Burak Bilgin* and Aslan Guzel
Department of Ophthalmology, Bahcesehir University School of Medicine, Istanbul, Turkey
*Corresponding Author:
Burak Bilgin
Department of Ophthalmology
Bahcesehir University School of Medicine
Istanbul, Turkey
Tel: 905335601355
E-mail: burbilgin@yahoo.com
Received date: April 19, 2016; Accepted date: May 25, 2016; Published date: May 29, 2016
Citation: Bilgin B, Guzel A (2017) Success of Early Surgical Intervention in A Case of Idiopathic Intracranial Hypertension Presented with Nearly Total Vision Loss. J Eye Cataract Surg Vol.3:33. doi: 10.21767/2471-8300.100033
Copyright: © 2017 Bilgin B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Idiopathic intracranial hypertension; Vetriculoperitoneal surgery; Magnetic resonance imaging; Computerized tomography; Visual impairment
Introduction
Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri is a condition of elevated intracranial pressure (ICP) without laboratory pathology or intracranial structural abnormalities in radiological imaging techniques [1,2]. It is usually diagnosed in women at childbearing age but also may be seen in pediatric pupulation [3,4]. The disease presents with some of the sypmtoms such as headache, nausea, vomiting, visual impairment and diplopia. The major complication of the disease is visual impairment which can be progressive [5,6]. Management of the disease is determined by the severity of symptoms and visual impairment. Since the pathophysiology of the IIH is not well known, the main goal of the treatment is to decrease the ICP either medically or surgically. Early intervention is critical to prevent permanent function losss of visual system.
Here in, we report a 21 years old patient presented with sudden bilateral vision loss and was treated with vetriculoperitoneal shunt (VPS) surgery and cured with full recovery. To the best of our knowledge, this is the first case report that describes full visual recovery due to early surgical intervention after bilateral sudden vision loss. This report indicates the importance of early surgical intervention in cases with sudden vision loss due to IIH.
Case Report
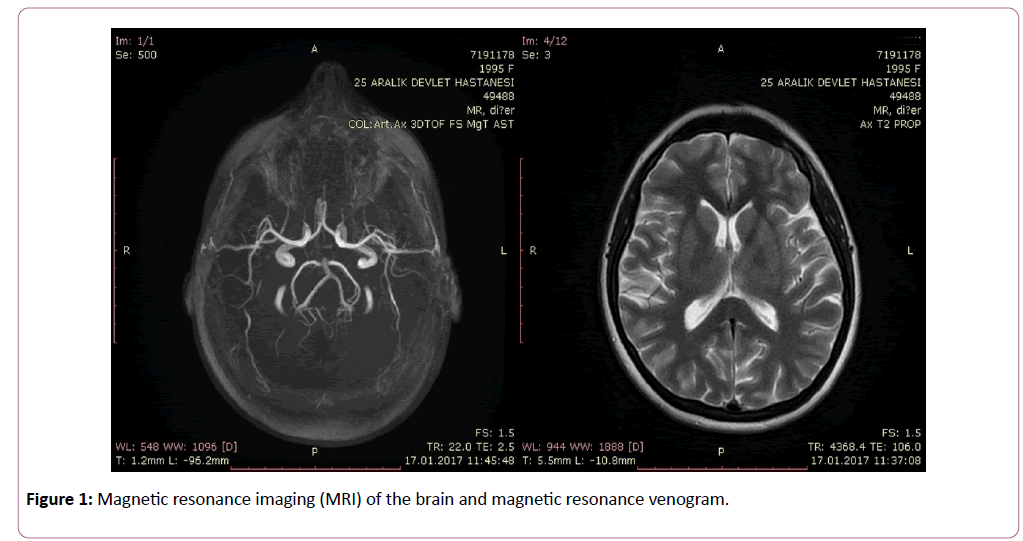
A 21 years old women, applied to the emergency department with a complain of sudden vision loss, vomiting and head ache. On further questioning she told that the complaints had started 2 months ago and worsened in the last week. Before sudden vison loss she had episodes of blurred vision. On general examination, her body temperature was 37.0°C, heart rate 76/ min, respiration rate 15/min and blood pressure was 110/70 mmHg. On ophthalmic examination; her visual acuity was ‘hand motion’ in the right eye and finger counting at 1 meter in the left eye. She had esotropia and lateral gaze restriction in the right eye. Direct and indirect light reflexes, intraocular pressure, and anterior segment were normal. Relative afferent pupillary defect (RAPD) was not seen. A dilated fundus examination revealed bilateral optic disc swelling, blurred disc margins, cotton wool exudates and splinter hemorhages surrounding the optic disc. Magnetic resonance imaging (MRI) of her brain with and without contrast and magnetic resonance venogram performed 2 days ago at a different clinic were normal (Figure 1).
