Research Article - (2022) Volume 7, Issue 6
Received: 01-Jun-2022, Manuscript No. ipjtac-22-13782; Editor assigned: 03-Jun-2022, Pre QC No. ipjtac-22-13782 (PQ); Reviewed: 17-Jun-2022, QC No. ipjtac-22-13782; Revised: 22-Jun-2022, Manuscript No. ipjtac-22-13782 (R); Published: 29-Jun-2022, DOI: 10.36648/2476-2105-22.7.134
Purpose: The literature is confusing when it comes to defining/differentiating periosteal reaction from periostitis, Sub-Periosteal New Bone Formation (SPNBF), and calcifying sub-periosteal hemorrhage. Furthermore, sub-periosteal fluid, readily seen on MRI, can be pus from osteomyelitis as well as hemorrhage from trauma. However, MRI is often obtained to evaluate for osteomyelitis, thus potentially leading to a confirmation bias where sub-periosteal fluid is attributed to infection. This is particularly concerning in cases of Non Accidental Trauma (NAT), where the history may be vague. In addition, trauma can produce elevated inflammatory markers, further clouding the picture. The purpose of this study is to report our experience with MRI and x-ray in patients with sub-periosteal hemorrhage, all of whom were ultimately diagnosed with NAT.
Methods: A retrospective search of the authors’ suspected abuse database (1997-2020) was performed to identify patients who had sub-periosteal hemorrhage on x-ray and/or MRI. Imaging findings were correlated with clinical history, inflammatory markers, and follow-up course.
Results: From the database, 2206 patients with skeletal surveys were identified, aged 3 weeks to 12 months old. Of those, MRIs had been obtained as a workup for infection in 5 cases of unexplained extremity swelling. Although MRI showed sub-periosteal fluid in all 5 cases, trauma was not considered as the etiology.
Conclusion: It is essential to avoid anchoring the radiological interpretation to infectious etiology, and thus consider hemorrhage as a potential cause of sub-periosteal fluid on MRI in an infant or young child to avoid missing a diagnosis of Non Accidental Trauma.
Alcoholic Intoxication; Trauma; Positive alcohol level
Periosteal reaction is a crucial radiographic finding not to be missed, especially on skeletal surveys, and may be present in the setting of a Classic Metaphyseal Lesion (CML), epiphyseal separation, direct blows, and clinically occult injuries [1]. However, the literature is confusing when it comes to defining and differentiating periosteal reaction from periostitis, Subperiosteal New Bone Formation (SPNBF), and calcifying sub-periosteal hemorrhage. These findings may be present in trauma, infection, metabolic bone disease and other entities, and their significance may prove difficult on radiographs as well as cross-sectional imaging such as MRI [2-5]. Additionally, traumatic injuries can serve as a nidus for infection, further clouding the etiology.
Subperiosteal Fluid
During skeletal growth the periosteum consists of 2 primary layers: an inner cambium layer and a superficial fibrous periosteum. Sub-periosteal fluid, which can be simple fluid, hemorrhage, or pus, is contained within the sub-periosteal space by the strong fibrous periosteum and the perichondrium. The perichondrium is located at the physis and represents the location where the superficial layer of the periosteum connects with the bony cortex. The increased vascularity at the metaphysis can predispose a patient to both an increased risk of hematogenous osteomyelitis as well as sub-periosteal hemorrhage [6,7]. Sub-periosteal fluid can underly intact periosteum as in sub-periosteal abscess or may be the result of a disrupted periosteum as in Salter-Harris fractures. MRI findings of sub-periosteal fluid can include fluid with increased T2 signal paralleling the shaft with a V-shaped tapering of the fluid as it approaches the physis/sub-periosteal bone collar [4].
Sub-periosteal hemorrhage is very difficult to detect radio- graphically in the acute phase, but rather is typically diagnosed in the sub-acute phase due to calcification [8,9]. This is most commonly present with trauma, including birth related trauma and severe manually administered forces seen with abuse, such as with a CML. CMLs, often described as corner or bucket-handle fractures on radiographs, have high specificity for Non Accidental Trauma (NAT) in infants less than 12 months [10,11]. CMLs are most common at the distal femur, proximal and distal tibia, proximal humerus and distal radius [11], often due to inflicted shearing forces (traction, torsion, and/or compression) on an extremity [6,10]. Centrally the fracture extends through the metaphyseal primary spongiosa adjacent to the chondro-osseous junction; peripherally the fracture line veers away from the chondro-osseous junction to separate a thicker metaphyseal fragment that includes the sub-periosteal collar (perichondral ring of LaCroix) [6,7,10-13].
