Original Article - (2019) Volume 20, Issue 2
Luis Ferreira1, Mar Achalandabaso1, Henrique Alexandrino2,3, Justin Geoghegan1, Kevin Conlon1,4
1Department of HPB (Hepato-Pancreato-Biliary) and Liver Transplant, St Vincent´s University Hospital, Dublin, Ireland
2Department of Surgery, HPB and Liver Transplant Unit, Hospital and University Center of Coimbra, Coimbra, Portugal
3Faculty of Medicine, University of Coimbra, Coimbra, Portugal
4Department of Surgery, Trinity College Dublin, Tallaght Hospital, Dublin, Ireland
Received Date: February 09th, 2019; Accepted Date: March 20th, 2019
Introduction Solitary malignant melanoma metastasis to the pancreas is rare and occurs in approximately 1% of patients with metastatic malignant melanoma. Historically, most patients are considered unresectable. However, resection of isolated metastasis could enable disease-free survival benefit, particularly in the absence of effective systemic therapies. Methods We present our department experience of pancreatic resection for isolated MM metastasis along with a review of the English published literature. Patients with extra-pancreatic disease and patients who did not undergo surgery were excluded. Results and Discussion A 46 year old woman, with a right arm MM excised nine years ago, presented to our unit with an isolated tail of the pancreas mass on routine follow-up computed tomography. Laparoscopic distal pancreatectomy and splenectomy were preformed and revealed a 28 mm metastatic MM, with negative resection margins. The patient is asymptomatic with no recurrence two years after the resection. No adjuvant treatment was given. The literature review revealed three case series and 22 case reports with a total of 38 patients. The follow-up ranged from 1-264 months with a 5 year survival of 37.5% reported. Conclusions In carefully selected patients surgery may offer an overall survival benefit. Resection of isolated pancreatic metastases should be considered as it may provide a significant survival benefit for a disease with high mortality and lack of effective systemic therapies. Multidisciplinary decision and treatment in high volume centres is mandatory.
Melanoma; Neoplasm Metastasis; Pancreas; Pancreatectomy
BL biochemical leak; CT computed tomography; CTLA-4 cytotoxic T lymphocyte antigen 4; DP distal pancreatectomy; F female; FDG fluorodeoxyglucose; FDA food and drug administration; IL interleukins; LDH lactate dehydrogenase; Lap laparoscopic; M male; MM malignant melanoma; NK not known; PD pancreaticoduodenectomy; PD-1 programmed cell death protein 1; PPPD pylorus-preserving pancreaticoduodenectomy; S splenectomy; TP total pancreatectomy
Malignant Melanoma (MM) is the 6th most common cause of cancer in Western Europe (5th in the United States) and the 16th most common cause of cancer-related death in both Western Europe and the United States [1].
Solitary MM metastasis to the pancreas is rare and occurs in approximately 1% of patients with metastatic melanoma [2]. Historically most of these patients were deemed not suitable for resection. However, resection of isolated pancreatic metastasis could allow disease-free survival benefit, particularly in the absence of effective systemic therapies. We present a case of pancreatic resection for isolated malignant melanoma metastasis along with a review of the related literature.
The authors systematically reviewed the published literature up to January 2019 using PubMed and following the PRISMA guidelines [3]. The search was performed under the following Medical Subject Headings (MeSH) terms: melanoma, metastases, pancreas, and pancreatectomy. All the literature published in the English language was reviewed and the references were cross-checked for additional studies. Most were case reports. Patients with extra-pancreatic disease (diagnosed and treated before or at the time of diagnosis of pancreatic metastases) and patients who did not undergo surgery were excluded. The following data were obtained from each study: authors, year of publication, number of patients, age and gender, primary site, interval between primary and metastases, tumour size, surgery performed follow-up, outcome and recurrence.
A forty-six-year-old, Caucasian, female patient with previous history of right arm MM was referred to our Unit after a pancreatic mass was detected in her routine follow-up with thoracoabdominopelvic Computed Tomography (CT).
In 2007 she had underwent excision of a MM from the right arm staged as a pT1b, Breslow thickness of 0.5 mm, with no lymphovascular or perineural invasion, or micro satellite lesions identified; mitotic rate was 1 per 10 HPF.