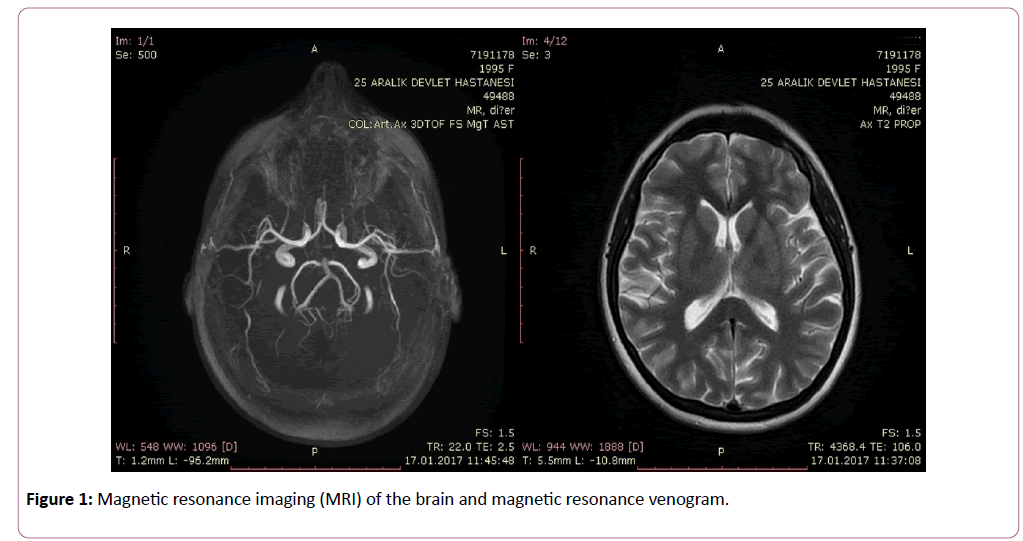
Figure 1: Magnetic resonance imaging (MRI) of the brain and magnetic resonance venogram.
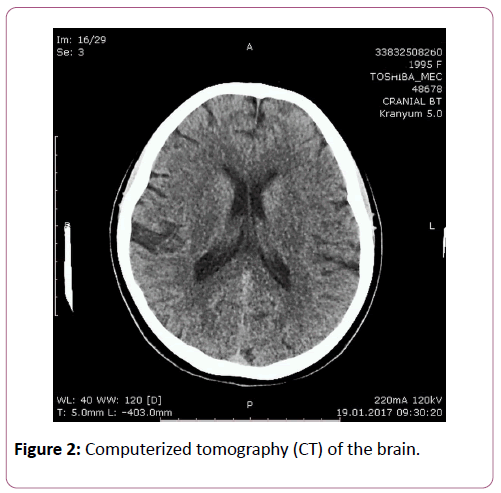
Computerized tomography (CT) of the brain was performed in our center and reported as normal (Figure 2).
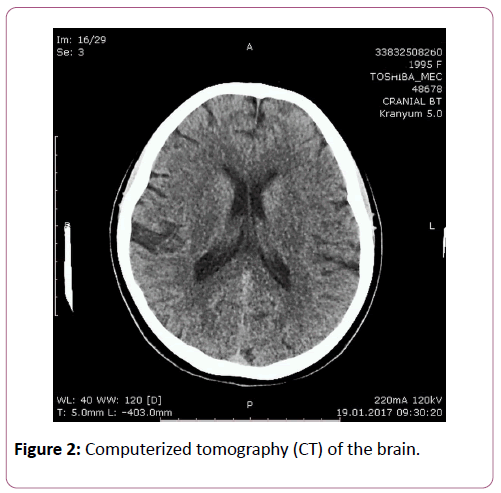
Figure 2: Computerized tomography (CT) of the brain.