Hemorrhage can elevate the periosteum from the underlying cortex and over the course of several days will eventually undergo mineralization and calcify (Sub Periosteal New Bone Formation), well seen on radiographs [6,8,11,14]. Unfortunately, there is little evidence in the literature to differentiate sub-periosteal hemorrhage from sub-periosteal abscess on MRI. Like hemorrhage in other areas of the body, sub-periosteal hemorrhage will calcify, which has been described in other diseases such as neurofibromatosis, scurvy, copper deficiency, and hypervitaminosis A [5,15-17]. However, there is no literature to our knowledge differentiating calcified sub-periosteal hemorrhage from sub-periosteal new bone formation as seen in healing fractures on follow up radiographs. In our experience, healing sub-periosteal hemorrhage ossification may develop slightly away from the shaft of the bone with a thicker and more amorphous appearance. This is different than other types of fracture healing periosteal reaction, which is just adjacent to the cortex.
Osteomyelitis
Bone infection typically manifests as low signal intensity on T1-weighted images, and high signal intensity on fluid-sensitive images, with infection usually demonstrated hyper enhancement [4,18]. An associated abscess will present as high signal intensity on fluid sensitive images with a non-enhancing center surrounded by a rim of enhancing tissue. This can be true of abscesses in the bone, in the soft tissue, as well as subperiosteal abscesses [4].
Inflammatory Markers
Trauma can produce an elevation in inflammatory markers, including elevated C-reactive protein (CRP), Erythrocyte Sedimentation Rate (ESR), and leukocytosis [19-21]. However, when there is no known history of trauma, these elevated labs might lead clinicians to an etiology of inflammation/infection, and trauma may not be considered.
Imaging Management
Standard radiologic workup for the child with suspected physical abuse, as per the American College of Radiology (ACR) Appropriateness Criteria, is a radiographic skeletal survey and cross-sectional imaging of head, usually CT in infants 12 months of age and younger [22,23]. Skeletal surveys are performed because fractures of inflicted trauma may often be clinically silent, particularly CMLs [24,25]. MRI of extremities is not considered as part of the imaging algorithm for suspected non-accidental trauma [26].
On the other hand, if there is concern for infection, in the evaluation of a young child with limp, extremity MRI has been deemed “usually appropriate” by the ACR [27]. As such, there is inherent conflict in interpretation of imaging; MRI is indicated for infection but not for trauma. Furthermore, as the radiographic findings of fracture may be missed on the initial skeletal survey [28], if a patient is placed on the pathway of evaluation for osteomyelitis, we are at risk of anchoring bias, and abnormal findings (sub-periosteal fluid) may be misinterpreted as infectious. Additionally, in pediatric medicine, evaluation often depends on and strongly emphasizes history provided by parents. However, history is often misleading or absent in the setting of NAT, thus clouding the diagnostic pathway.
In the presence of overlap of the above variables, sub-periosteal fluid seen on MRI is often interpreted as a sub-periosteal abscess. However, hemorrhage should also be in the differential. The consideration of sub-periosteal hemorrhage may allow for the identification of NAT even in the absence of radiographic findings of a fracture. The purpose of this study is to report our experience with MRI and x-ray in patients with sub-periosteal hemorrhage, all of whom were ultimately diagnosed with NAT.
This retrospective study was approved by the institutional review board and was compliant with Health Insurance Portability and Accountability Act guidelines. Our institution is a large tertiary care pediatric center, with over 320 beds. A retrospective search of the senior author’s (ESR) suspected physical abuse database yielded nearly 4000 cases of suspected NAT over 21 years, 1997-2020. Of those, 2206 had undergone skeletal surveys as part of an initial work-up for non-accidental trauma. The sub-database of 2206 patients was searched to identify those patients who had also undergone an extremity MRI.
