- (2006) Volume 7, Issue 1
Kolitha Sanjaya Goonetilleke, Ajith Kumar Siriwardena
Hepatobiliary Unit, Department of Surgery, Manchester Royal Infirmary. Manchester, United Kingdom
Received: 19 July 2005 Accepted: 05 October 2005
Background Although nutritional supplementation is established in surgicalpractice, studies on feeding patients undergoing pancreaticoduodenectomy utilize widely disparate protocols, include small numbers of patients and have disparate endpoints. The aim of this study is to carry out a systematic review of peri-operative nutritional supplementation in patients undergoing pancreaticoduodenectomy in order to identify consistent themes. Methods Searches of the MEDLINE and EMBASE databases yielded 10 studies examining nutritional support in 571 patients undergoing pancreaticoduodenectomy. Data were retrieved on: proportion of pre-operative weight loss, biochemical parameters (preoperative albumin and the presence of jaundice), type and duration of nutritional support and clinical outcome (morbidity, mortality and hospital stay). Results Pre-operative percentage weight loss was similar in all studies evaluated. Routine post-operative total parenteral nutrition (TPN) was associated with a higher incidence of complications. Enteral nutrition reduced infective complications. Cyclical nutrition was associated with a lower incidence of postoperative gastric stasis. Conclusion Clear themes emerge from this systematic review. Patients undergoing pancreaticoduodenectomy are nutritionally depleted at the time of surgery and the preoperative period may present a window for intervention. Routine TPN is not beneficial. Routine post-operative enteral nutritional support, delivered on a cyclical basis appears to be the optimal mode of delivery.
Nutrition; Pancreatic Neoplasms; Pancreaticoduodenectomy
In current gastrointestinal surgical practice, peri-operative nutritional support is a widely accepted standard of care [1, 2, 3, 4]. In postoperative patients, in addition to providing caloric support at a time of intense catabolic activity, nutritional supplementation may reduce gut translocation [5] and infective complications [5, 6]. The consensus view from several randomised trials, meta-analyses and consensus statements favours perioperative nutritional support [7].
Although much of this evidence translates to all gastrointestinal surgical procedures, pancreatic surgery and in particular pancreaticoduodenectomy can logically be considered as a discrete category. Pancreaticoduodenectomy results in loss of gastric pacemaker activity due to removal of the interstitial cells of Cajal [8] and this together with the physiologic consequences of partial pancreatic resection and biliary and pancreatic diversion lead to a high incidence of postoperative gastric stasis. Recent evidence suggests that routine post-operative enteral nutritional support after pancreaticoduodenectomy may lead to an increased incidence of post-operative gastric stasis [9]. Further, the optimal timing of delivery of feed is unclear: should nutritional supplementation be given after surgery or should support cover the entire peri-operative period?
As the individual studies examining nutritional supplementation in patients undergoing pancreaticoduodenectomy are relatively small it is difficult to formulate a coherent management policy based on isolated reports whilst the wide variation in protocols between studies makes formal metaanalysis unfeasible.
In these settings systematic review of published evidence can be a valuable resource in identifying consistent themes across studies and areas of conflict. Further, the information gained can supplement existing data to help guide the evidence base for management of patients undergoing pancreaticoduodenectomy.
A computerized search of the National Library of Medicine MEDLINE database from January 1994 to November 2004 was undertaken together with searches of EMBASE from 1974 to 2004. In MEDLINE, the search terms “peri-operative OR postoperative OR pre-operative” yielded 167,080 hits. Combination of the terms: “nutrition OR parenteral OR enteral OR feeding OR nasojejunal OR nasogastric” yielded 115,592 hits. Finally, “pancreaticoduodenectomy OR Whipple OR pancreas cancer” yielded 2,133 hits. Combination of these three searches yielded 66 hits. Restriction of the search to studies in English and those reporting human studies resulted in 12 exclusions and a population of 54 studies. This process was repeated in EMBASE to yield a population of 89 studies. The MEDLINE and EMBASE searches were then combined and duplicates deleted to produce a population of 103 reports. The abstracts of these reports were then retrieved and studied. Studies were retained only if they were reports of nutritional supplementation in patients undergoing pancreaticoduodenectomy including (but not restricted to) randomised trials. Specifically excluded were case reports, review articles and studies not providing data on nutrition in patients undergoing pancreaticoduodenectomy. Studies on nutritional supplementation in upper gastrointestinal cancer patients, which included individuals undergoing pancreaticoduodenectomy, are also included but are reported separately. Application of these final filtration criteria resulted in the exclusion of 93 of the 103 studies to produce a final population of 10 studies.
