Research Article - (2024) Volume 9, Issue 1
The Accuracy of Readability Formulas in Health Content: A Systematic Review
Brittany U. Carter1*,
Kinjalbahen Nayak2 and
Isabella Vembenil3
1Department of Health and Research, Wellsource, United States
2Department of Public Health, Kent State University, United States
3The Ursuline School, United States
*Correspondence:
Brittany U. Carter,
Department of Health and Research, Wellsource,
United States,
Email:
Received: 05-Feb-2024, Manuscript No. IPJHCC-24-19014;
Editor assigned: 07-Feb-2024, Pre QC No. IPJHCC-24-19014 (PQ);
Reviewed: 21-Feb-2024, QC No. IPJHCC-24-19014;
Revised: 26-Feb-2024, Manuscript No. IPJHCC-24-19014 (R);
Published:
04-Mar-2024, DOI: 10.36846/2472-1654-9.1.9002
Abstract
Background: Readability formulas are commonly used to assess the ease in which a reader can understand written text. It is unclear which is best to use when evaluating the readability of health content. This systematic review assessed the accuracy of readability formulas when evaluating health content targeting adults.
Methods: Searches of PubMed, Cochrane Library, and Education Resources Information Center from inception through January 31, 2024 were conducted. Two investigators independently reviewed abstracts and full-text articles against a set of a priori inclusion criteria. Studies evaluating the accuracy or validity of readability formulas when
applied to health content for adults were included. Data was analyzed qualitatively.
Results: Three fair-quality studies were included. One study found readability formulas frequently underestimated the document’s difficulty when compared to expert panel ratings. Another study found very low correlations between the readability formulas and user difficulty ratings. Another study found readability formulas were unable
to consistently identify problematic health survey questions among question pairs.
Conclusion: Evidence is limited regarding the accuracy of readability formulas for health content. Study limitations and those associated with the readability formulas likely contributed to the poor performance. More studies are needed to determine which is best to use for health content.
Keywords
Health literacy; Readability formulas; Health content
Introduction
According to the National Assessment of Adult Literacy, 88%
of U.S. adults are not proficient in health literacy [1], that is,
the degree to which they have the capacity to obtain, process,
and understand basic health information and services needed
to make appropriate health decisions [2]. Low health literacy is
associated with negative health outcomes including increased
hospitalizations, poor medication adherence, and higher
mortality rates [3,4]. The ease in which a reader can understand
written text-or readability-is a contributing factor to health
literacy as it affects the reader's ability to comprehend the
content. The Centers for Disease Control and Prevention (CDC)
and National Institutes of Health (NIH) recommend, and the
Centers for Medicare and Medicaid Services (CMS) requires
for its members, that health materials be written at a reading
level no higher than an 8th grade, while the American Medical
Association (AMA) recommends patient-facing material be
written at a 6th grade reading level.
Readability can be determined by using various formulas
such as the Flesch Reading Ease (FRE), Flesch-Kincaid Grade
Level (FKGL) index, and the Simple Measure of Gobbledygook
(SMOG) index. However, there are concerns, criticisms, and
limitations regarding the use and accuracy of these readability
formulas in general as well as when assessing health content
[5-9]. For example, although the government agencies and medical associations provide or suggest a threshold at which
content should not pass (i.e., a 6th or 8th grade reading level),
studies have shown that the readability formulas when used
for health content largely disagree by up to 5 reading grade
levels on the same text [10]. This may be the result of the
formulas using different components as well as not being
designed, intended, or appropriate for use in evaluating health
content. These issues with the readability formulas can lead to
confusion as to which is best to use to assess the readability
of health content to maximize health literacy. It also results in
spending unnecessary resources to revise health content that
might otherwise not need to be modified. There is currently no
guidance as to which formula should be used in health content.
The aim of this systematic review was to evaluate the evidence
on the accuracy of readability formulas when assessing health
content targeting adults to inform which to use.
Materials and Methods
Scope of the Review
This systematic review addressed the key question: What is
the accuracy of readability formulas when evaluating health
content directed towards adults? This systematic review is not
registered.