At our institution, skeletal surveys follow the parameters outlined by the ACR: Including the thorax (AP, lateral, and bilateral oblique views), abdomen AP view, lumbosacral spine lateral view, skull (AP and lateral views), cervical spine lateral view, and AP views of the appendicular skeleton (humeri, forearms, hands, femurs, lower legs, and feet) [29]. At our institution, extremity MRIs also follow the guidelines provided by the ACR, including post-contrast (gadoterate meglumine at our institution) images [27].
All skeletal surveys, both initial and follow-up, and MRI’s, as well as their radiologic reports, were reviewed by two pediatric radiologists (JZ-4 years of experience, ESR-31 years of experience), with a focus on injuries specific for NAT [11,12,30,31]. In addition, the patients’ medical records were reviewed by the authors. All fractures on both the initial as well as the follow-up skeletal survey were recorded. The MRI’s were reviewed for the presence of sub-periosteal fluid, bone marrow abnormality, fracture and soft tissue abnormality. All imaging findings discussed in this study were based on consensus (JZ, ESR). All patients were seen at time of admission by our hospital’s child protection team. The final diagnosis of non-accidental trauma was reached by a child abuse pediatrician based on a comprehensive clinical history, physical examination, laboratory testing to rule out metabolic bone disease, radiologic findings, and discussion of each patient during multidisciplinary case reviews with law enforcement, social workers, and other child welfare officials.
4 patients ranging in age from 3-12 months at time of presentation (2 male, 2 female) met criteria of presentation with unexplained extremity swelling and underwent MRI as part of a workup for infection. One of these patients presented on two different occasions (cases 2 and 3) 15 days apart, for a total of 5 cases (Table 1).
Table 1: Summary of 5 cases. legend: temperature (temp), left (lt), right (rt), decreased (decr), possible (poss), elevated (elev), c-reactive protein (crp), white blood cells (wbc), erythrocyte sedimentation rate (esr), classic metaphyseal lesion (cml), salter-harris (sh). fracture (fx), subperiosteal new bone formation (spnbf), proximal (prox). osteomyelitis (om), subperiosteal (subp), soft tissue (st), differential diagnosis (ddx), skeletal survey (skel surv), bilateral (bl), distal (dis), non-accidental trauma (nat), child protective services (cps).
| CASE # | Age in mo | Clinical Presentation | Initial X-ray | MRI | Other fractures | Follow-up X-ray | Diagnosis of NAT |
|---|---|---|---|---|---|---|---|
| 1 | 12 F | LT leg swelling and pain | CML LT distal tibia (initially read as SH 2 fx) | Day 2-Reported as Tibial osteomyelitis with subP abscess bone marrow edema CML not seen on MRI | Day 4 Skel surv-RT radius, RT 6-8 ribs, RT humerus, BL Clavicles | Day 18-thick SPNBF | Not delayed |
| 2 | 10 M | Day 1 LT knee tenderness | STSW, but no FX | Day 2-SubP fluid concerning for infection bone marrow edema CML not seen on MRI | None | Day 16-thick SPNBF misinterpreted | 40 days |
| 3 | 10 M | Day 16 Not moving RT arm | Day 16 Amorphous SPNBF | Day 16 SubP fluid with adjacent ST edema-DDx of Caffey’s, dermatomyositis, infection bone marrow edema CML not seen on MRI | None | Day 40-further amorphous SPNBF of humerus, initially misinterpreted CML now apparent | 40 days |
| 4 | 4 F | Decr L arm movement, poss swelling | L prox humerus CML | Day 28-MRI correctly interpreted as healing FX bone marrow edema CML not seen on MRI | Day 1 Skel Surv Dis L radius, L fem CML | Day 27-F/up Xray amorphous SPNBF misinterpreted as infection | Not delayed Recognition of healing CML with SPNBF can obviate sedated MRI |
| 5 | 3 M | Flexed L hip | Distal tibia CML | Day 3 MRI subP fluid with adjacent ST edema- interpreted as OM bone marrow edema CML not seen on MRI | Day 1 skel surv BL dis fem healing CMLs BL healing rib Fx’s | 4 weeks later-thick SPBNF misinterpreted as physiologic periostitis.CML now apparent | Not delayed |
Two patients initially displayed focal tenderness (cases 1 and 2) and three presented with limited range of motion (cases 3, 4, and 5). Two cases involved the upper extremity (cases 3 and 4) and three the lower extremity (cases 1, 2, and 5). No patient had associated bruising at time of initial presentation. One patient (case 5) presented with subjective history provided by parent of fever, was febrile in our ED and had recurrent upper respiratory illness.
