative parameters was adherence to a uniform method of measurement using the same arterial segment at the same insonation angle, which was comfortably obtainable through the L-shaped approach which is applied in extended corporocaudal resections for pancreatic cancer. Duplex scanning was employed to acquire an adequate postoperative assessment of the arterial blood flow within the splenic parenchyma, but we feel that comparing these data with the presurgical data is complicated [40, 59]. 3D CT angiography was used as an accurate modality for displaying the main arteries both pre- and postoperatively [60].
The spleen maintaining its arterial blood supply is the case when the gastroepiploic arcade is unlocked, except that, owing to collaterals having a tiny diameter, the compensatory dilation of small arteries and veins of the the gastric body and fundus takes place, thus increasing the risk of gastric bleeding as occurred in one of our earlier cases (Figure 11).
Figure 11. Celiaco-mesenterial arterial anatomy in a 34-year-old man 9 years after a spleen-preserving distal pancreatectomy with resection of the splenic vessels for a neuroendocrine carcinoma. a. 3D CT angiography (after the renal artery images were eliminated) showing the collateral blood flow through the inferior branch of the left gastric artery (arrowhead) anastomosing with the short gastric arteries and/or the branches of the left gastroepiploic artery (thin arrow) with the gastroepiploic arcade being broken (thick arrow). b. and c. CT: arterial phase. Delineated elongation, coiling, tortuousness and dilation of the perigastric arteries and veins (arrows) are seen against the background of a thickened gastric wall and splenomegaly. S: spleen; SAR: splenic artery remnant
The evidence we acquired is suggestive of the left gastroepiploic artery being the key spleen-supplying collateral, communicating with the right gastroepiploic artery completely in the majority of cases but more rarely with the subsidiary left gastric artery, thus forming the gastro-epiploic arcade. In most spleenpreserving distal pancreatectomies with resection of the splenic vessels with a functioning gastroepiploic arcade, the short gastric arteries had no role in delivering blood to the spleen. And what is worse, owing to the well-evolved arterial network of the splenic hilus, this scenario is open to “stealing” from the arterial flow to the spleen, if the direction of the blood flow through the short gastric arteries remains the same as it was prior to splenic artery excision. This is to be expected in view of the fact that postoperative CT angiography delineates a strong arterial blood flow through the left gastroepiploic artery; the vigorous blood flow through this artery would preset a regular blood flow route in the short gastric arteries (towards the stomach), and consequently, “steal” from the spleen. When this is the case, the transection of the short gastric arteries in a spleen-preserving distal pancreatectomy with resection of the splenic vessels is bound to improve the blood supply to the spleen, but to do that is technically rather troublesome owing to an intimate intermingling of the short gastric arteries and veins. Cutting the short gastric veins across could severely disturb the splenic outflow.
Therefore, when performing a distal pancreatectomy with resection of the splenic vessels, a surgeon should not rely on the short gastric arteries if he strives for spleen salvage. It is possible but it is contingent on small diameter communication or on rarely encountered aberrant vessels. In the case of spleenpreserving distal pancreatectomy with resection of the splenic vessels the left gastroepiploic artery, ordinarily (around 90% of the cases [32]) anastomosing directly with the right gastroepiploic artery or (far less commonly) with the accessory left gastric artery, is the crucial spleen-supplying collateral. It is precisely these vessels which merit conservation.
Unwarranted reliance on the short gastric arteries with the splenic artery being transected more distally to the sites of origin of the left gastroepiploic artery will result in splenic infarctions or a primary splenectomy or a splenectomy at a later date [41, 61, 62]. Even considering “… the fact that there is no evidence that the spleen does not survive or how often it does not survive if the left gastroepiploic artery is taken, inadvertently or by ignorance; …” as well as that sometimes “… the splenic circulation is demonstrably diminished at the end of the operation but rebounds to essentially normal levels within a short time (days?), probably due to opening or enlargement of collaterals from either system …” (Warshaw, personal communication), we reason that there are few surgeons, if any, who might ever risk sparing a spleen of dubious viability in the expectation that some mysterious undetectable collaterals would start functioning in the indefinite future. It is much safer to acquire intraoperative confirmation the viability of the spleen and we obtained such confirmation only with the gastroepiploic arcade being left intact.