Study Outcomes
Given the wide disparity in study protocols, definition of end-points and study outcomes, formal meta-analysis of pooled data is not feasible. Instead, data were collected on the design of the studies with specific attention to the protocols employed in randomisation arms, nutritional base line data (percentage of normal body weight lost prior to surgery), pre-operative albumin, the presence of preoperative jaundice, duration of nutritional support, morbidity, mortality and in-hospital stay.
Study Profiles of Trials of Peri-Operative Nutritional Support in Patients Undergoing Pancreatic Resection for Suspected Malignancy
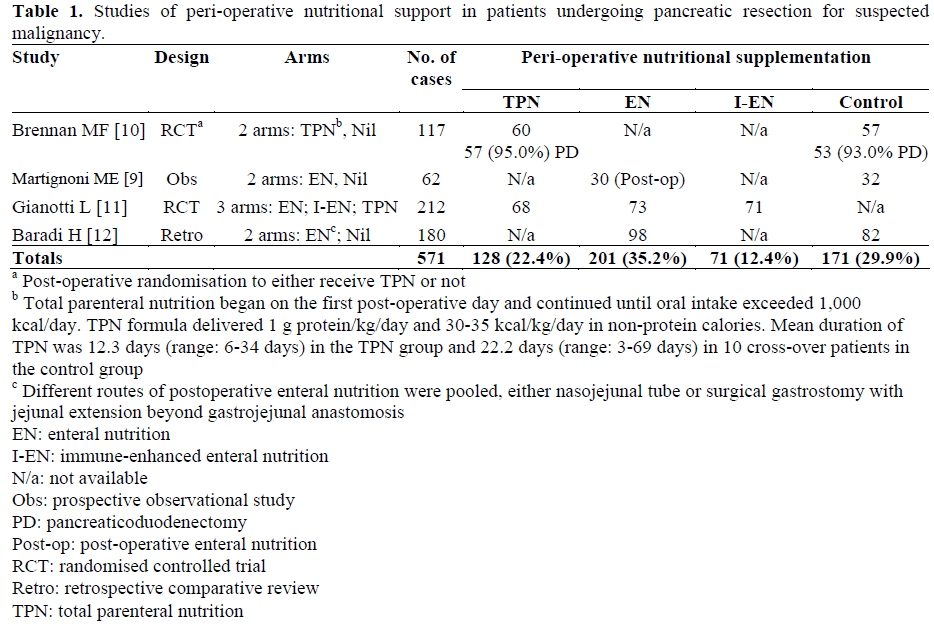
The study designs of the four trials of perioperative nutritional support in patients undergoing pancreatic resection are shown in Table 1. There were two randomised studies. There was a wide disparity in study protocols with a total of 571 patients being evaluated. Of these, 128 (22.4%) received total parenteral nutrition (TPN), 201 (35.2%) enteral, 71 (12.4%) immune-enhanced enteral nutrition and 171 (29.9%) controls had no initial post-operative nutritional support.
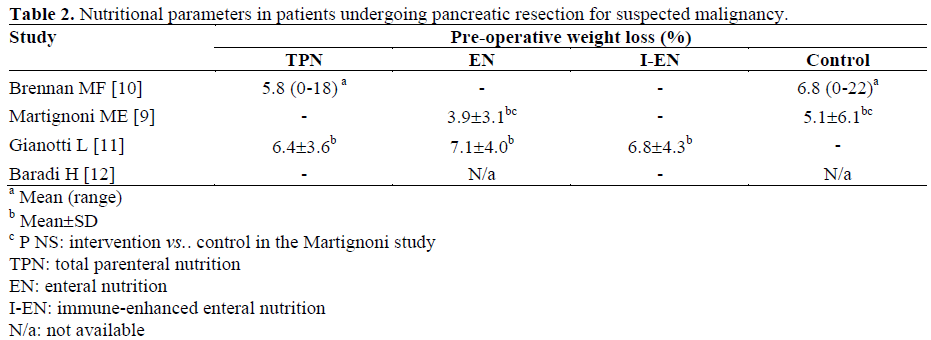
Nutritional Parameters
Percentage weight loss (immediate preoperative weight compared to stable preillness weight) data were available for three of the four studies (Table 2). The data show similar weight loss profiles across the studies and between groups within studies.