In case 1, a 12-month-old female presented with leg swelling. A CML was seen on initial radiographs (Figure 1a). Skeletal survey demonstrated multiple fractures. At first, only her CRP was mildly elevated, but by hospital day 4, ESR was abnormal. Inflammatory markers coupled with further swelling of her left leg was concerning for infection. A lower extremity MRI was obtained, which revealed sub-periosteal fluid (Figure 1b). This was interpreted as superimposed left distal tibia osteomyelitis rather than hemorrhage. Follow-up radiographs 15 days later demonstrated sub-periosteal new bone formation adjacent to bone (Figure 1c). The diagnosis of NAT was not delayed in this case, in part because of multiple other unexplained fractures in the setting of radiologically normal bones.
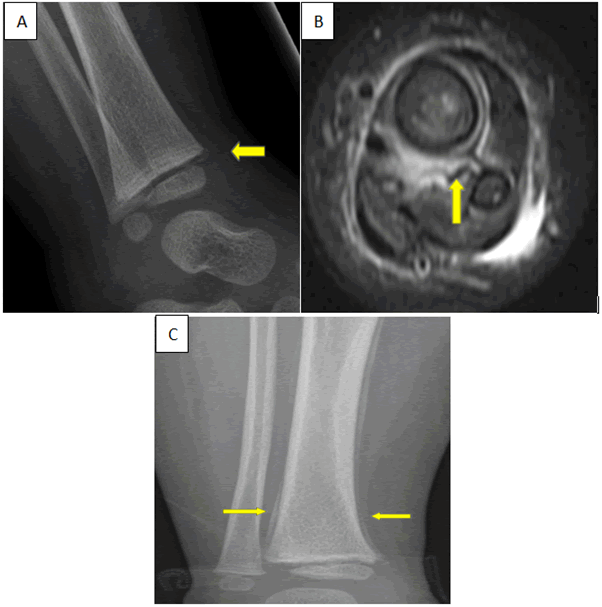
Figure 1: Classic metaphyseal lesion (CML) with subperiosteal hemorrhage. 13 month-old-female (case 1) who presented with leg swelling. a: Lateral Left Ankle radiograph at presentation demonstrates a corner fracture appearance consistent with a CML (arrow). b: Axial T2 weighted fat saturated MR images of the distal tibia and fibula demonstrate subperiosteal fluid (arrow), bone marrow edema, and surrounding muscle edema. This was reported as tibial osteomyelitis and myositis. c: Repeat radiographs of the lower leg 15 days after presentation show thick linear calcific densities (arrows) paralleling the cortex consistent with subperiosteal new bone formation.
In cases 2 and 3 (same patient), a 10-month-old male with left knee tenderness had no radiologically apparent fracture on initial radiographs (Figures 2 and 3). He was initially transferred to our institution for suspicion of infection due to clinical exam, peripheral leukocytosis and elevated ESR at outside facility. These labs were normal at our institution, where CRP was mildly elevated. Parent provided a history of subjective fever. Sub-periosteal fluid on MRI was interpreted as infectious (Figure 2b). Radiographs two weeks later showed thick sub-periosteal new bone formation paralleling the femur metadiaphysis (Figure 2c); there was no demonstrable fracture and trauma was not considered. Two weeks later he re-presented with decreased movement of his right arm. Radiographs showed amorphous calcific densities paralleling the proximal humerus metadiaphysis but slightly away from the cortex (Figure 3a). MRI demonstrated sub-periosteal fluid with soft tissue edema (Figure 3b) and he was given a differential diagnosis of Caffey’s disease, dermatomyositis, infection, and rheumatologic pathology.
