Raj Parikh*, Janice Stanley and Rajive Tandon
1725 W Harrison St, Suite 054, Chicago, IL 60612, USA
Corresponding Author:
Raj Parikh
1725 W Harrison St, Suite 054
Chicago, IL 60612, USA
Tel: 3129426744
Fax: 3129423131
E-mail: raj_parikh@rush.edu
Received date: March 15, 2016; Accepted date: March 18, 2016; Published date: March 25, 2016
Citation: Parikh R, Stanley J, Tandon R. Superior Vena Cava Syndrome Masquerading as Angioedema. J Intensive& Crit Care 2016, 2:2.
Introduction
SVC syndrome can masquerade as an acute allergic reaction and results from external or intrinsic obstruction of blood flow through the SVC [1]. Common factors, including mast cell degranulation or kinin formation, can occur in both angioedema and dermatomyositis [2,3]. We present a clinical image case report of a patient who presented with symptoms of angioedema though was eventually diagnosed with SVC syndrome.
Case Summary
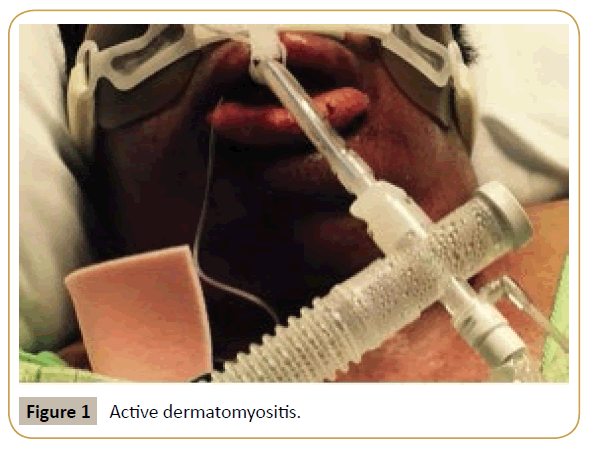
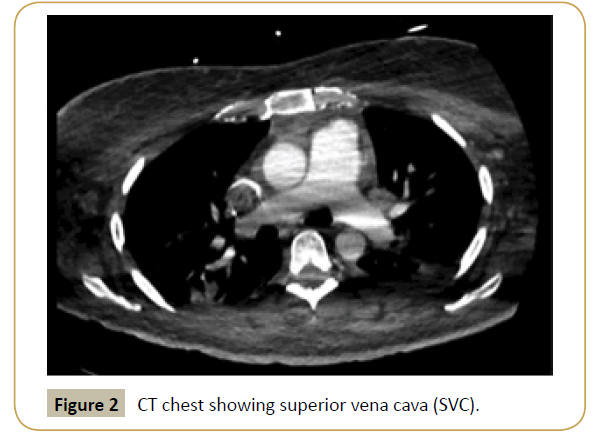
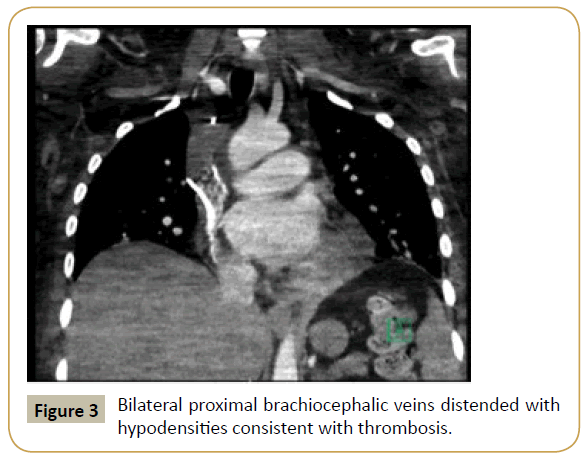
A 40-year-old woman with active dermatomyositis presented with fevers and left sided painful extremity swelling. Dermatomyositis flare was treated with IVIG and prednisone was increased. Empiric antibiotics were initiated for persistent fever with initial improvement seen. Subsequently, she developed significant facial and bilateral arm swelling thought to be angioedema and fevers up to 103°F despite restarting antibiotics (Figure 1). She was intubated, given higher dose steroids, and possible culprit medications were stopped. Fevers continued with tachycardia and declining platelet count. HIT antibody was negative. CT chest showed superior vena cava (SVC) and bilateral proximal brachiocephalic veins distended with hypodensities consistent with thrombosis (Figures 2 and 3). Unfractionated heparin infusion was started with improvement in her facial and lip edema.