Data Sources and Searches
Comprehensive literature searches were performed in
PubMed, Education Resources Information Center (ERIC), and
the Cochrane Library from inception through January 31, 2024.
The literature search strategies were developed by one of the
investigators and are available in Appendix A. The database
searches were supplemented by reviewing the reference lists
from relevant studies and background articles. All references
were managed using EndNoteTM version 19 (Thomson Reuters,
New York, NY).
Study Selection
Two investigators independently reviewed titles and abstracts
using an online platform (Rayyan®, Rayyan Systems, Inc), and
subsequently, full-text articles against pre-specified inclusion
and exclusion criteria (Appendix B). Disagreements were
resolved through discussion and when necessary, consultation
with a third investigator.
Studies published in the English language that assessed the
validity or accuracy of readability formulas in the evaluation of
written health content directed towards an adult population
(i.e., ages 18 years or older) were included. There were no
limitations on the topic of the health content (e.g., nutrition,
diabetes), the source used to deliver the written health content
(e.g., website, brochure, medical journal), or the setting in
which the health content was provided (e.g., healthcare
organization, university-based). Studies that evaluated content
that was unrelated to health, or any content that was directed
towards children and/or adolescents (i.e., ages less than 18
years) were excluded. There were also no limitations on the
study design or publication type.
Readability formulas are those that assess the ease with
which a reader can understand written text and are typically
reported as a grade level or a score that is translatable to a
grade level equivalent to the U.S. education system. Only
the following readability formulas were included as they are
the most frequently used in health [10]: FRE, FKGL, SMOG,
Dale-Chall, Spache, FORCAST, Fry Graph, Rate Index (RIX),
Automated Readability Index (ARI), Gunning-Fox Index, and the
Coleman-Liau Index. Readability formulas specifically designed
to measure the readability of tables, charts, or graphs (e.g.,
Suitability Assessment of Materials [SAM]) were excluded.
Formulas used to measure comprehensiveness of the content,
reading comprehension (e.g., Cloze test), suitability or quality of
the content, or to estimate health literacy (e.g., Rapid Estimate
of Adult Literacy in Medicine [REALM]) were excluded.
Studies were included if the comparator group with whom
to compare the results of the readability formulas) were
standard health textbooks at a specific grade-level or a panel
of individuals rating the content. Studies that compared the
grade levels between readability formulas were excluded, as
were studies that compared the readability of the content
to the state or national average grade level or to the content
developer's stated readability level.
Studies were included if they reported on the validity or
accuracy of the readability formulas through correlations or
measures of accuracy (e.g., sensitivity). Studies that reported
on the agreement between two or more readability formulas
were excluded.
Quality Assessment and Data Abstraction
Quality assessment of the included studies using an existing
validated tool, such as those used for diagnostic accuracy or
specific observational study designs [11,12], was not performed
as these tools did not met the needs of this systematic review.
In lieu of formal quality assessment, two investigators discussed
the limitations of each study and reached consensus on a final
quality rating of good, fair, or poor. Such study limitations
included the sample size, the depth and breadth of health
content evaluated including its selection, the comparator used,
the approach to the analysis, and generalizability. Fair-quality
studies often had minor flaws while a poor-quality study had
significant design flaws that seriously called into question the
validity of the study results, and thus, poor quality studies were
excluded.
One investigator abstracted data from all included studies and
a second investigator checked the data for accuracy. Abstracted
data included information on the study design, descriptions of
the health content, the readability formulas evaluated, the
comparator used, validity and/or accuracy outcomes, and
study limitations.
Data Synthesis and Analysis
Results from included studies are summarized qualitatively as
there were too few studies and not enough data to allow for
meta-analysis.
