Research Article - (2017) Volume 1, Issue 1
William E. Feeman*
Bowling Green Study, Bowling Green, Ohio, USA
*Corresponding Author:
William E. Feeman, Jr, MD
Bowling Green Study, Bowling Green
Ohio, USA
Tel: (419) 352-4665
E-mail: BGSCRF43402@yahoo.com
Received Date: November 14, 2017; Accepted Date: November 24, 2017; Published Date: December 01, 2017
Citation: Feeman WE (2017) Statin Therapy in a 102 Year Old Survivor of Myocardial Infarction Statin Therapy in Extreme Old Age. Cardiovasc Investig. Vol.1 No.1:3
This manuscript involves a case report, unique in the world, of an elderly female patient who survived an acute myocardial infarction at age 75 and subsequently underwent coronary artery bypass surgery. Nothing was done about the atherothrombotic disease (ATD) risk factors by her attending physician. When her chest pains returned some four years later, she came to the author’s clinic for preventive treatment. After determination of the patient’s ATD risk factors, appropriate therapy was initiated with statins, low dose aspirin, and a calcium channel blocker (for the chest pain). The patient is still alive at age 102 and ½ years, living at home, with no evidence of dementia, on the noted therapeutic regimen and no other intervention. At age 101 and ½ years, the patient developed a mild case of congestive heart failure, which was treated symptomatically. She continues to do well. This case report shows what is possible in the treatment of ATD in the very old patient population.
Keywords
Statin therapy; Atherothrombotic disease; Dyslipidemia
Introduction
The anti-Cholesterol/anti-statin Crusade is still alive and well on the internet, specifically on Medscape/theheart.org. The main concerns of the internet bloggers, some of whom are physicians, are the safety of statin therapy, the use of statin therapy in the treatment of dyslipidemia, and its use in the elderly [1-3]. These issues have recently been addressed by the National Lipid Association, but have been argued in the literature for many years, with most authors, at least since 1990, concluding that dyslipidemia in the elderly should be treated [4-15]. In support of these positions, the author wishes to report a case which he believes may be unique: continued statin therapy in a 75 year old survivor of an acute myocardial infarction (AMI) for the following 27 years. The patient is now 102 and ½ years old and, following an initial period of post-infarction angina and recurrent syncopal episodes, has done well since on statin/calcium blocker/aspirin therapy, living at home without subsequent cardiac events or interventions.
Materials and Methods
The patient to be discussed, with her permission, sustained an acute AMI in 1990 at the age of 75 years. Her presenting symptoms were chest pain radiating down both arms and she had serial EKG’s showing initial ST segment depression, which improved over time. Her CPK levels peaked at 1112 U/L and then resolved; her CKMB, at 9 mg/ml with subsequent resolution. Coronary angiography showed severe three vessel disease with a 70% stenosis of the LAD diagonal branch and an 80% stenosis of the LAD distal to the second diagonal branch. The left circumflex artery had a tapering 80% stenosis and the right coronary artery had a proximal 99% stenosis. The patient subsequently underwent coronary artery bypass surgery of the stenoses.
Results
The author first attended the patient, who had been seeing another physician, in the spring of 1994, at which time the patient related that she had done well until approximately two months previously, at which time she began to have chest pain again. The pain was relieved by nitroglycerine. The pain had recurred two days prior to her initial visit, this time presenting at the base of her neck and moving into her throat, again relieved by nitroglycerine. Thereafter her symptoms resolved. The author’s initial treatment consisted of reducing her aspirin dose to 81 mg daily, adding fish oil and amlodipine (for angina). Nitroglycerine was added in the form of a patch and the nitroglycerine spray was continued.
The author also ordered a lipid profile and when that was abnormal, repeated it for verification. She had no other atherothrombotic disease (ATD) risk factors. She had never smoked cigarettes, though her husband had smoked for many years, eventually quitting some years prior to her AMI. She was not diabetic. Her body mass index was 24. Her blood pressure was 138/76 mmHg. A sample of her serial lipid profiles are given in the Table 1. Her two hour postprandial blood sugar was 100 mg/dl.