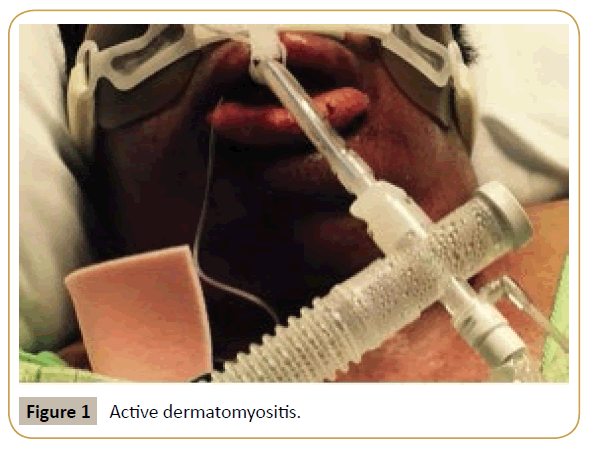
Figure 1: Active dermatomyositis.
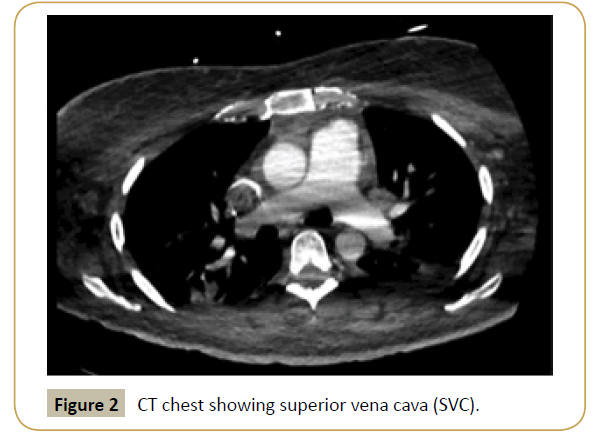
Figure 2: CT chest showing superior vena cava (SVC).
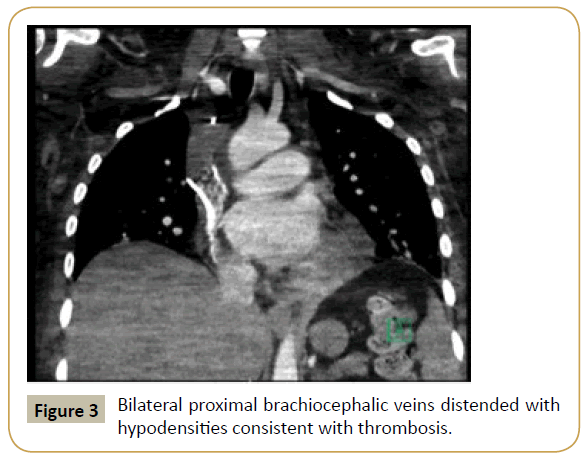
Figure 3:Bilateral proximal brachiocephalic veins distended with hypodensities consistent with thrombosis.
Discussion
SVC syndrome, caused by dermatomyositis, and angioedema typically manifest distinctly; however, given related inflammatory cascades, misdiagnosis is possible. Our case highlights the similarities in presentation between angioedema and SVC syndrome. Establishing the diagnosis of SVC syndrome is imperative as severe cases can develop cerebral edema or respiratory compromise.
References
- Monaco RG, Bertoni H, Lastiri R, Varela M, Beveraggi EM, et al. (2003) Use of self-expanding vascular endoprostheses in superior vena cava syndrome. Eur J CardiothoracSurg 24:208-211.
- Shrestha S, Wershil B, Sarwark JF, Niewold TB, Philipp T, et al. (2010) Lesional and nonlesional skin from patients with untreated juvenile dermatomyositis displays increased numbers of mast cells and mature plasmacytoid dendritic cells.Arthritis Rheum 62:2813-2822.
- Kaplan AP, Greaves MW (2005)Angioedema.J Am AcadDermatol 53:373-388.