Results
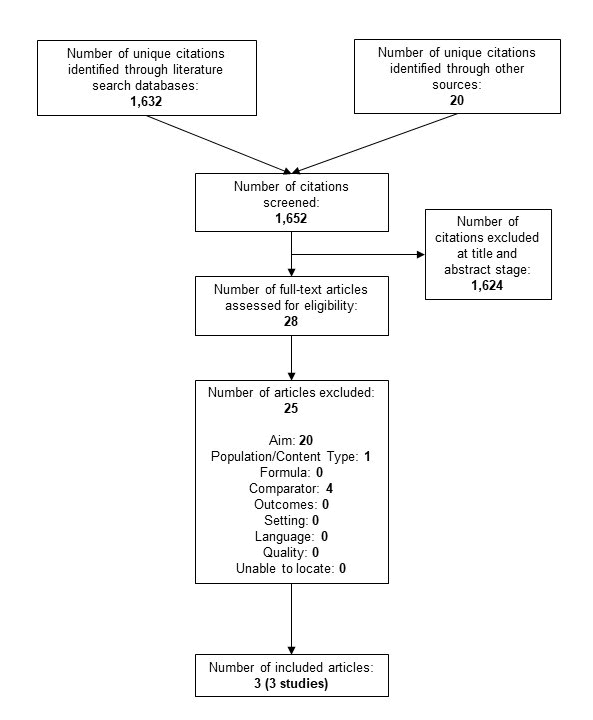
A total of 1,652 unique citations and 28 full-text articles were reviewed (Figure 1). Three fair-quality studies met the inclusion criteria; a list of excluded studies at full-text is available in Appendix C [13-15]. In summary, two of the studies assessed the readability of diabetes content while the other assessed health survey questions (Table 1). The accuracy of FKGL was evaluated in three studies; SMOG and Gunning Fog Index were evaluated in two studies; and Dale-Chall and FRE were evaluated in one study each. No other readability formulas were evaluated in the studies. The comparator group of two studies consisted of a panel of individuals who assessed the ease or difficulty of the content while the other was designed to identify the problematic question of a question pair. All three studies found the readability formulas to not perform well. Further information about each of the included studies can be found below.
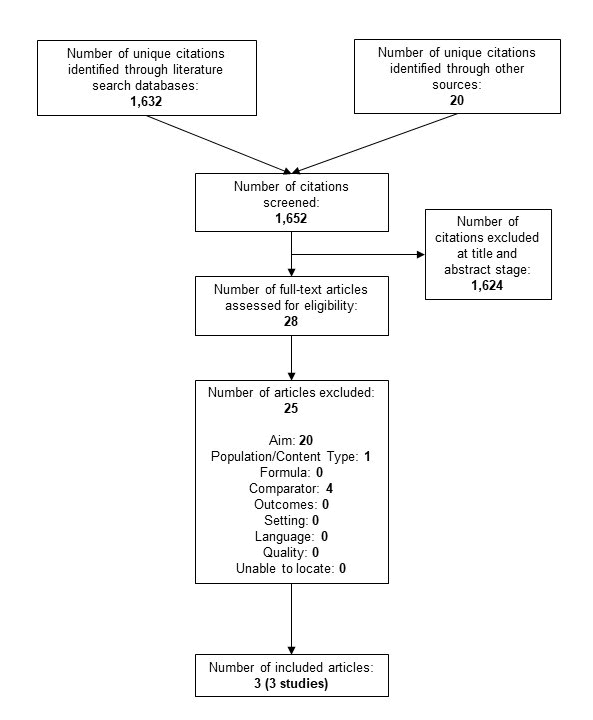
Figure 1: Literature flow diagram
Table 1: Characteristics of included studies
| Study |
Brief Methods |
Health Content |
Readability Formula(s) |
Comparator |
Quality |
| Kandula, 2008 [14] |
324 diabetes-related documents manually reviewed by an expert panel to assign a readability score which was compared to the FKGL and SMOG scores |
Diabetes mellitus consumer education materials (k=142), news stories (k=34), clinical trial records (k=39), clinical reports (k=38), scientific journal articles (k=38), consumer education materials for children (n=33) |
FKGL SMOG |
Expert panel (n=5) developed Likert scale (1-7)* to assess ease of reading material |
Fair |
| Lenzner, 2014 [15] |
Readability scores calculated for 71 pairs of health survey questions (one difficult and one improved) to determine if formulas correctly classified them as being more or less difficult |
Health survey question pairs as published in journal articles or textbooks (k=15), or in the Q-Bank database (k=56) |
FKGL FRE Gunning Fog Dale-Chall |
Problematic survey question (e.g., syntactically complex) |
Fair |
| Zheng, 2017 [13] |
Readability scores of 382 diabetes-related documents compared to laypeople's perceived difficulty of the content |
General health information on diabetes (Wikipedia articles; k=140) and electronic health records notes with diabetes ICD-10 codes (k=242) |
FKGL SMOG Gunning-Fog |
Laypeople's (n=15) perceived difficulty level of the content on a Likert scale (1-10) |
Fair |
FKGL=Flesch-Kincaid Grade Level; FRE=Flesch Reading Ease; ICD-10=International Classification of Disease 10th edition; SMOG=Simple Measure of Gobbledygook
*Lower rating indicates lower education level: 1=any; 3=high school graduate (12th); 4=some college; and 7=professional education only Lower rating indicates easiest to understand with highest score indicating the most difficult to understand |
One fair-quality study used a panel of five health literacy and clinical experts to assess the readability of 324 documents on diabetes in comparison to two readability formulas (FKGL and SMOG) [14]. The documents included consumer education materials (k=142), news reports (k=34), clinical trial records (k=39), scientific journal articles (k=38), and clinical reports (k=38); 33 documents targeted children and are not discussed further. The expert panel developed a “gold standard” using a Likert scale (1-7) to assess the ease of the reading materials with lower scores indicating lower education levels required to understand the content. The “gold standard” had good interrater reliability and validity (data not shown). Across all documents (including those directed at children), the grades assigned by FKGL and SMOG had a Spearman's correlation coefficient of 0.54 and 0.55, respectively, with the expert