From our point of view, the data obtained to date can be looked upon as being a matter of both theoretical and practical interest to surgeons, not only providing an incentive for additional studies but also fostering awareness in deciding upon the best surgical option.
In a few instances, the left gastroepiploic artery originated from the interior of the spleen (a fact to be remembered) and it may be coiled and superimposed on the splenic terminal branches. In this anatomical situation, the left gastroepiploic artery can lie on the surface of the inferior or superior terminal branch of the splenic artery which makes its identification difficult.
In our opinion, all Michels’ words are irrevocable and fully deserve to be remembered for the sake of reliability and their persuasiveness. Therefore, we would like to report Michels’ findings in his words [32].
Splenic Artery
There are two types of splenic arteries, the magistral (30%) and the distributed (70%). In its course to the spleen, the splenic artery may be divided into four segments. Segment #1: suprapancreatic segment. It is very short (1-3 cm) and usually lies above the pancreas. In order of frequency, this segment gives rise to: a) the left inferior phrenic artery b) the dorsal pancreatic artery (arteria pancreatica dorsalis), c) the superior polar artery, d) the cardioesophageal artery (ramus esophagogastricus posterior ascendens), e) an accessory gastric or hepatic artery and f) the inferior mesenteric artery. Segment #2: pancreatic segment. This segment gives rise to numerous pancreatic branches. It is frequently the site of origin of a long superior polar artery. When the left gastroepiploic artery is branches off from this segment, the resultant divisional pattern of the splenic artery is usually of a distributed type. A characteristic regional branch is the large pancreatic artery (arteria pancreatica magna) which enters the pancreas at the dorsal superior border, then descends to anastomose to the left with the caudal pancreatic artery and to the right with the transverse pancreatic artery. The cardioesophageal branch (ramus esophagogastricus posterior ascendens), one or more short gastric (fundic) branches or an accessory left gastric artery may arise from this segment. Segment #3: prepancreatic segment. This portion of the splenic artery usually branches off from the upper border of the pancreas to run obliquely along its anterior surface. In the majority of instances (80%), the main splenic trunk divides into the arteria terminalis superior (ramus lienogastricus) and the arteria terminalis inferior (ramus lienogastroepiploicus). The distance of the terminal division point from the spleen is relatively constant (from 2 to 6 cm), usually 3-5 cm. Other linealbranches of the spleen may arise 1 to 12 cm from the hilus (i.e. anywhere from the celiac axis to the hilus of the spleen). Other patterns comprise cases having a third terminal artery, cases having only an arteria terminalis superior, and cases where terminal division of the trunk is atypical. The left gastroepiploic artery arises over the tail of the pancreas, either from the trunk or from the inferior terminal. One or more polar arteries arise from the splenic trunk or its primary branches. Short gastric and omental rami are frequently given off by the splenic terminals. The caudal pancreatic artery distributed to the tail of the pancreas may arise from the splenic trunk from one of its terminal divisions or from the left gastroepiploic artery. Segment #4: the prehilar segment is the portion of the splenic artery situated between the tail of the pancreas and the hilus of the spleen. Its lineal branching into the superior and the inferior terminals occurs in this region in 30% of cases. In the majority of cases, this segment is occupied by penultimate and ultimate lineal branches (from 7 to 35) which usually arise at a right angle to the stem.
Left Gastroepiploic Artery
In origin, size, length, constituent branches, number and mode of vascular connections with the stomach, spleen and pancreas, the left gastroepiploic artery is such a markedly varied artery that a uniform concept of it cannot be formed. In about three-quarters of the cases (72%), it arises from the splenic trunk several centimeters (ranging from 1 to 4 cm) proximal to its division into two or three terminal branches (Figure 1). Next in frequency (22%) is its origin from the inferior splenic terminal or from one of its lineal branches (authors’ note: Ndoye et al. described such an origin of the left gastroepiploic artery in 68% of cases [33]). Least frequent is its origin from the middle of the splenic trunk (6-7 cm from the spleen) or from a superior terminal. The artery may be replaced by 2 to 3 vessels, the main vessel arising from the splenic artery or its branches, the other or others, usually smaller, from a polar artery given off by the splenic artery to the spleen. In a few instances, the left gastroepiploic artery originates from the interior of the spleen, a fact to be remembered because, in this anatomical situation, the left gastroepiploic artery can be applied to the surface of the inferior or superior terminal branch of the splenic artery which makes its identification difficult.
