- (2009) Volume 10, Issue 4
Leena Kylanpää1, Jaana Hagstrom2, Anna Lepisto1, Tiina Linjama3, Päivi Kärkkäinen2, Tuula Kiviluoto1, Caj Haglund1,2
1Department of General Surgery, Helsinki University Central Hospital; 2Department of Pathology, Haartman Institute, University of Helsinki and Helsinki University Central Hospital; 3Blood Service, Red Cross Finland. Helsinki, Finland
Context Since benign and malignant mucin-producing tumors of the pancreas may be difficult to distinguish from each other; preoperative methods for differential diagnosis would reduce unnecessary surgery. Objective To compare syndecan-1 and tenascin immunoexpression in benign and malignant cystic pancreatic tumors. Design We used immunohistochemical staining for syndecan- 1 and tenascin antibodies in tumor tissue samples. Setting Helsinki University Central Hospital. Patients Tissue material came from 33 patients undergoing surgery from 1979 to 2005 for cystic pancreatic tumors. Results A statistically significant difference appeared in syndecan-1 expression between benign (mucinous cystic neoplasms and intraductal papillary mucinous neoplasms) and mucinous carcinomas, but there was no significant difference in tenascin immunoexpression between these tumor groups. Conclusion Our findings suggest that low syndecan-1 expression might serve as a predictive factor for malignancy in cystic tumors of the pancreas.
Immunohistochemistry, Neoplasms; Pancreas
CT: computed tomography; ERCP endoscopic retrograde cholangiopancreatography; IPMN: intraductal papillary mucinous neoplasm; MCN: mucinous cystic neoplasm; MRI: magnetic resonance imaging
Mucinous cystic neoplasms (MCNs) of the pancreas are characterized by mucin-producing columnar epithelium with no ductal connection and ovarian-like stroma. The majority of patients are female. Intraductal papillary mucinous neoplasms (IPMNs) include papillary epithelium and mucin producing cells and arise from ductal structures. Both MCNs and IPMNs originate from mucinous epithelium, but only in the last decade have they been defined as different entities [1, 2].
IPMNs, first described in 1982, account for 5% of pancreatic neoplasms [3]. The overall prognosis is superior to that of ordinary pancreatic ductal adenocarcinoma, although a significant proportion of IPMNs are malignant. Typical clinicopathological features for MCNs include a prevalence for the female sex and ovarian-type stroma. It has been proposed that MCNs originate from endodermal immature stroma, the growth of which is stimulated by female hormones [4].
Syndecan-1 is a member of a family of core proteins which mediate cell-extracellular matrix adhesion by acting as receptors for molecules including extra cellular matrix proteins, cytokines, and growth factors. They control or influence tissue repair, metabolism, formation of tumors and the development of immune responses [5]. Syndecan-1 is known to be overexpressed in pancreatic adenocarcinomas [6, 7].
Tenascin is an extra-cellular matrix protein capable of interacting with other extra-cellular matrix proteins and cell-surface receptors such as syndecans. It is expressed during tissue remodeling and affects cell adhesion. Tenascin expression is mostly lacking in normal adult tissues, but it is overexpressed in pancreatic ductal adenocarcinomas and in chronic pancreatitis [8, 9].
Expression levels are higher in low-grade intraductal lesions than in high-grade lesions and invasive pancreatic lesions [8].
However, in pancreatic adenocarcinoma tenascin is not found to be a prognostic factor whereas syndecan-1 expression correlates with prognosis [6, 8, 9].
Cystic tumors of the pancreas are a challenging entity. The accurate preoperative differential diagnosis of a malignant cystic neoplasm from a benign cystic lesion remains unclear. Preoperatively, a suspicion of cancer would help the clinician to plan patient management in order to avoid unnecessary surgery and complications. We studied syndecan-1 and tenascin expression in MCNs and IPMNs, and compared their expression with that of their malignant counterparts. To the best of our knowledge, neither tenascin nor syndecan-1 expression has yet been reported in these benign tumor groups.
Patients
From 1979 to 2005, 33 patients underwent surgery for MCNs (n=12), IPMNs (n=6) or mucinous carcinomas (malignant invasive IPMNs or mucinous cystadenocarcinomas, n=15) at Helsinki University Central Hospital. Their characteristics are listed in Table 1. Pain was the most common symptom in all types of cystic tumor disease (Table 2). Only one patient had diabetes mellitus preoperatively. Tumor markers such as serum CA 19-9 and serum CEA were unable to accurately identify cancer (Table 1).