In 2015, she presented with right side axilla lymphadenopathy for which she underwent unilateral axillary dissection. The pathology report revealed a deposit of metastatic malignant melanoma, 67 mm, likely representing a replaced lymph node. Extra-capsular extension was not identified. Immuno-phenotyping was consistent with metastatic MM (S100+; melanin A-). A further 12 nodes sampled were negative for tumour. She received adjuvant treatment with interferon alpha-2b.
In 2016, on a follow up CT scan, a new isolated hypodense lesion in the tail of the pancreas measuring 1.7 cm was identified (Figure 1).
A 18F-flurodeoxyglucose (FDG) positron emission tomography revealed a 2 cm focus of markedly increased FDG uptake in the tail of the pancreas, consistent with a solitary metastasis, with no other hypermetabolic suspicious areas identified (Figure 2).
The patient was referred to our Unit at this time and in a multidisciplinary meeting the decision was made to proceed with a laparoscopic distal pancreatectomy and splenectomy. The patient did not have any other medical history, medication or allergies. She also had a recent brain CT and oesophagogastroduodenoscopy, both of which were normal.
She underwent a laparoscopic distal pancreatectomy and splenectomy in February 2017. She made an uneventful recovery and was discharged home four days after the surgery with a surgical abdominal drain in situ, due to a Biochemical Leak (BL) pancreatic fistula [4]. She was reviewed in our out-patient clinic one week after discharge and the drain was removed.
Pathology report revealed a deposit of metastatic tumour in the pancreas consistent with metastatic malignant melanoma, 28 mm maximum dimension. Lymphovascular invasion was present. Two lymph nodes out of 21 were positive for metastatic melanoma. The resection margins were negative. The spleen was normal (Figure 3).
Figure 3: (a). Macroscopic image of tumour cut surface of resected specimen. (b). Histopathological appearance of resected tumour; (b1). Hematoxylin and eosin staining with tumour predominantly on the left with occasional residual pancreatic tissue and non-involved pancreas on the right (10x lens); (b2). Hematoxylin and eosin staining demonstrating a high mitotic rate (20x lens); (b3). Positive immunohistochemical staining of S-100 protein (10x lens).
The patient is currently well with no signs of recurrence two years after the resection and is undergoing followup at her local hospital. She did not receive any adjuvant treatment.
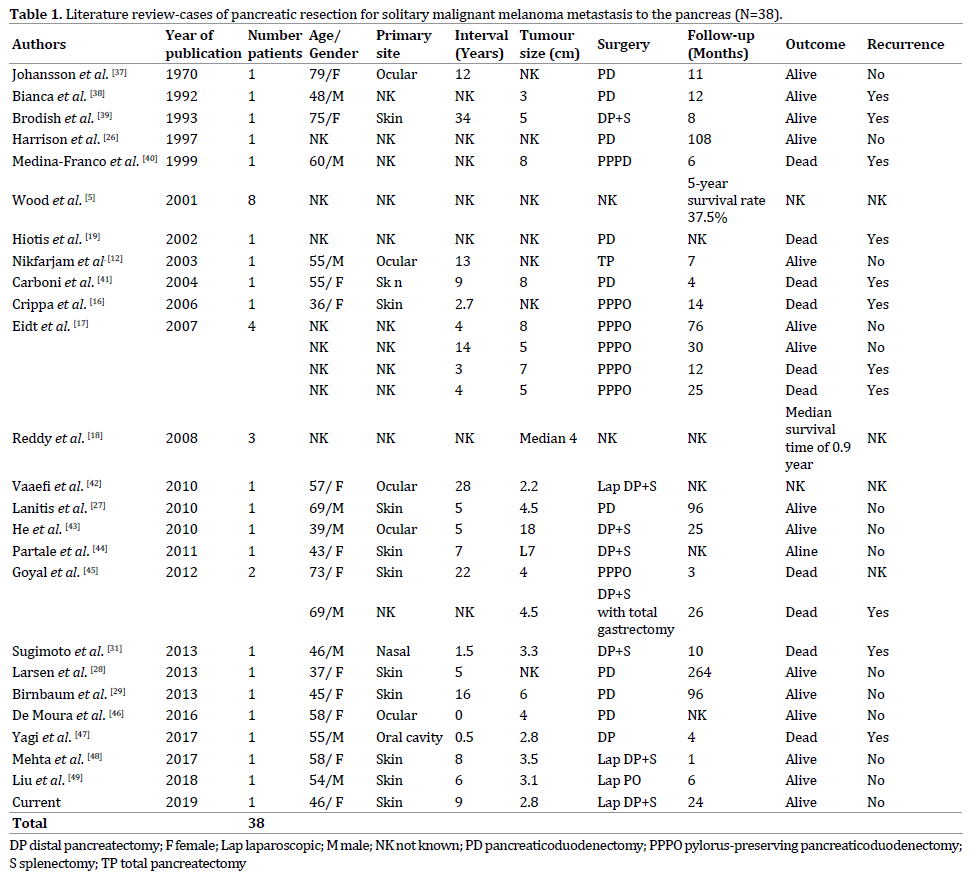
The literature search revealed three case series (more than two patients) and 22 single case reports, for a total of 38 patients with isolated MM metastases to the pancreas (Table 1). Among these patients, 11 had a primary skin MM, five had ocular MM, one had nasal cavity MM, another had oral cavity MM and in 20 the primary site was not reported. The interval between the primary diagnosis and development of metastases ranged from 0-408 months. The surgeries performed were: nine pancreaticoduodenectomies; seven pylorus-preserving pancreaticoduodenectomies; one laparoscopic pancreaticoduodenectomy; one open distal