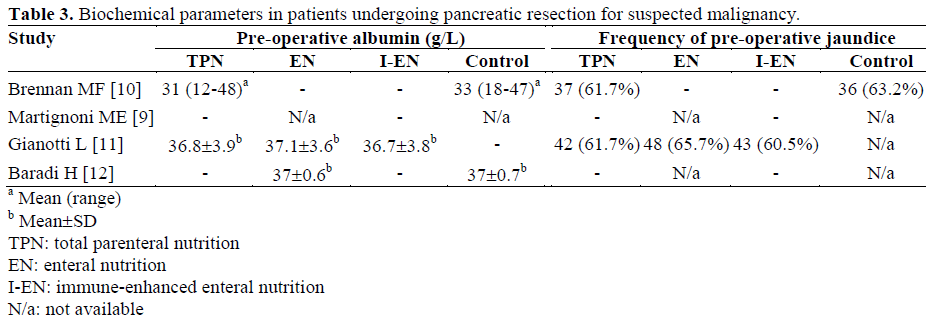
Biochemical Parameters
Data on pre-operative albumin levels were available in three studies (Table 3). Data on the presence of absence of pre-operative jaundice were available in two. No studies provided information on whether there were policies of routine pre-operative decompression for malignant obstructive jaundice in operation.
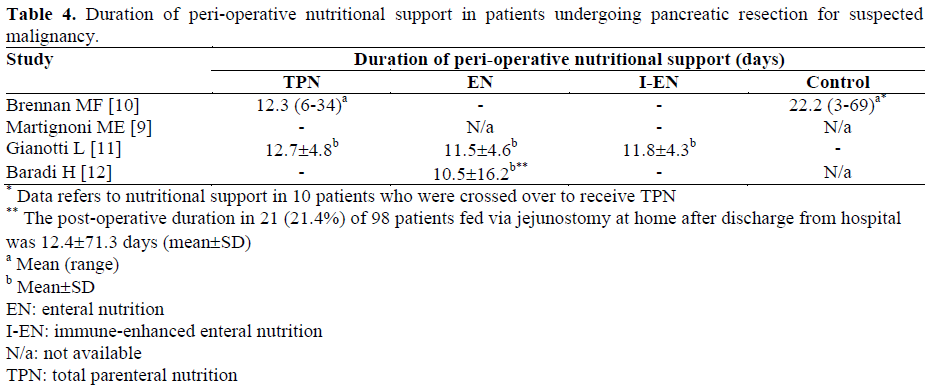
Duration of Nutritional Support in Studies of Pancreatic Cancer Resection Patients
Data on duration of peri-operative nutritional support were available in three studies (Table 4). In Baradi’s study, enteral nutrition was provided after discharge from hospital for 21 of 98 jejunostomy-fed patients [8].
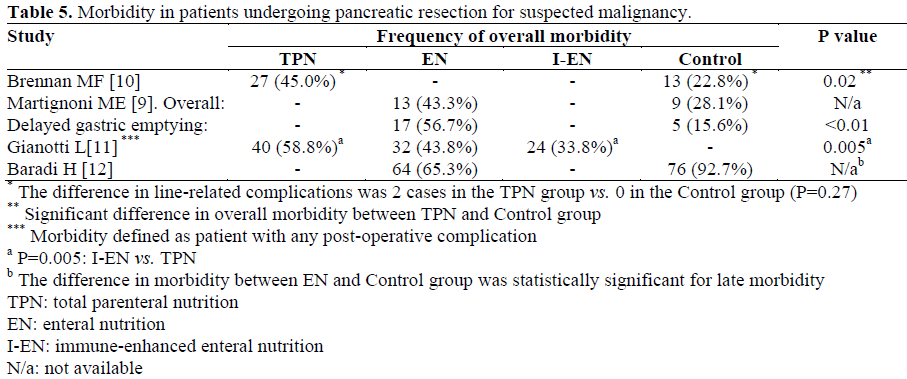
Morbidity, Mortality, Hospital Stay
There was no uniformity in the terminology used to describe post-operative complications and overall post-operative morbidity as defined by each individual set of authors was used. All four studies provide data on postoperative complications (Table 5). Martignoni’s study reveals a significantly higher rate of delayed gastric emptying in patients receiving post-operative enteral nutrition compared to non-nutritionally supported controls [9].