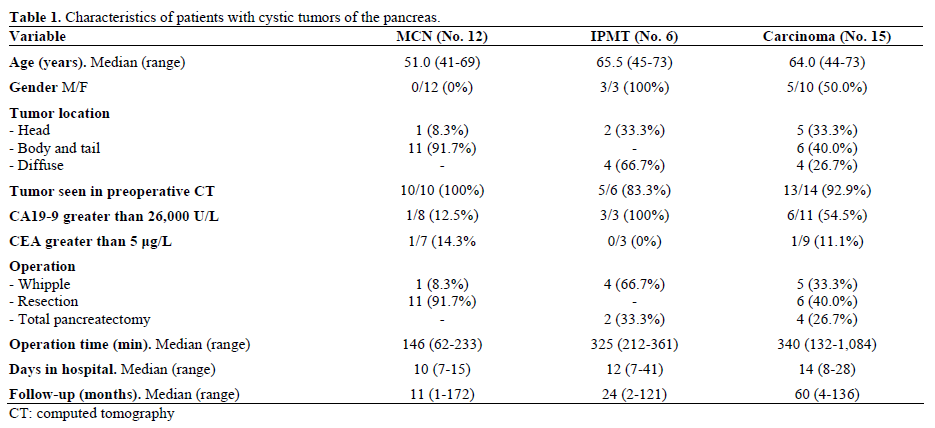

Preoperative computed tomography (CT) was performed on nearly every patient (Table 1). One patient with an MCN had been previously operated on by a gynecologist because of suspicion of a cystic ovarian tumor based on vaginal ultrasound. The tumor was, however, located in the body of the pancreas; a pancreatic resection followed. Another patient with an MCN had been treated in 1979 when CT was not yet readily available. One patient with an invasive IPMN did not undergo preoperative CT, but endoscopic retrograde cholangiopancreatography (ERCP) showed mucin coming from the pancreatic duct.
Surgery and Sample Collection
The type of surgery is shown in Table 1. All operations were performed with intention to cure. Two patients with carcinoma had lymph node metastasis. Tissue samples were collected by routine biopsy or were surgical specimens stored at the Department of Pathology, Helsinki University Central Hospital.
Immunohistochemistry
Formalin-fixed and paraffin-embedded tumor samples were cut into 4 μm thick sections. Before immunohistochemistry, the sections were deparaffinized in xylene and rehydrated through a graded ethanol series. The slides were treated in a PT module (LabVision UK Ltd, UK) in Tris-HCl buffer (pH 8.5) for 20 min at 98°C and with 0.3% Dako REAL Peroxidase-Blocking Solution (Dako, Glostrup, Denmark) to block endogenous peroxidases for 5 min. The immunostaining procedure was performed by the addition of monoclonal Tenascin-C clone DB7 antibody (1:50 diluted in Dako REAL Antibody Diluent; Biohit, Helsinki, Finland) or mouse monoclonal Syndecan/CD 138 antibody (1:2000; Serotec, Oxford, United Kingdom) for one hour, followed by a 30-min incubation with the Dako REAL EnVision/HRP (Dako, Glostrup, Denmark) detection system and rabbit/mouse reagent (ENV; Dako, Glostrup, Denmark). The slides were finally visualized by Dako REAL DAB+ Chromogen (Dako, Glostrup, Denmark) for 10 min. Between steps, the slides were washed with PBS 0.04%-Tween20. The slides were counterstained with Meyer’s hematoxylin and mounted in mounting medium (Aquamount, BDH, Poole, UK).
Evaluation of Immunostaining
Evaluation of the immunostaining was carried out by two independent pathologists who calculated the percentage of positive tumor cells. Positivity was cytoplasmic and only the epithelial tumor cells were evaluated. No positivity for syndecan-1 was graded as negative, up to 30% positivity as mild, 30-60% positivity as moderate, and over 60% positivity as strong. Tenascin immunostaining in the tumors was low and it was graded only as negative/positive.
Permission for this study was obtained from the local Ethics Committee, and the study conformed to the ethical guidelines of the Declaration of Helsinki.
The results are expressed as median, range and frequencies. For statistical analysis, we applied the liner-by-linear association chi-square test to the ordinal variable (syndecan-1) and the Fisher’s exact test to the dichotomic one (tenascin). A difference was regarded as statistically significant for a two-tailed P value less than 0.05. Statistical analysis was undertaken with SPSS 9.0 for Windows® (SPSS Inc., Chicago, IL, USA).
Complications
One patient operated on for an MCN developed a postoperative pancreatic fistula which was resolved conservatively. This patient also developed diabetes postoperatively.
Of the patients with benign IPMNs, two developed gastric retention which was resolved conservatively. One patient showed postoperative liver abscesses, probably partly due to her primary hypogammaglobulinemia.
In the carcinoma-patient group, one had stomach retention but recovered conservatively. Four patients needed re-operation. One patient had bleeding from the gastrojejunal anastomosis, one had necrosis of the omentum, one had leakage of the pancreatic anastomosis and one had leakage of the biliary anastomosis.