Her medical, surgical and family history was unremarkable. Her neurological examination was normal except for papilledema and right sixth cranial nerve palsy. Laboratory tests including complete blood count, bio-chemistry panel, liver function tests were all normal. Diagnostic lumbar puncture was performed and opening pressure was measured as 540 mmH2O. Biochemical anaylyses of the cerebrospinal fluid (CSF) revealed normal protein, glucose and chloride levels. There was not any cell in the CSF. Bacterial culture of the CSF was negative which was resulted later. The patient was diagnosed as idiopathic intracranial hypertension and surgery was planned. VPS was installed successfully without any complication.
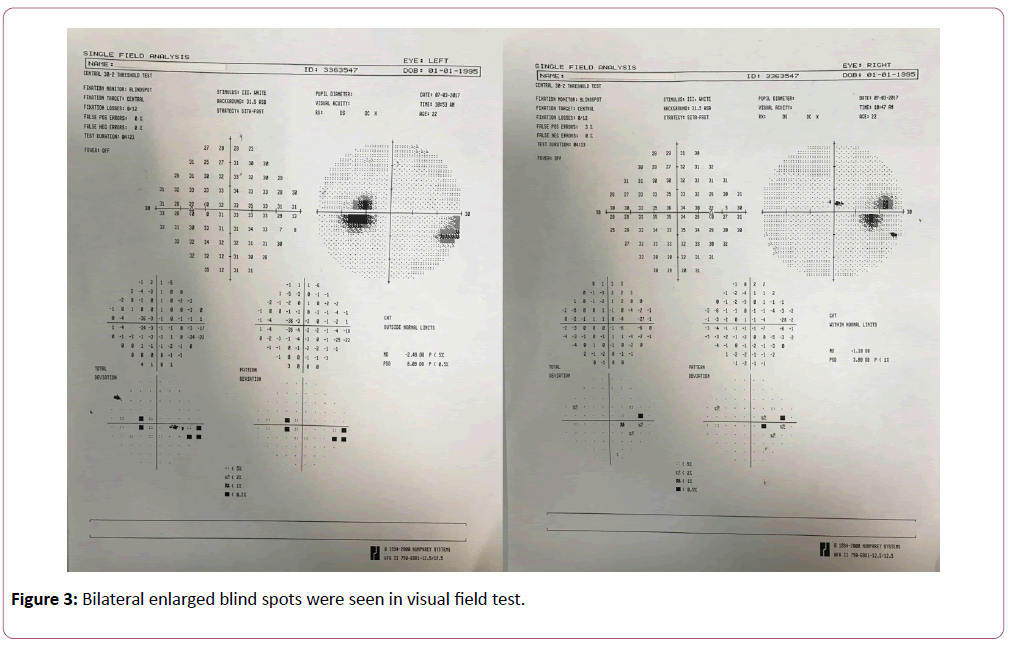
On ophthalmic examination performed at the first day after the surgery, her visual acuity increased dramatically and measured as 10/10 in her both eyes using Snellen chart. The esotropia was still present in her right eye and restriction of the lateral gaze was reduced. As a result, she had diplopia. In dilated fundus examination, papilledema signs were still present without any regression. The patient was discharged from hospital with her medical treatment and first week examination was scheduled. At the first week after surgery the esotropia and lateral gaze restriction in her right eye was hard to notice but still present. Papilledema signs were regressing. Patient was comfortable and not complaining about diplopia. Visual field testing using standartd automated perimetry with the 30-2 SITA-FAST strategy (Humphrey Field Analyzer II, Carl-Zeiss Meditec, Dublin, CA, USA) was performed. Bilateral enlarged blind spots were reported (Figure 3).