ratings; both were statistically significant moderately strong correlations (p<0.0001) (Table 2). When evaluated by document type, the only significant difference between the expert ratings and the two readability formulas were the clinical reports with the latter demonstrating the content to be understandable at a lower grade level. The formulas frequently underestimated the document's difficulty across all document types when compared to the expert panel ratings. Limitations of this study include using a non-validated “gold standard” which relied on the use of expert knowledge as opposed to lay persons, having a small sample size of the experts providing the ratings, evaluating a few content sources where health information is delivered, and covering only one health topic.
Table 2: Correlations of Readability Formulas
| Study |
Document Type |
Formula |
Mean (SD) |
Correlation |
| Kandula, 2008 [14] |
All (k=324)* |
FKGL |
NR |
0.54 (p<0.0001) |
| SMOG |
NR |
0.55 (p<0.0001) |
| News report (k=34) |
FKGL |
11.29 (2.22) |
NR |
| SMOG |
13.68 (1.80) |
| Expert Panel |
4.26 (0.86) |
| Consumer education material (k=142) |
FKGL |
10.19 (2.05) |
NR |
| SMOG |
12.62 (1.69) |
| Expert Panel |
4.02 (1.18) |
| Clinical trial record (k=39) |
FKGL |
15.71 (2.37) |
NR |
| SMOG |
17.10 (1.93) |
| Expert Panel |
6.33 (0.89) |
| Scientific journal article (k=38) |
FKGL |
15.82 (1.43) |
NR |
| SMOG |
17.24 (1.07) |
| Expert Panel |
6.55 (0.72) |
| Clinical report (k=38) |
FKGL |
8.38 (1.78) |
Significant difference between expert panel and FKGL/SMOG (p-value NR) |
| SMOG |
11.36 (1.44) |
| Expert Panel |
6.13 (0.84) |
| Zheng, 2017 [13] |
Wikipedia articles (k=140) |
FKGL |
14.75 |
0.1758 |
| SMOG |
11.07 |
0.4134 |
| Gunning Fog |
12.33 |
0.2695 |
| User Rating |
4.41 |
- |
| EHR (k=242) |
FKGL |
9.87 |
0.2999 |
| SMOG |
8.74 |
0.1024 |
| Gunning Fog |
8.16 |
0.1272 |
| User Rating |
5.35 |
- |
EHR=electronic health record; FKGL=Flesch-Kincaid Grade Level; FRE=Flesch Reading Ease; NR=not reported; SD=standard deviation; SMOG=Simple Measure of Gobbledygook
*Includes the 33 documents directed towards children Lower rating indicates lower education level: 1=elementary school; 3=high school graduate (12th); 4=some college; and 7=professional education only Lower rating indicates easiest to understand with highest score indicating the most difficult to understand |
Another fair-quality study also compared the readability of three formulas (FKGL, SMOG, and Gunning Fog) against a difficulty rating as perceived by 15 Amazon Mechanical Turk users (Table 1) [13]. The Amazon Mechanical Turks had English as their primary language and were master workers; three had high school diplomas, 7 had an associate degree, four had a Bachelor's degree, and one did not report their education level. 140 Wikipedia articles containing general health information on diabetes and 242 de-identified Electronic Health Record (EHR) notes with diabetes codes (International Classification of Diseases 10th edition codes 250.00 to 250.93) were evaluated. Each user measured the level of difficulty of 20 randomly assigned paired analogous documents using a Likert scale (1- 10) with lower scores indicating the easiest to understand. The readability formulas suggested the EHR notes to be significantly easier than the Wikipedia articles while the user ratings showed the opposite (Table 2). All correlations were very low between the user ratings and readability formulas suggesting the users' perceived difficulty and the readability formulas predictions were inconsistent (Table 2). Limitations of this study include using a non-validated Likert scale, having a small sample size of lay persons provide ratings in a population that may not be generalizable to the United States [16], evaluating only two content sources where health information is delivered, and covering only one health topic.