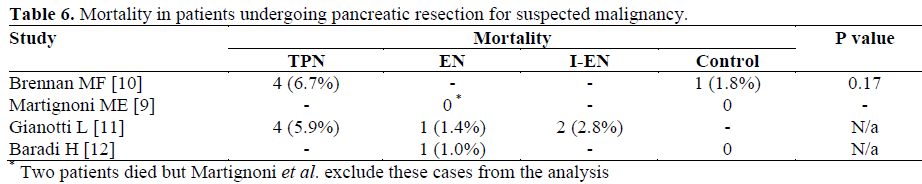
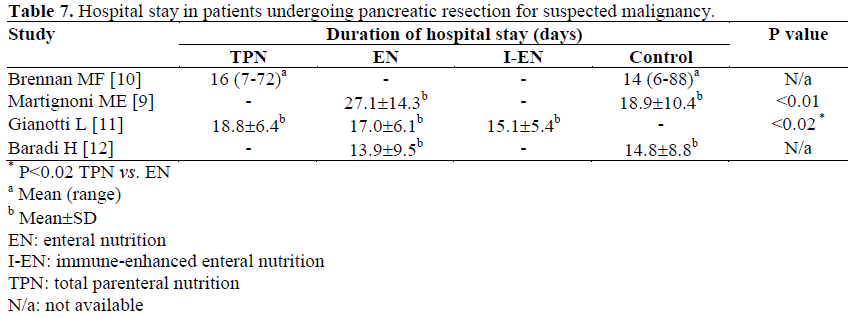
All four studies provide data on peri-operative mortality (Table 6) and duration of hospital stay (Table 7). TPN is associated with a higher mortality and a longer hospital stay compared to no TPN or enteral nutrition.
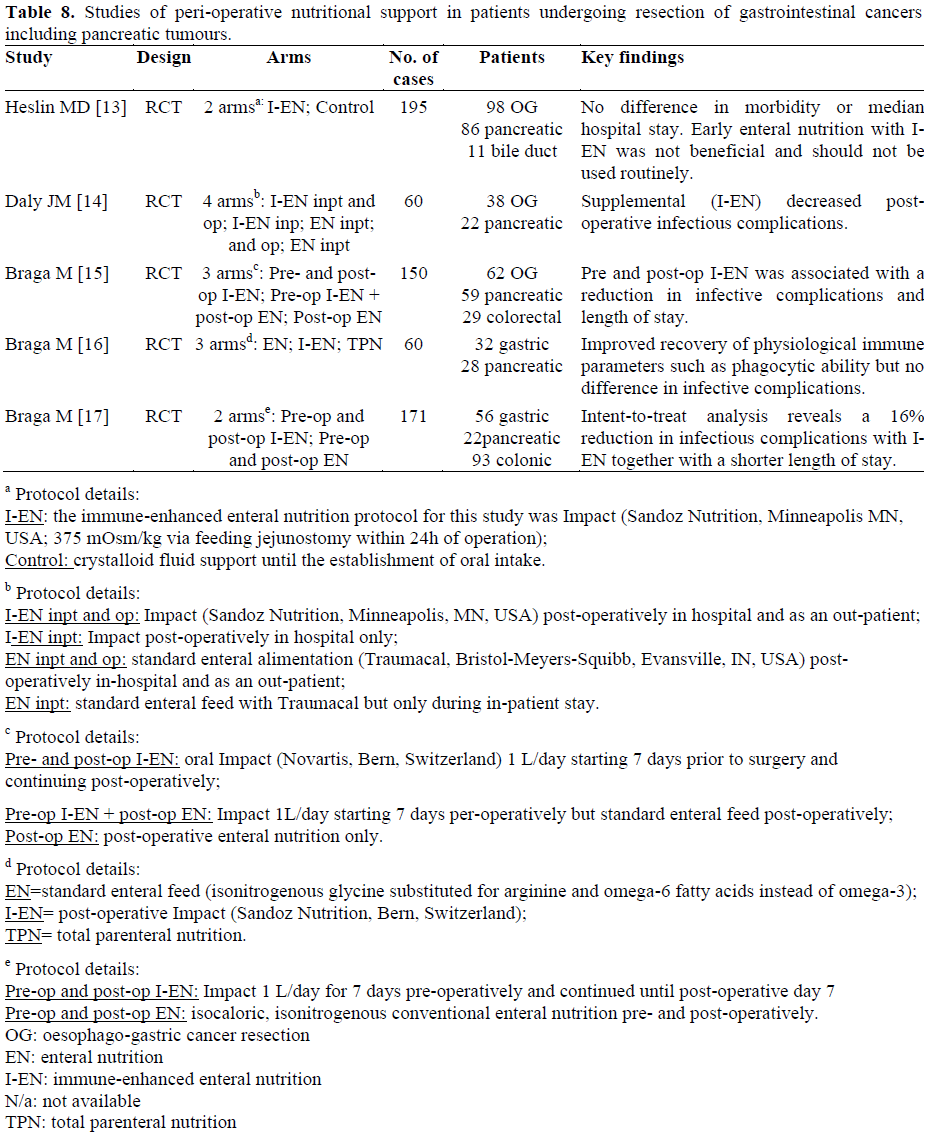
Studies of Peri-Operative Nutritional Support in Patients Undergoing Resection of Gastrointestinal Cancers Including Pancreatic Tumours
The 5 studies we found are listed in Table 8; all are randomised trials of nutritional support in patients undergoing gastrointestinal cancer resection. Of the 671 patients randomized, 217 (32.3%) underwent pancreatic cancer resection. None of these studies provide outcome data categorised by type of operative procedure.
Cyclical vs. Non-Cyclical Enteral Nutrition
The last study is a randomised controlled trial by the group of Obertop and Gouma [18]. This study compared continuous postoperative enteral nutrition delivered via a needle catheter jejunostomy in 30 patients undergoing pancreaticoduodenectomy to cyclical post-operative enteral nutrition in 27 pancreaticoduodenectomy patients where post-operative feed was delivered for 18 h with a 6 h non-feeding window from midnight to 06:00 a.m. There was no significant difference in the number of days of nasogastric intubation (P=0.82) but the mean number of days to resumption of normal diet was significantly (P=0.04) shorter in patients receiving cyclical enteral nutrition than in the continuous group (12.2 vs. 15.7). Cholecystokinin levels were lower in patients receiving cyclical nutritional support: in cyclical patients, fasting plasma cholecystokinin levels were 1.7±0.3 pmol/L and after starting the enteral nutrition they increased significantly in these patients (P=0.02). In continuous patients, cholecystokinin levels did not change during testing (P=0.99).
This systematic review has examined studies of peri-operative nutritional support in patients undergoing pancreaticoduodenectomy. The central issue in interpreting the findings is whether the data add substantially to the findings of the individual studies viewed in isolation. Formal pooled analysis is unfeasible and likely to be misleading given the wide disparity in study protocols, healthcare settings and study time periods in these reports. Nonetheless, careful analysis of the studies yields findings of interest. The four studies in patients undergoing pancreaticoduodenectomy show that in all reports, the proportion of pre-operative weight loss was similar. Given that all these patients underwent the same operative procedure, this finding provides a sense that the patient groups were not widely disparate in terms of their pre-operative nutritional status. Similar findings are obtained from comparison of pre-operative albumin levels and analysis of the number of jaundiced patients.
Brennan’s study although relatively small can be regarded as providing definitive evidence that routine post-operative parenteral nutrition is not associated with any improvement in outcome in this population [10].