The left gastroepiploic artery reaches the stomach below the fundus by means of the phrenicopancreaticolienal ligament and descends along the left side of the greater curvature in the anterior layer of the great omentum. The left gastroepiploic artery, in most instances (90%), effects a direct anastomosis with the right gastroepiploic artery, constituting the arcus arteriosus ventriculi inferior of Hyrtl. In many instances (10%), the left gastroepiploic artery does not anastomose with the right gastroepiploic artery at all, while, in other cases, anastomosis is very weak.
Branches of the left gastroepiploic artery include: 1) fine and stout fundic branches (from 2 to 4), 2) a variable number of short ascending gastric branches to the anterior and the posterior surfaces of the stomach, 3) short and long descending or omental branches, some of which communicate with similar branches from the right gastroepiploic artery and with branches from the left colic artery, 4) pancreatic rami to the tail of the pancreas; one of these is usually large and is known as the arteria caudae pancreatic and the others, (2 or 3) are small and 5) inferior polar arteries to the spleen, which vary in number (from 1 to 5), size and length (from 3 to 8 cm).
The left gastroepiploic artery may arise from an inferior polar artery, the caliber of which is larger than the left gastroepiploic artery itself. The same may be said of its occasional origin from a branch of the inferior splenic terminal. As it approaches the spleen, the left gastroepiploic artery may give rise to an irregular contoured arch from which many small lineal branches arise, these in turn giving off short gastric arteries. Collectively considered, the blood volume coming to the spleen through the inferior splenic polar branches (from 2 to 4) of the left gastroepiploic artery may approach that reaching the spleen through its primary terminal lineal branches. The main splenic blood route, in such cases, is through the left gastroepiploic artery, just as, in certain instances, a main route may be through an enlarged transverse pancreatic artery arising from the superior mesenteric artery.
Similar to its parent trunk, the left gastroepiploic artery is frequently tortuous and looped, but rarely coiled. Its relationship to the tail of the pancreas varies in accordance with its site, mode of origin from the splenic artery and with the volumetric proportions of the pancreas, the artery frequently coursing the pancreaticolienal ligament between the tail of the pancreas and the spleen. Tortuosity may extend to the inferior polar arteries given off by the left gastroepiploic artery, the latter and its branches lying in loops and spirals on the gastric surface of the spleen, making the identification of the left gastroepiploic artery somewhat confusing and difficult. In such instances, the exact origin of the short gastric arteries cannot be ascertained without extensive dissection and repeated manipulation. An important branch of the left gastroepiploic artery is the left epiploic artery (arteria epiploica sinistra) which forms a left limb of the arcus epiploicus magnus of Barkow, the right limb being formed by the right epiploic (arteria epiploica dextra) from the right gastroepiploic artery or transverse pancreatic artery.
The Short Gastric or Fundic Branches of the Splenic Artery (Arteriae Gastricae Breves)
Short gastric arteries vary in number (from 2 to 10), size, site of origin and mode of distribution, some of them reaching the esophagus. Collectively considered, they comprise an upper, a middle, and a lower group, the latter being the longest. The shorter ones arise from the splenic trunk, from the superior splenic terminal or its branches, or from a superior polar artery; the longer ones arise from the inferior splenic terminal and from the left gastroepiploic artery or its branches. In some instances, one or two may arise from the interior of the spleen unaccompanied by a vein. Leaving the phrenicolienal ligament, the short gastric arteries pass into the gastrolienal ligament to reach the fundus and the cardio-esophageal end of the stomach, where they ramify over the anterior and the posterior surfaces, and anastomose with branches given off by the left gastric artery, left gastroepiploic artery and the left inferior phrenic artery. When an aberrant left hepatic artery stems from the left gastric artery or an accessory left gastric artery stems from the left hepatic artery, the cardioesophageal branches of the respective vessels communicate with the short gastric arteries which have reached the esophageal region.
The authors would like to express appreciation to Ingrid Evaldovna Valeniks for her translation
The authors have no potential conflicts of interest