The final fair-quality study evaluated whether four readability formulas (FRE, FKGL, Gunning Fog Index, and Dale-Chall) correctly identified the problematic survey question from 71 question pairs each containing a problematic question and an improved version of the same question (Table 1) [15]. Problematic questions were described as syntactically complex or vague. An example of a problematic question was “Have you ever had a Pap test to check for cervical cancer?” while the improved question was “Have you ever had a Pap smear or Pap test?” The question pairs came from two sources: Journal articles or textbooks, and the Q-Bank database. The literature sources addressed questionnaire design and included examples of problematic survey questions together with recommendations for improving them; 15 pairs were reported in five publications. The Q-Bank database provides access to question evaluation research and contains pretested and improved survey questions. 56 questions originally identified having “problematic terms” (k=34) or were “overly complex” (k=22) were included with their improved version. The FRE and FKGL formulas performed better than the Gunning Fog Index and Dale-Chall formulas (Table 3), however, all showed low classification accuracy (less than 52%). Binomial testing showed none of the formulas performed significantly better than expected from random guessing, in fact, three of the formulas (FKGL, Gunning Fog Index, and Dale-Chall) performed worse than by chance alone (data not shown). When analyses were limited to from where the questions pair came, the classification accuracy was considerably better for questions from the Q-Bank database than from the literature (Table 3). Limitations of this study include relying on an assumption that the pairs contained one problematic and one improved question as they were not tested.
Table 3: Success Rates of Readability Formulas Correctly Classifying Question Pairs [15]
| Health Survey Questions |
Readability Formula |
Success Rate |
P-value |
| All (k=71) |
FRE |
51% |
1 |
| FKGL |
49% |
1 |
| Gunning Fog |
39% |
0.1 |
| Dale-Chall |
38% |
0.06 |
| From journal articles or textbooks (k=15) |
FRE |
27% |
0.12 |
| FKGL |
27% |
0.12 |
| Gunning Fog |
27% |
0.12 |
| Dale-Chall |
27% |
0.12 |
| From Q-Bank database (k=56) |
FRE |
57% |
0.35 |
| FKGL |
55% |
0.5 |
| Gunning Fog |
43% |
0.35 |
| Dale-Chall |
41% |
0.23 |
| From Q-Bank database and tagged as having a “problematic term” (k=34) |
FRE |
53% |
0.86 |
| FKGL |
50% |
1 |
| Gunning Fog |
44% |
0.61 |
| Dale-Chall |
44% |
0.61 |
| From Q-Bank database and tagged as being “overly complex” (k=22) |
FRE |
64% |
0.29 |
| FKGL |
64% |
0.29 |
| Gunning Fog |
41% |
0.52 |
| Dale-Chall |
36% |
0.29 |
| EHR=electronic health record; FKGL=Flesch-Kincaid Grade Level; FRE=Flesch Reading Ease; NR=not reported; SD=Standard deviation; SMOG=Simple Measure of Gobbledygook |
Discussion
Only three studies assessing the accuracy of readability formulas
when evaluating health content were identified and only a few
of the readability formulas were evaluated in these studies. The
studies show that the readability formulas did not correlate
well with panel ratings or accurately identify problematic
health survey questions [13-15]. There are too few studies to
make any definitive conclusions on the accuracy of readability
formulas when assessing health content directed towards
adults. And there is a multitude of reasons that the readability
formulas performed poorly, albeit in the few included studies
in this systematic review, including study design limitations
and some of the previously mentioned preexisting concerns,
criticisms, and limitations of using readability formulas to
assess health content.