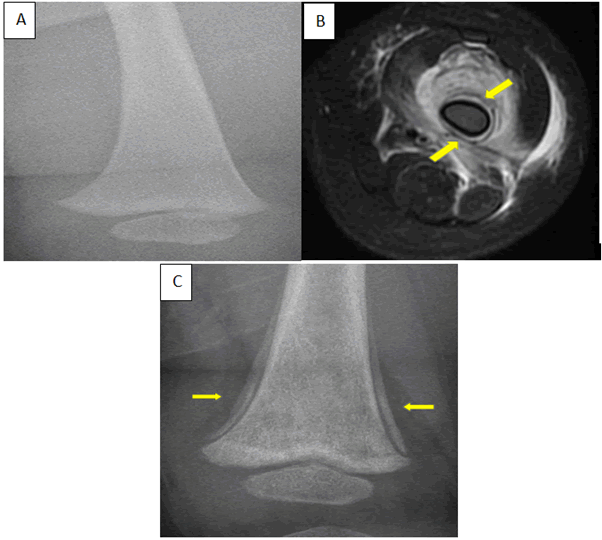
Figure 2: 10 month-old-male (case 2) who presented with left knee tenderness. a: Normal femur radiograph at presentation demonstrates no fracture. b: Axial T2 weighted fat saturated MR images of the distal femur demonstrate subperiosteal fluid (arrows) and edema within the surrounding musculature. The subperiosteal fluid was reported as being compatible with osteomyelitis. c: Repeat radiographs 2 weeks after presentation demonstrate thick linear calcific densities (arrows) paralleling the femoral cortex consistent with subperiosteal new bone formation; note that no fracture is evident.
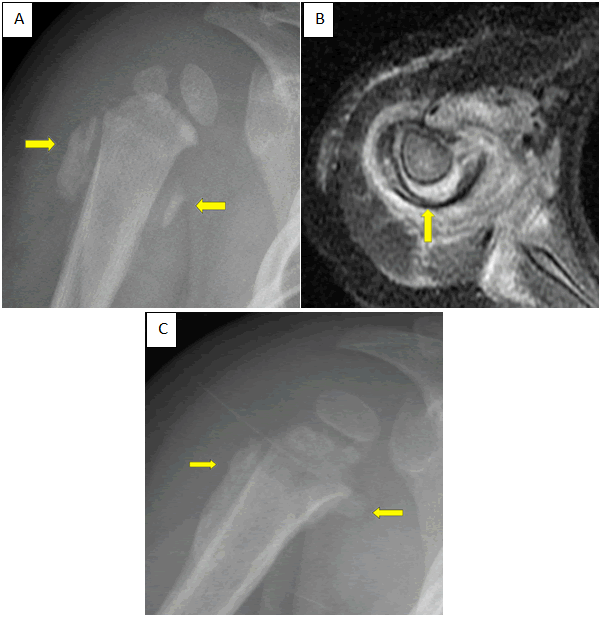
Figure 3: Same patient in Figure 2. a: Radiograph of the right shoulder 2 weeks after admission (time in 2a) demonstrates amorphous ossification (arrows) paralleling but slightly away from the proximal humerus cortex consistent with subperiosteal new bone formation. A CML is now apparent laterally. b: Axial T2 weighted fat saturated MR images of the shoulder demonstrate elevation/displacement of the periosteum off the cortex (arrow) and edema within the surrounding musculature. c: Repeat radiograph of the shoulder 40 days after admission demonstrate progression of the amorphous subperiosteal new formation (arrows) along the proximal humerus subperiosteal hemorrhage.
Hemorrhage and inflicted trauma were not considered. Forty days after initial presentation, follow up radiographs demonstrated progression of the now correctly identified amorphous sub-periosteal new bone formation (Figure 3c), and the diagnosis of inflicted trauma was made.