Table 1 Sampling of patient’s initial and on-treatment lipids.
| Date | CT | LDL-Cholesterol | HDL- Cholesterol | TG | CRF | SBP |
|---|---|---|---|---|---|---|
| 05-Aug-94 | 194 | 130 | 39 | 125 | 0.7 | 138 |
| 21-Feb-95 | 193 | 119 | 48 | 132 | 0.6 | 128 |
| 21-Oct-96 | 157 | 79 | 54 | 119 | 0.32 | 122 |
| 17-Aug-98 | 157 | 82 | 49 | 131 | 0.4 | 122 |
| 21-May-01 | 173 | 91 | 53 | 147 | 0.42 | 124 |
| 17-May-05 | 232 | 141 | 59 | 158 | 0.58 | 128 |
| 17-Nov-05 | 118 | 39 | 60 | 94 | -0.54 | 124 |
| 13-Mar-08 | 145 | 64 | 59 | 111 | 0.08 | 128 |
| 13-Sep-11 | 151 | 76 | 60 | 74 | 0.21 | 124 |
| 07-Dec-15 | 143 | 51 | 74 | 89 | -0.45 | 122 |
Note: CT means total cholesterol; LDL means low-density lipoprotein; HDL means high-density lipoprotein; TG means triglycerides; CRF means Cholesterol Retention Fraction ([LDL-HDL]/LDL); SBP means systolic blood pressure. All lipid values are given in terms of mg/dl
In 1999 at the author’s local hospital laboratory, the methodology for measuring HDL-cholesterol was changed from the precipitation method to the enzymatic method. These differing methodologies do not give the same results. The HDL-cholesterol level obtained using the enzymatic method is on the order to 10 mg/dl (0.25 mmoles/L) higher than the equivalent value obtained when the precipitation method is used. In turn, the calculated LDL-cholesterol will be on the order of 10 mg/dl (0.25 mmoles/L) lower than the equivalent LDL-cholesterol calculated had the precipitation method of HDL-cholesterol measurement been used. This change is not trivial, as borne out by what happened to one of the author’s patients. For this reason, all HDL-cholesterol measurements since 1999 have been converted to their precipitation method equivalents using a formula supplied to the author by the auto-analyzer manufacturer: HDL-cholesterol (precipitation)= [HDL-cholesterol (enzymatic) minus 12]/0.93. This keeps all the lipids in the same system [16].
The author uses, as his preferred lipid predictor, the Cholesterol Retention Fraction (CRF, or [LDL-HLD]/LDL), which is abnormal at any age at 0.70 and in people after their sixth decade of life at 0.60-0.69. (These values are based on the precipitation method of HDL-cholesterol measurement; if the enzymatic method of HDL-cholesterol measurement is used, then the values are 0.60 and 0.50-0.59 respectively). The author combines the CRF with systolic blood pressure (SBP) into an ATD predictive graph, with the CRF on the ordinate and SBP on the abscissa. A threshold line has been generated, above which lie the CRF-SBP plots of the majority (83%, or 500/602 patients) of the author’s ATD patients. Once cigarette smokers are excluded, only 7% (44/601) of all of the authors ATD patients with outpatient data are not predicted by a CRF-SBP plot above the threshold line and/or cigarette smoking status, and such patients are quite old when their ATD events occur (mid- to late-eighth decade of life, on average, with death not occurring, on average, for an additional 10-15 years. The author therefore designates the area below the threshold line, in the absence of any history of cigarette smoking, to be an area of minimal ATD risk, and it is his goal to lower the CRF-SBP plots of his patients below the threshold line (Figures 1A and 1B).
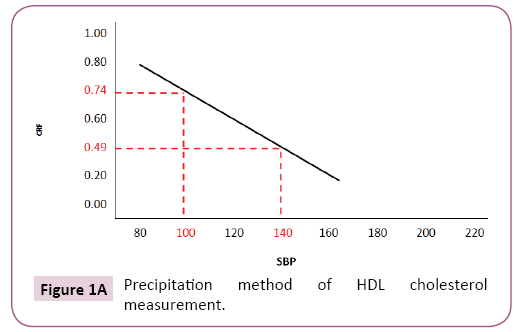
Figure 1A: Precipitation method of HDL cholesterol measurement.
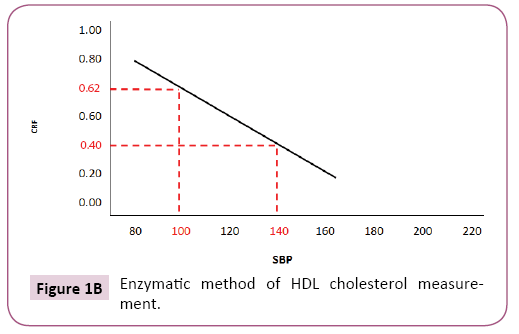
Figure 1B: Enzymatic method of HDL cholesterol measurement.