First, readability formulas were not created with health
content in mind. These formulas were invented in the late
19th and early 20th centuries to assess the comprehensibility
of general educational literature for children and adults-not
health literature [17]. The developers used written text from
school textbooks, newspapers, and magazines-not healthrelated
sources-to identify components that would predict
comprehension or assess reading difficulty. Components of
formulas identified as the best to determine readability and
used in the equations include the length of words, the length
of sentences, and/or the frequency of “hard words”. Health
content, however, often contains polysyllabic words, scientific
terminology, and medical abbreviations which results in it
being assessed at a higher grade level. The components or
coefficients of the readability formulas might differ if health
content were used in their development. In fact, recent studies
have shown different elements such as syntax and semantics
to be more important when assessing health content than
the components used in existing readability formulas [18,19].
Although one adult reading ease formula used passages
on health topics from various sources to identify factors
influencing the difficulty of reading level among adults with
limited reading ability, and used three factors in the formula, it
was not included in this review as it is not commonly used [20].
Second, the readability formulas also did not use health
content in their validation. The McCall-Crabbs Standard Test
Lessons in Reading (for children), the Cloze test, or other similar
types of texts were used for validation-not health content [17].
Although the predictions of the Dale-Chall readability formula
across 55 passages of health education materials were highly
correlated with the judgments of readability experts [17];
there was no further information regarding this statement or
validation study from the 1940's and thus not included in this
review. Validating the readability formulas with health content
may contribute to refinements in the equations when applied
to this specific type of content.
Third, the assumptions of the readability formulas also do
not hold true with regards to health content. According to
the formulas, a word or sentence is harder if it is longer.
As mentioned previously, health content tends to include
polysyllabic words such as diabetes and hypertension which
decreases readability. Attempts to improve the readability,
however, such as substituting polysyllabic words with multiple
smaller words (e.g., hypertension to high blood pressure) make
it less readable per the formulas because sentence length
increases. In addition, readability formulas do not consider if
the words are familiar or the sentences are clear and cohesive
[6]. Many health terms and abbreviations-such as cholesterol
and HIV-are common to lay audiences, however, including these
words or abbreviations makes the health content less readable
per the formulas. And adding more words to explain these
health terms more simply again counts against readability.
And finally, the source from which the health content is provided
may further contribute to issues with using these formulas
to assess readability. These readability formulas assume
content is delivered in well written paragraphs with complete
sentences of at least 100 words. A patient's EHR, however, may
contain lists of clinical events, drug names, tests results with
numbers and measurement units, medical abbreviations, and
short and incomplete sentences, thus lowering the readability
[13]. It is possible that the health content used in the included
studies may not have met the minimum requirements for the
readability formulas to accurately work thus contributing to
the poor performance of the formulas. For example, the Dale-
Chall formula requires at least a 100-word sample of text while
FORCAST requires a 150-word sample [21]. When it comes
to health survey questions, for example, most are less than
100 words and thus no readability formula may be suited for
their assessment. Given the uncertainty that adequate health
content was used in the included studies contributes to the lack
of a definitive conclusion on the readability formulas accuracy.