In case 4, a 4-month-old female with decreased left arm movement was correctly diagnosed with a proximal humerus CML on initial shoulder radiographs (Figure 4a). Follow up radiographs demonstrated amorphous sub-periosteal new bone formation which was misinterpreted as periosteal reaction suspicious for osteomyelitis (Figure 4b). This patient initially presented with a mild leukocytosis (13.9 k/mcl), although this normalized 4 weeks later at the time the x-ray was repeated. ESR and CRP were not obtained at presentation and were also normal at the time of repeat radiographs. MRI was obtained to rule out osteomyelitis due to the extensive calcific changes and initial high white blood cell count (Figure 4c). Sub-periosteal fluid was identified, although periosteal reaction and new bone formation were correctly attributed to a healing CML. Although the diagnosis of NAT was not delayed, this case demonstrates the challenge of definitively diagnosing trauma in the presence of the amorphous appearance of healing ossifying sub-periosteal hemorrhage that may be associated with classic metaphyseal lesions.
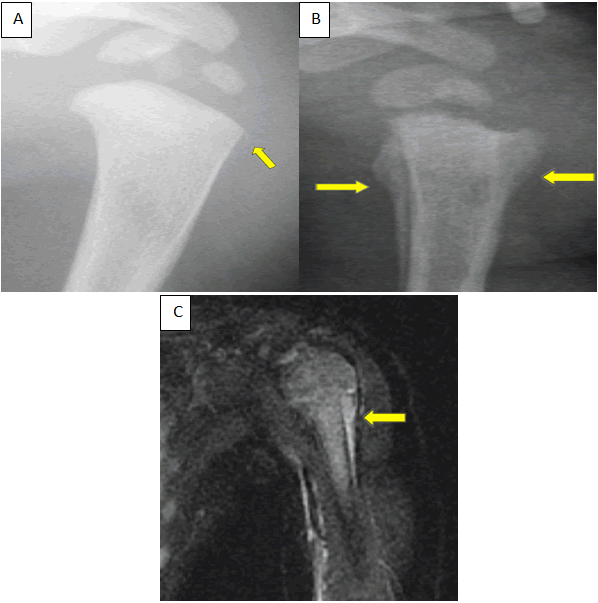
Figure 4: 4 month-old-female (case 3) that presented with decreased left arm movement. a: Shoulder radiograph at presentation demonstrates a fracture through the corner of the proximal humerus metaphysis (arrow) consistent with a CML. b: Repeat radiograph 27 days after presentation shows prominent amorphous subperiosteal new bone formation (arrows) along the proximal humerus metadiaphysis subperiosteal hemorrhage. c: Coronal T2 weighted fat saturated MR images of the shoulder demonstrate subperiosteal fluid with elevation/displacement of the periosteum off the cortex (arrow).
In case 5, a 2-month-old febrile (t-max 39.1) infant presented with decreased movement of his left leg which he preferentially held flexed at knee and abducted. He was diagnosed with multiple fractures including bilateral distal femoral CMLs (not shown) and a bucket-handle left distal tibia CML (Figure 5a) on initial radiographs. On presentation, his peripheral WBC was normal but subsequently was elevated twenty-four hours later. His ESR was elevated at presentation but CRP was normal. CRP was not repeated. He underwent MRI for concern for superimposed osteomyelitis. MRI showed sub-periosteal fluid (Figure 5b), interpreted as compatible with osteomyelitis. Follow up tibial radiographs demonstrated sub-periosteal new bone formation (Figure 5c), which was misinterpreted as physiologic periostitis, despite the presence of abnormal asymmetric thick linear calcific density along the cortex extending to involve the metaphysis. However, the diagnosis of NAT was not delayed in this patient as the skeletal survey had demonstrated multiple fractures.