Follow-up
Seven patients with carcinoma died from cancer (46.7%) after surviving for an average of 15 months (range: 4-73 months) postoperatively. One patient developed a pulmonary metastasis which was operated on 19 months after the primary operation. After 5 years of follow-up, she has no new metastases (Table 1).
Analysis of Immunohistochemistry
Statistical analysis revealed that benign tumors (MCNs and IPMNs) expressed significantly more syndecan-1 than mucinous carcinomas (P=0.015; Figure 1). Between MCNs and mucinous carcinomas, the difference in syndecan-1 expression was statistically significant (P=0.030) but not between IPMN and simple carcinoma (P=0.167). No significant difference was observable in syndecan-1 expression between MCNs and IPMNs (P=0.606). The immunohistochemical expression of syndecan-1 among the groups of tumors is shown in Figures 1 and 2. Mild syndecan- 1 immunoexpression occurred in malignant tumors only (Figure 1).
Tenascin was negative in 3 cases of IPMT (50.0%) and one case of MCN (8.3%). It was positive in all carcinomas. No significant difference in tenascin expression existed between benign and malignant cystic lesions (77.8% vs. 100%; P=0.108). In IPMNs, the tenascin expression was lower than in MCNs and in mucinous carcinomas, but statistical significance was reached in comparison to mucinous carcinomas only (P=0.083 and P=0.015, respectively). MCNs and mucinous carcinomas showed almost identical tenascin expression (P=0.444).
On the basis of our data, it seems that IPMNs and MCNs express syndecan-1 and tenascin differently. In IPMNs, syndecan-1 expression does not predict malignant transformation. On the contrary, loss of syndecan-1 expression in mucinous carcinomas, when compared to benign cystadenomas, suggests that syndecan-1 may serve as a useful marker for the tumor classification of cystic neoplasms of the pancreas, together with radiological imaging techniques.
In recent years, due to improved imaging methods, an increasing number of cystic lesions of the pancreas have been identified. Neoplasms account for less than 10% of cystic lesions of the pancreas, with pseudocysts as the most common finding. Despite the excellent accuracy of CT or MRI, the diagnosis of a cystic lesion often remains uncertain. A history of episodes of pancreatitis and/or calcifications in the pancreas suggests the possibility of a pseudocyst
Here, all malignant cystic tumors of the pancreas were categorized into one group, since in most cases, it was impossible to determine whether the tumors originated from an MCN or an IPMN. This limited the possibility of comparing the marker expression of malignant cystic tumors with that of their benign counterparts, independently of whether the neoplasm originated from an MCN or an IPMN, which may be assessed as a limitation of the study. From a clinical point of view, it is important to distinguish preoperatively whether a cystic neoplasm of the pancreas is benign or malignant whereas knowledge as to the origin of the tumor is less relevant. In our patients, serum tumor markers or patient symptoms did not distinguish between benign and malignant cystic neoplasms. Preoperatively, it is possible to take a cytological sample with the aid of endoscopic ultrasonography. MCNs and benign IPMNs have a favorable outcome whereas the prognosis of invasive ductal carcinomas is poor. What requires further study is whether syndecan-1 staining of the cytological samples taken at endoscopic ultrasonography or at Wirsungoscopy will help in assessing the risk for malignancy in cystic tumors.
In a previous study, stromal syndecan-1 positive pancreatic tumors had a worse outcome than syndecan- 1 negative cancers [6]. In addition, the loss of syndecan-1 expression in malignant epithelial cells and its increased expression in stromal cells both predict the clinical outcome of invasive ductal breast carcinoma [10]. In ovarian cancer cells, the loss of syndecan immunoexpression is associated with enhanced invasion [11].
This study included only ductal adenocarcinoma patients and covered only epithelial syndecan-1 immunoexpression. According to our present results, elevated epithelial syndecan-1 expression was more often related to benign cystic lesions of the pancreas. Similar to our findings, in one colon cancer study, a reduction in syndecan-1 expression occurred in carcinomas when compared to adenomas [12]. Similar results have also been described in gastric cancer [13].
Management of cystic lesions of the pancreas remains debatable. For young asymptomatic patients at low surgical risk, surgical resection is recommended. However, in an elderly patient with moderate or high surgical risk and asymptomatic cystic lesions, the decision to operate is not so clear. Limitations in accurate diagnosis and incomplete understanding of the course of the disease make decisions difficult. Therefore, research on new tissue markers using immunohistochemistry to assess the nature of pancreatic lesions is important and might help in finding a diagnostic tool to differentiate malignant or potentially malignant lesions. Syndecan-1 expression may be helpful when reaching a final diagnosis. In conclusion, loss of syndecan-1 expression may be a predictive factor for malignancy of cystic lesions of the pancreas.
This study was supported by the Sigrid Juselius Foundation
The authors have no financial disclosures or conflict of interestq