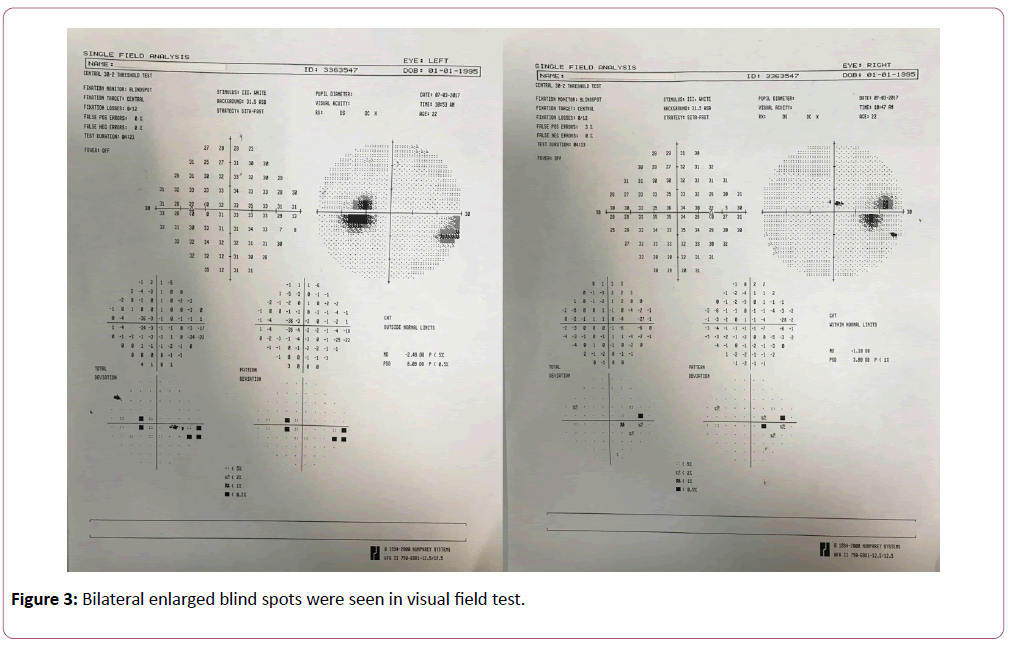
Figure 3: Bilateral enlarged blind spots were seen in visual field test.
At the third month after the surgery her ophthalmic examination was totally normal with 10/10 visual acuity in her both eyes. Papilledama signs were absent. There was not any restriction to lateral gaze in the right eye. She was ortophoric at the primary position.
Discussion
Management of IIH ranges from conservative medical treatment to surgical intervention. Saving the vision and reducing the symptoms are the main goals of the treatment. Severeness of the symptoms and visual impairment are considered when planning the time and type of the treatment. Asymptomatic patients who present with papilledema and have cooperance on follow up may be observed without medical or surgical intervention [7]. In our case, the patient had severe vision loss, headache, papilledema and sixth nerve palsy. The opening pressure of the lumbar puncture was 540 mmH2O. Immediate invasive management is recommended in cases of severe and sudden vision loss [1,8]. CSF diversion procedures such as ventriculoperitoneal shunting (VPS), ventriculoatrial (VA) or lumboperitoneal (LP) shunting [1] and optic nerve sheath decompression (ONSD) [9] are commonly performed surgical procedures. In this condition, we had planned and performed VPS surgery successfully.
Conclusion
Visual impairment is a major and serious complication of IIH. Considering the severeness of the symptoms, early intervention is critical to prevent permanent function loss of visual system.
References
- Biousse V, Bruce BB, Newman NJ (2012) Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry 83: 488-494.
- Friedman DI, Jacobson DM (2004) Idiopathic intracranial hypertension. J Neuroophthalmol 24: 138-145.
- Durcan FJ, Corbett JJ, Wall M (1988) The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana Arch Neurol 45: 875-877.
- Rangwala LM, Liu GT (2007) Pediatric idiopathic intracranial hypertension. Surv Ophthal 52: 507-617.
- Wall M, George D (1991) Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 114: 155-180.
- Corbett JJ, Savino PJ, Thompson HS, Kansu T, Schatz NJ, et al. (1982) Visual loss in pseudotumor cerebri. Follow-up of 57 patients from five to 41 years and a profile of 14 patients with permanent severe visual loss. Arch Neurol 39: 461-474.
- Dave SB, Subramanian PS (2014) Pseudotumor cerebri: An update on treatment options. Indian J Ophthalmol 62: 996-998.
- Bateman GA, Stevens SA, Stimpson J (2009) A mathematical model of idiopathic intracranial hypertension incorporating increased arterial inflow and variable venous outflow collapsibility. J Neurosurg 110: 446-456.
- Feldon SE (2007) Visual outcomes comparing surgical techniques for management of severe idiopathic intracranial hypertension. Neurosurg Focus 23: E6.