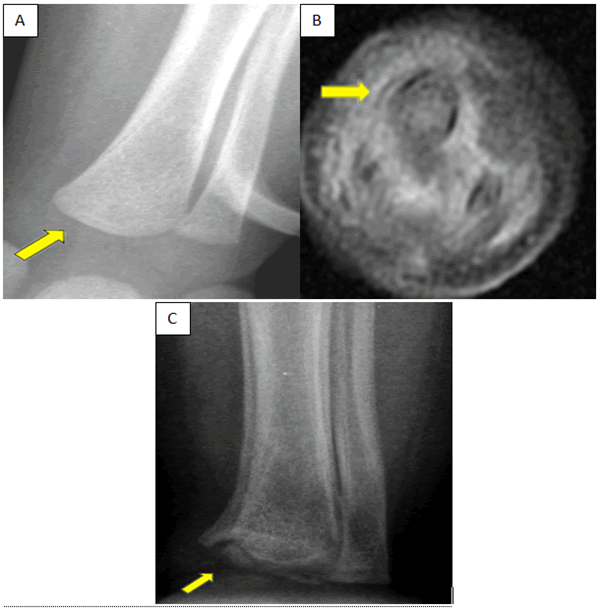
Figure 5: 3 month-old-male (case 4) that presented with a flexed hip. a:Distal tibia and fibula radiograph at presentation demonstrates a bucket handle fracture (arrow) of the proximal humerus metaphysis consistent with a CML. b: Axial T2 weighted fat saturated MR images of the distal tibia and fibula demonstrate elevation/displacement of the periosteum off of the cortex (arrow) with surrounding soft tissue edema. c: Repeat radiographs show increased thick linear calcific density along the cortex (arrow), consistent with subperiosteal new bone formation along the subperiosteal hemorrhage, which was misinterpreted as physiologic periostitis. A CML is now apparent along the medial tibia.
In summary, initial radiographs demonstrated a CML in three cases (1, 4, and 5), who also had additional unexplained fractures in the setting of radiologically normal bones, which from an imaging perspective is highly suspicious for inflicted trauma. An additional CML became apparent on follow-up plain film in cases 2 and 3 (the same patient who presented twice). MRI demonstrated bone marrow edema in four cases (1, 2, 3, and 4), with sub-periosteal fluid in four cases (1, 2, 3, and 5). CML was not seen on any MRI. Follow up radiographs demonstrated thick or amorphous sub-periosteal new bone formation in all five cases, but was misinterpreted in four cases (2, 3, 4, and 5) as osteomyelitis (cases 2,3, 4) and physiologic periostitis (case 5). All cases had at least one inflammatory marker (ESR, CRP, and peripheral WBC) elevated at presentation, though all three markers were not initially checked in all patients.
We have described our small experience with MRI and x-ray in patients with sub-periosteal fluid, all of whom were initially or ultimately diagnosed with non-accidental trauma. There are several variables in this arena with considerable overlap. The first is periostitis/periosteal reaction, which when seen on a radiograph, should engender a large differential diagnosis [13]. Physiologic periostitis is often seen in infants 1 to 5 months old, will appear smooth and usually bilaterally symmetric along the humeral, femoral, and tibial shafts, and should not be greater than 2 mm in thickness. Furthermore, physiologic periosteal reaction should be limited to the diaphysis and not extend to the metaphysis [5,12]. Aside from the physiologic type, periosteal reaction can be divided into benign and aggressive, both with an extensive differential including metabolic and neoplastic etiologies. Fracture healing periosteal reaction is one of the most commonly seen periosteal reaction etiologies.
Sub-periosteal hemorrhage may occur in the absence of any demonstrable fracture (cases 2 and 3), and the periosteum may or may not be intact. Sub-periosteal hemorrhage in the absence of visualized fracture typically indicates a significant torque mechanism/torsional force to the extremity, similar to the mechanism that may result in a classic metaphyseal lesion [32]. For this reason, these two injuries often coexist. Can we differentiate calcified sub-periosteal hemorrhage and fracture healing SPNBF? It may be difficult and not always relevant if both imply trauma. However, in our experience, healing sub-periosteal hemorrhage may be identified by the development of ossification, usually slightly away from the shaft of the bone and typically thick and amorphous in appearance. This is different than other types of fracture healing periosteal reaction which is adjacent to the cortex. This separation is likely due to the volume of fluid which has lifted the periosteum to produce new bone which is disconnected from the cortex. This notion needs to be evaluated on a larger study.
On MRI sub-periosteal hemorrhage in the acute phase will manifest as sub-periosteal fluid, which is easily identified. However, there are no definite MRI findings to differentiate sub-periosteal hemorrhage from abscess. As exemplified by our cases, because of its infrequent occurrence and the indication for which the MRI was done (often to evaluate for osteomyelitis), a cognitive bias can develop where hemorrhage may not be considered as a differential for the fluid. Thus, not recognizing this type of inflicted injury on radiography or not considering it on MRI may unfortunately result in delayed or misdiagnosis of non-accidental trauma. There is a paucity of literature on CML appearance on MRI. This may be related to the small nature of these injuries which may be obscured by overlapping inflammation/swelling.