It is not possible to definitively conclude that health content
might not be a good fit for the readability formulas without
further good quality studies.
The results of this systematic review do not suggest that the
readability formulas are useless or that the limited evidence
suggests they should not be used as there must be a starting place
for ensuring lay audiences understands health information.
For example, one could use these formulas to estimate the
ceiling of the content's readability and subsequently edit the
content as needed. In addition, previous studies have shown
that readability formulas are valid and reliable with other
types of content such as fiction and non-fiction literature,
general education textbooks, and governmental websites
[17,21,22]. The choice of formula can have a strong influence
on the conclusions drawn from readability and there is minimal
guidance on which to use to assess health content. As mentioned
previously, readability of the same health content can differ by
up to five reading levels per the formulas [10]. One readability
formula-SMOG-has been endorsed for use in healthcare as it
is the only formula based on complete comprehension of the
content meaning all individuals who read the content also
understand it [10,21,23]. Such high comprehension is very
important in healthcare to ensure individuals experience safe
and effective outcomes. Expecting such high comprehension,
however, means SMOG scores are often 1-2 grades higher than
the results of other readability formulas [24] so more effort
may be needed to bring the grade level down. There are lots
of tools and suggestions on how to improve readability when
one's health content is grading too high such as the Agency for
Healthcare Research and Quality's Health Literacy Toolkit [25]
or the Centers for Medicare and Medicaid Services Guidelines for Effective Writing and Plain Language [26,27].
Implications of the Findings for Health
Communication Research and Practice
The greatest implication of these findings on health
communication research and practice is there is no universally
recommended formula for content developers to use that
has proven validity and reliability in assessing the readability
of health content. Every effort made to help improve health
literacy (and subsequently health outcomes) by attempting
to optimize this one aspect (i.e., readability) may be thwarted
because the output from readability formulas may be incorrect.
Health communication research should conduct future studies
to determine which readability formula is best to use for health
content either by validating and/or refining existing formulas
or creating a de novo one. These future studies should also
consider the source of the health content as written text
in EHRs may differ from that provided on a drug label or a
website about diabetes care-all of which may be read by a
lay person. With regards to health communication practice,
health content developers should continue to strive to ensure
optimal readability by following proven guidance to ensure the
reader can read, process, and understand the content. The use
of readability formulas-although at risk of an inaccurate grade
level being reported-can still occur as a starting point to see
what content may require improvement to warrant maximum
comprehension.
Limitations Of The Systematic Review
There are a few limitations of this review. First, the literature
search was not developed nor reviewed by a research librarian
and only three databases were searched; both of which may
have resulted in the searches missing relevant studies. The
literature search also did not include terms for online readability
calculators (e.g., readable.com) that use the underlying
included readability formulas which may have also missed
relevant studies. This limitation was mitigated by checking
references of relevant studies and background articles to
ensure none were missed. Second, some readability formulas
were omitted such as the Golub Syntactic Density Score,
Linsear Write, and the Lexile framework. These omissions were
not concerning as the most prevalent readability formulas used
in health were in the literature search strategies [10]. Targeted
searches for studies on the omitted formulas also resulted in
few-to-none being found and thus the literature searches were
not modified from the initial search. Third, there is no universal
gold standard [10] and thus it was defined in this review as
either a panel of individuals assessing the content's difficulty
to read or understand the materials or standard health text
at a specified grade reading level. A more broadly defined
comparator may have resulted in additional included studies.
Fourth, no formal quality assessment was conducted; however,
the investigators considered the limitations of the studies to
ensure none had any significant flaws that called into question
the validity of the results which should be sufficient to have
trust in the conclusions of this review. And finally, most of the
initial validity and reliability studies of the readability formulas
were excluded as they were validated among children; used
content targeted towards children, or used content that was
not related to health.
Conclusion
Limited evidence contributes to the concerns, criticisms, and
limitations of using existing formulas to assess the readability
of health content. In lieu of having a better alternative, using
existing readability formulas (especially SMOG) is a start to
ensuring improved health literacy and subsequently health
outcomes.