In the context of enteral nutrition, the study by Martignoni et al. reports a more prolonged requirement for nasogastric intubation in patients receiving post-operative jejunal feeding as compared to controls not receiving enteral feed (15.1 days as compared to 3.4 days; P<0.01) [9]. Of 30 patients receiving enteral nutrition, 17 (56.7%) had delayed gastric emptying compared to 5 (15.6%) of 32 non-fed controls. This translated into increased hospital stay in patients receiving routine enteral nutrition. Martignoni et al. do not provide information on the composition of feed or whether cyclical feeding was employed.
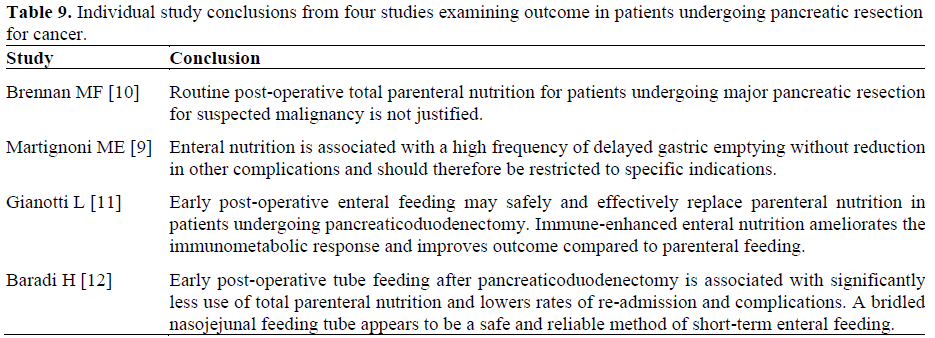
The findings of Gianotti’s [11] study support those of Brennan’s [10] in that TPN was associated with a greater risk of postoperative morbidity. They did not demonstrate a major clinical benefit from the use of immune-enhanced enteral nutrition as compared to conventional feed. Baradi’s [12] study is the least valuable in terms of extrapolatable information. The data are analysed retrospectively and audit the practice of three different surgeons, one who used enteral feeding routinely, one who did not and one who used feeding tubes selectively. Clearly, almost all of the findings of their study could be attributed to observational bias associated with variations in surgeon performance. Additional guidance can be gained from the several studies which evaluate outcome in patients undergoing pancreatic cancer resection as part of cohorts undergoing gastrointestinal cancer resection (Table 9). The validity of pooling data from a technically disparate group of surgical procedures can be questioned - resumption of feeding after colonic resection seems likely to be predictably and consistently different from patterns of feeding after oesophagectomy or pancreaticoduodenectomy. Bearing this limitation in mind, the studies suggest that enteral nutrition in the post-operative period is associated with a lower incidence of infective complications. Although the data (Table 8) may have been further used to support immune-enhanced enteral nutrition, critical interpretation taking into account the lack of procedure-specific outcome data in patients undergoing pancreaticoduodenect- omy would be that the evidence for immuneenhanced feed as compared to conventional feed is small.
Synthesising this evidence into a practical management algorithm it is apparent that nutritional deficiency is relatively widespread pre-operatively. This appears to be a relatively constant finding and suggests that there are opportunities for optimisation of nutritional status prior to surgery. Commencement of nutritional support prior to surgery may provide additional benefit over post-operative supplementation alone and is borne out by the study of Braga et al. [17]. In the post-operative period there seems little evidence in favour of routine TPN in current practice. Although selection and definition of end-points varies, enteral nutrition is associated with a lower incidence of infective complications. The optimal route of delivery of enteral feeding is unestablished: nasojejunal feeding tubes may avoid the risks of surgical jejunostomy but can dislodge and can be a source of post-operative discomfort. Although the trial evaluating cyclical enteral feeding in comparison to continuous feeding is small and it remains to seen whether these results can be reproduced, the corollary physiologic evidence of persistent elevation of cholecystokinin in patients receiving continuous enteral nutrition tends to favour cyclical feeding. The evidence for immuneenhanced feed in patients undergoing pancreaticoduodenectomy is limited. Although individual trial numbers are small, the studies appraised here evaluate in excess of 1,300 patients suggesting that a reasonable evidence base exists for guidance of nutritional support in patients undergoing pancreaticoduodenectomy. The conclusions of this study are that in patients undergoing pancreaticoduodenectomy attention should be paid to pre-operative nutritional optimisation, nutritional support should be delivered in the post-operative period with cyclical enteral nutrition being the current standard of care.