In a primary prevention scenario, the threshold line CRF-SBP coordinates are (0.74, 100) and (0.49, 140) when the precipitation method of high-density lipoprotein (HDL) cholesterol is utilized, but (0.62, 100) and (0.40, 140) if the enzymatic method of HDLcholesterol measurement is used. This graph covers all forms of clinical ATD. If, however, only coronary artery disease is targeted, then SBP can be dispensed with and the low-density lipoprotein (LDL) can be stratified by CRF. The basis of excluding SBP can be found in the Program on the Surgical Control of the Hyperlipidemias (POSCH), in which marked rates of plaque stabilization/regression were observed with marked lipid modification in the face of extremely high SBP. (POSCH was not structured to control SBP) [17,18].
The patient in question, however, was in a secondary prevention scenario, having had her acute ATD event in 1990. In secondary prevention scenarios the author has shown that in eight published angiographic regression trials, maximum plaque stabilization/ regression (93% of cases) occurs at a LDL-cholesterol goal of 79 mg/dl or less [19]. (These values hold for the precipitation method of HDL-cholesterol measurement; if the enzymatic method of HLD-cholesterol measurement is used, then the LDLcholesterol goal is 69 mg/dl or less). The patient met all of the goals of therapy, at least most of the time, as can be observed in the Table 1. After confirming the dyslipidemia, treatment of her dyslipidemia was initiated with lovastatin 10 mg daily. Her initial clinical course was unsettled. She had intermittent angina pains, but these eventually resolved and she stopped her nitroglycerine patch and eventually stopped her nitroglycerine spray as well. She did have one hospitalization in 2009 for chest pain, not thought to be cardiac in origin, but necessary due to an abundance of caution. She also had a hospitalization for syncopal episodes, but after evaluation by a cardiology team and extensive testing, no cardiac etiology could be ascribed. In 2005, the patient’s statin was switched to rosuvastatin due to worsening lipids. The initial dose was 5 mg daily and that dose was reduced over time to 5 mg weekly. Eventually, due to the expense of rosuvastatin, the patient was switched to atorvastatin 10 mg daily. After the patient was stabilized from a cardiac standpoint, she has done well with no further interventions other than her medical therapy with statin, calcium channel blocker, and aspirin. She currently lives at home, free of any clinical ATD, other than the mild case of heart failure noted previously.
Treatment of this patient’s dyslipidemia and hypertension was sufficient to bring and maintain her CRF-SBP plot below the threshold line virtually all of the time and her LDL-cholesterol at or below 80 mg/dl (precipitation method of HDL-cholesterol measurement, but 70 mg/dl if the enzymatic method of HDLcholesterol is used) most of the time. She has had no adverse reactions to this treatment regimen. She has had no other cardiovascular interventions beyond her statin/calcium channel blocker/aspirin therapy. She currently lives in her own home.
Discussion
This patient represents the only case to the author's knowledge of a lady with a history of severe ATD who has been treated with statins beyond the age of 100 years. She has done well on her statin/calcium channel blocker/aspirin regimen and has had not clinical recurrence of her ATD symptoms.
Unfortunately the anti-cholesterol/anti-statin crusades are alive and well and vigorously contested on the internet-specifically on Medscape/theheart.org website. These often scathing attacks on the Cholesterol Crusade are sparked by the publication of articles in the medical literature that attempt to discredit aspects of the link between cholesterol and ATD [20,21]. While other articles criticize the current guidelines [22,23]. Under the most favorable interpretation, these articles are meant to point out areas of the Cholesterol Crusade that need to be improved upon, but they also serve to spark controversy on the Internet.
Many of the bloggers advocate for their own points of view, suggesting that ATD has little to do with cholesterol but rather to do with insulin resistance (minus the lipid intermediary), defects in Vitamin D metabolism, inflammation (minus the lipid intermediary), oxidative stress (minus the lipid intermediary), etc. Above all, the bloggers decry the use of statins in the prevention of ATD but instead opt for dietary (often decreased dietary sugars) measures or increasing exercise as the primary means of preventing ATD. They justify this position by listing a panel of statin adverse effects, claiming that statins are the most dangerous medications in the world and leading to cancer, myopathy, renal disease, and dementia. They further claim that statin trials do not show a decrease in ATD or over-all mortality. They strongly contest any suggestion that more and more people should be placed on statin therapy.
The Helsinki Heart Study involved the use of gemfibrozil and was the first randomized controlled clinical trial (RCCT) to show a decrease in ATD mortality, but this effect was counterbalanced by an increase in non-ATD mortality, specifically in violent death [24]. Not long thereafter was published the Scandinavian Simvastatin Survival Study (4-S), a RCCT using simvastatin, and this study showed a decrease in both ATD and over-all mortality [25]. Other studies have affirmed the 4-S study findings [26-31].