pancreatectomy; four open distal pancreatectomies with splenectomy; one open distal pancreatectomy, splenectomy and total gastrectomy; three laparoscopic distal pancreatectomies with splenectomy; one total pancreatectomy and in eleven cases the surgical procedure performed was not reported. A five-year survival rate of 37.5% was reported in one of the case series [5]. Recurrent disease was observed in 11 patients, 14 had no recurrence and 13 had no information regarding recurrent disease. Sixteen patients were alive, 10 patients had died and in 12 patients no information was available.
Malignant Melanoma is the 6th most common cause of cancer in Western Europe (5th in the United States) and the 16th most common cause of cancer-related death in both Western Europe and the United States [1]. According to the SEER program the incidence of MM has dramatically increased (7.89/100000 in 1975 – 25.23/100000 in 2017) [6] and in 2017 it is estimated that there will be 87,110 new cases of cutaneous melanoma and 9,730 people will die of this disease [7]. MM is the most rapidly increasing malignancy in men, and the 2nd most common cancer in women, surpassed only by lung cancer. The median age at diagnosis is 59 years and the lifetime risk of developing MM is 1 in 53 for men and 1 in 34 for women. Overall, a patient loses 20.4 years of potential life as a result of MM mortality compared to 16.6 for all malignancies [8].
Risk factors include male sex, age above 60, phenotypic predisposition, previous personal or family history of MM, use of immunosuppression and environmental factors [8].
The outcomes of MM depend, as with other malignancies, on the stage at presentation according to the TNM classification [8]. In the United States, it is estimated that 84% of patients will present with localized disease, 9% with regional disease, and 4% with metastatic disease [8]. Patients with stage IV disease can be further subdivided into those with only cutaneous metastases (IVa), lung metastases (IVb), or other visceral metastases (IVc) with associated 5-year survival rates of 18.8%, 6.7%, and 9.5%, respectively [9]. MM frequently metastasizes to the Gastrointestinal (GI) tract, with studies showing GI tract involvement in 50% to 60% of patients with MM at autopsies. However, a clinical diagnosis of GI involvement is only made in 1.5% to 4.4% [10]. Although these patients continue to have a poor prognosis, with a mean survival of 8–10 months [9], long-term survival after complete resection for GI tract metastases is reported [5, 11].
Metastatic tumours to the pancreas represent about 2% of all pancreatic malignancies [12, 13, 14]. According to a review of 418 patients with secondary tumours of the pancreas, the site of origin was renal cell carcinoma (70%), followed by MM (9.1%), colorectal cancer (8.9%), breast cancer (4.5%), sarcoma (4.3%), and lung cancer (3.1%) [12]. In another review of 243 patients with resected metastatic pancreatic tumours, the site of origin was renal cell cancer (61.7%), colorectal cancer (7.8%), melanoma (4.9%), sarcoma (4.9%), lung cancer (3.3%), gastric cancer (3.3%), gallbladder cancer (3.3%), and breast cancer (2.5%) [15].