Another confounding factor is that trauma can produce an elevation in inflammatory markers [19-21]. This is particularly true with more extensive trauma or head trauma but can be seen in isolated long bone fractures in adults [33,34]. Leukocytosis has been shown to occur in severe abdominal injury in the pediatric population and in severe trauma in adults [20]. ESR and CRP can be elevated in isolated long bone fractures [34]. As such, when there is no known history of trauma, these elevated labs paired with a swollen, painful extremity, can lead the clinician away from consideration of trauma. Careful information-gathering during the diagnostic process and avoidance of anchoring to infectious etiology is essential. Non-accidental trauma should remain on the differential especially in very young children. Future studies of the timeline for return of inflammatory markers to normal after long-bone trauma, especially associated with NAT, may be helpful to differentiate infection from injury in these cases. Further complicating the picture is that posttraumatic osteomyelitis is a relevant entity, as these fractures can become superinfected [18].
As such, superimposed infection may be present. But whether these patients had superimposed infection does not take away from the fact that they all had underlying trauma, and ultimately diagnosed with NAT. Additionally, sub-periosteal fluid of infection should not calcify like that seen in hemorrhage from trauma. However, as in our cases above, sometimes this is only determined retrospectively.
Lastly, the ACR Appropriateness Criteria may unintentionally lead to this dilemma. According to ACR Appropriateness Criteria, when there is no concern for infection, MRI is usually not appropriate [27]. Thus, MRI is usually reserved for cases when trauma is less likely and infection is higher in the differential diagnosis. On the other hand, in a young child with limp, if there is concern for infection, extremity MRI has been deemed “usually appropriate” by the ACR [27]. Thus, MRI is ordered when pre-test probability of infection is higher, which may confound interpretation as sub-periosteal fluid is already favored to represent infection rather than hemorrhage. Additionally, the ACR child with limp recommendations may be misapplied to children that are not walking.
Limitations
The primary limitations of this study are the small number of cases and its retrospective nature. Additionally, completely excluding osteomyelitis may be difficult in the absence of bone biopsy. Even if there was super-infection, the fact that trauma was not considered, is the problem that must be resolved. Furthermore, some of these cases may have simply been wrongly interpreted, and the findings should have suggested trauma. This may stem from the lack of literature on this topic.
Sub-periosteal fluid on MRI has a differential diagnosis that includes trauma. The nature of NAT and CMLs is that they may not be present on initial radiographs, leading to first encountering pathology on MRI. It is essential to avoid anchoring the radiological interpretation to infectious etiology, and thus consider hemorrhage as a potential cause of sub-periosteal fluid on MRI in a young child. Lastly, it may be difficult to distinguish periosteal reaction from healing trauma versus healing infection. In addition, in our experience, the thick amorphous appearance of sub-periosteal new bone formation slightly away from the bone is more typical for mineralizing sub-periosteal hemorrhage rather than infection. This distinguishing appearance is not widely known which may cause misinterpretation and possible delay in the diagnosis of non-accidental trauma. A larger study examining these differences is necessary to aid in its recognition.
Jonathan Zember, MD (Contribution: Lead author, manuscript preparation)
Rebecca Rohrer, MD (Contribution: First draft author, data gathering and manuscript preparation)
Tanya Hinds, MD (Contribution: Child and adolescent protection data input, manuscript preparation)
L. Kaleb Friend, MD (Contribution: Orthopedic data input, manuscript preparation)
Narendra Shet, MD (Contribution: Manuscript preparation)
Eglal Shalaby Rana, MD (Contribution: Mentor, study design, manuscript preparation)
Disclosure
Jonathan Zember, Rebecca Rohrer, Tanya Hinds, L. Kaleb Friend, Narendra Shet and Eglal Shalaby Rana have no conflicts of interest or financial ties to disclose.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zember J, Rebecca R, Tanya H, L Kaleb F, Narendra S, et al. (2022) Subperiosteal Fluid Misdiagnosed on MRI as Abscess. Potential to Miss Non-Accidental Trauma. Trauma Acute Care. 7:134.
Copyright: © Zember J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.