Many researchers have studied the adverse sequelae of statin therapy, and found the risk of rhabdomyolysis to be rare, though the risk of myopathy is not so rare and indeed is the most common cause of so-called statin intolerance. (Statin intolerance may not be reproducible on repeat challenge) [32]. Statins may help treat chronic renal disease [33]. An increased cancer rate was found in only two studies: Cholesterol and Recurrent Events Trial and Pravachol in Elderly Individuals at Risk of Vascular Disease [8,26]. It was not found in Jupiter or the Heart Protection Study [29,30]. The Cholesterol Treatment Trialists Collaboration has analyzed 21 trials (129, 526 patients) and found no increased cancer risk [34]. The NLA committee on the statin safety has summarized its findings on these adverse reactions and found statins to be generally well-tolerated and safe [3].
The risk of dementia may be more attributable to people on statins living longer, but this manuscript cites the case of a 101 and ½ year old patient who has taken statins for decades and is not demented. Moreover, the author had another patient who had taken statins for decades and who at age 90 years decided to stop taking her statin. Two years later she was totally demented and confined to a nursing home. She was not demented when she made the decision to stop taking her statin. The author does have a patient who, at age 84 years, became demented while taking a statin; the patient’s family history is of no help since no male member of his blood line survived age 69 years, all dying of ATD. However, the author’s lipid clinic has been on-going for decades and very few statin-treated patients in his lipid clinic have developed dementia despite many patients being in their eighth and ninth decades of life. And lastly, the author himself has been on statins for over 20 years and is not demented.
As to goals of treatment, there is no RCCT’s specifically studying dyslipidemic therapy in people aged 80 years and over, or for that matter aged 75 years or older. Hence, goals of treatment of dyslipidemia in the very old must be extrapolated from RCCT’s done in younger patients and modified by expert opinion. The NLA roundtable discussed this issue and it was pointed out that the pathogenesis of ATD is not different in younger versus older patients and hence why should the goals of therapy be different. The author would add a caveat: more fibrotic, calcified plaques might well interfere with reverse cholesterol transport by interfering with the ability of apo A-1 on the HDL-cholesterol particle to attach to the ABC receptor to remove cholesterol from macrophages and so therapeutic manipulation of the HDL-cholesterol particle may be less effective in some very old patients [1].
The 102 and ½ years old subject of this report had her CRF-SBP plot virtually always below the threshold line, but her LDL-cholesterol level was not infrequently above 80 mg/dl (2.0 mmoles/L) (precipitation method of HDL-cholesterol measurement, but 70 mg/dl (1.75 mmoles/L) when the enzymatic method of HDLcholesterol measurement is used). This suggests that the BGS graph can function as an alternate goal of therapy in dyslipidemic patients, with the caveats that if LDL-cholesterol is very high, then LDL-cholesterol must be brought down to below 170 mg/ dl (4.25 mmoles/L) (precipitation method of HDL-cholesterol measurement, but 160 mg/dl (4.0 mmoles/L) if the enzymatic method of HDL-cholesterol measurement is used). The second caveat is that if HDL-cholesterol is very low, the CRF will always be high, so that in such cases the CRF is abandoned and LDLcholesterol maintained at 79 mg/dl (2.0 mmoles/L) (precipitation method of HDL-cholesterol measurement, but 70 mg/dl (1.75 mmoles/L) when the enzymatic method of HD-cholesterol measurement is used) or less.
The author would like to note that in addition to lowering her LDL-cholesterol levels, the patient also had a rise in her HDLcholesterol level levels over time. She thus fulfilled the criteria for Esko Nikkila, MD,’s Lipid regulatory Hypothesis (described in reference 24), which states that maximal plaque stabilization/ regression occurs when LDL-cholesterol levels are lowered and simultaneously HDL-cholesterol levels are raised, a finding borne out angiographically. Moreover, her SBP was rarely below 120 mmHg, an important finding in light of the recommendations of the Systolic Blood Pressure Intervention Trial (SPRINT), which advocate a SBP goal of less than 120 mmHg [34-36].
As in any decision to initiate therapy in any patient, the risks of treatment must be weighed against the benefits. In the case of statin therapy, treatment may be withheld if the patient’s life expectancy is limited or if the patient has multiple co-morbid conditions. And, of course, secondary causes of dyslipidemia should always be sought since correction of the causative factor (such as hypothyroidism) may well bring lipid levels back to ideal.
Conclusion
This report describes a patient who sustained a severe ATD event and who eventually stabilized on statin, aspirin, and calcium channel blocker therapy. She is now 102 and ½ years old and continues on therapy. This report supports the safety of statin therapy in the elderly and reports the first case, to the author’s knowledge, of a patient treated to beyond age 100 years. This report is not intended as proof that dyslipidemia in the elderly must be treated, but rather is intended to show what is possible.