Solitary MM metastasis to the pancreas is rare and occurs in approximately 1% of patients with metastatic melanoma [2]. Historically, most of these patients were offered either systemic or palliative treatment and were deemed unsuitable for resection. This was partly due to the fact that the 5-year survival was less than 10% and there was considerable morbidity and mortality associated with pancreatic surgery [2, 16, 17]. On the other hand, with the combined evolution of imaging techniques and surgical expertise, these resections have been effectively and safely performed with improvements in survival [16, 17, 18, 19]. Fletcher et al. achieved a 5-year survival of 18%, with a median survival of 15 months, following complete resection of solitary pancreatic metastases from MM [20].
Still, the role of resection in the management of isolated metastatic MM involving the pancreas is not well defined [18, 21].
Another factor to be taken into consideration is systemic therapies for melanoma. They have evolved slowly since the approval of dacarbazine by the U.S. Food and Drug Administration (FDA) in the seventies. Highdose interferon alpha-2b was sanctioned in the nineties for the adjuvant treatment of patients with MM. During that period, Fletcher et al. stated that surgical resection provides 5-year survival rates superior to any available nonsurgical therapy [20]. Since then, many other therapies have been or are being developed, namely, BRAF inhibitors, systemic and intralesional IL-2, Imiquimod/toll-like receptor activation, Bacillus Calmette-Guérin, interferon therapy, cancer vaccines, oncolytic vaccines, and adoptive cell therapy. More recently, the newer biologic agents, such as anti-CTLA4 therapy and anti-PD-1 have made an enormous impact on melanoma therapy [22].
Despite all the extensive research and drug development in the field of MM treatment, Duetsch et al. in a large study published in 2017 including 1623 patients with abdominal MM metastases, demonstrated that patients treated with surgical resection had better overall survival and that systemic treatment with newer agents did not have a significant effect on survival [23]. Several other authors have also found that long-term survival can be achieved when complete resection of pancreatic metastases is undertaken, typically in patients with renal cell cancer but also in patients with other primaries [11, 18, 19, 21, 24, 25]. Furthermore, some case reports, of patients undergoing pancreatic resection for isolated metastases from MM, support the idea that this approach improves overall survival [5, 26, 27, 28, 29]. One must also consider the benefits of a drug free period after surgical resection with curative intent.
When reviewing the literature, the authors identified few case series and single case reports in the surgical treatment of patients with isolated pancreatic MM metastases. Although pancreatic resections for juxta pancreatic MM metastases have been reported, these were excluded from our analysis [30]. Given the inherent difficulties in performing randomized prospective clinical trial in the management of this disease, it appears that in carefully selected patients with isolated pancreatic metastases amenable to complete resection, surgery may offer an overall survival benefit [5, 11, 18, 19, 21, 24, 25, 26, 27, 28, 29]. When selecting which patients should undergo surgery four principles should be considered. First, the patient age and comorbidities [23]; second, the tumour biology (primary site/pathology report of primary/ interval between primary and metastases) [2, 9, 10, 20, 23, 31, 32]; third the preoperative workup (imaging/LDH) [9, 10, 32, 33, 34, 35, 36]; and fourth a complete resection of all identifiable disease should be achievable [10, 20, 23].
Finally, given the rarity of this indication, the authors suggest that a large-scale multi-institutional, prospectively updated survey on surgical treatment of pancreatic metastases (in as much as the Livermet Survey for colorectal cancer liver metastases) could provide a more expanded knowledge on the prognostic factors involved, thus aiding in the decision-making process.
The authors fully acknowledge the limitations of this review. As stated above, the literature review revealed a heterogeneous collection of retrospective small case series and single case reports; the time interval between the first and the last article is nearly fifty years, with all the developments and expertise gained in the fields of adjuvant treatment and surgery. Furthermore, it is well recognised that cases/series with poorer outcomes are usually not reported in the literature; and we are also aware of the short follow-up in the case we describe. Nonetheless, there is sufficient encouraging experience with resection of isolated pancreatic metastases from MM that it should be considered in selected patients, as it may provide a significant survival benefit for a disease with high mortality and lack of effective systemic therapies. Multidisciplinary decision and treatment in high volume centres is mandatory.
All authors are in agreement with the contents of the manuscript. There is no conflict of interest.