Acknowledgement
None.
Competing Interests Statement
BUC was employed by Wellsource, a company who develops
health content. KN and IV worked on this project as student
interns of Wellsource.
Funding Statement
None.
References
- Lopez C, Kim B, Sacks K (2022) Health literacy in the United States: Enhancing assessments and reducing disparities. Santa Monica, CA: Milken Institute.
[Crossref] [Google Scholar]
- Ratzan SC, Parker RM (2000) Introduction in: Selden CR, Zorn M, Ratzan SC and Parker RM, eds. Health Literacy.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K (2011) Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 155(2):97-107.
[Crossref] [Google Scholar]
- Fan ZY, Yang Y and Zhang F (2021) Association between health literacy and mortality: A systematic review and meta-analysis. Arch Public Health 79(1):119.
[Crossref] [Google Scholar]
- U.S. Department of Health and Human Services (2010) Using readability formulas: A cautionary note.
- Agency for Healthcare Research and Quality (2015) Tip 6. Use caution with readability formulas for quality reports.
- Redish G (2000) How valid are readability formulas for technical material for adult readers? J Com Doc. 24:132-137.
- Pichert JW, Elam P (1985) Readability formulas may mislead you. Patient Educ Couns. 17(2):181-191.
[Crossref] [Google Scholar]
- Danielson KE (1987) Readability formulas: A necessary evil? Reading Horizons: A Journal of Literacy and Language Arts. 27:178-88.
[Google Scholar]
- Wang LW, Miller M, Schmitt M, Wen F (2013) Assessing readability formula differences with written health informaiton materials: Application, results, and recommendations. Res Social Adm Pharm. 9(5):503-516.
[Crossref] [Google Scholar]
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, et al. (2011) QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 155(8):529-536.
[Crossref] [Google Scholar]
- Wells GA, Shea B, O'Connell D, Robertson J, Peterson J, et al. (2021) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: The Ottawa Hospital Research Institute.
[Google Scholar]
- Zheng J, Yu H (2017) Readability formulas and user perceptions of electronic health records difficulty: A corpus study. J Med Internet Res. 19(3):e59.
[Crossref] [Google Scholar]
- Kandula S, Zeng-Treitler Q (2008) Creating a gold standard for the readability measurement of health texts. AMIA Annu Symp Proc. 2008:353-357.
[Google Scholar]
- Lenzner T (2014) Are readability formulas valid tools for assessing survey question difficulty? Sociol Methods Res. 43(4):677-698.
[Crossref] [Google Scholar]
- Mortensen K, Hughes TL (2018) Comparing Amazon's mechanical turk platform to conventional data collection methods in the health and medical research literature. J Gen Intern Med. 33(4):533-538.
[Crossref] [Google Scholar]
- DuBay WH (2006) The classic readability studies. Costa Mesa, CA: Impact Information.
- Rosemblat G, Logan R, Tse T, Graham L (2006) Text features and readability: Expert evaluation of consume health text.
[Google Scholar]
- Treitler QZ, Kim H, Goryachev S, Keselman A, Slaughter L, et al. (2007) Text characteristics of clinical reports and their implications for the readability of personal health records. Stud Health Technol Inform. 129:1117-21.
[Google Scholar]
- Dale E, Tyler RW (1934) A study of factors influencing the difficulty of reading materials for adults of limited reading ability. The Library Quarterly. 4(3):384-412.
[Crossref] [Google Scholar]
- Burke V, Greenberg D (2010) Determining readability: How to select and apply easy-to-use readability formulas to assess the difficulty of adult literacy materials. Adult Basic Edu Literacy Journ. 4(1):34-42.
[Google Scholar]
- Ley P, Florio T (1996) The use of readability formulas in healthcare. Psych Health Med. 1(1):7-28.
[Crossref] [Google Scholar]
- Friedman DB, Goetz HL (2006) A systematic review of readability and comprehension instruments used for print and web-based cancer information. Health Educ Behav. 33(3):352-373.
[Crossref] [Google Scholar]
- Badarudeen S, Sabharwal S (2010) Assessing readability of patient education materials: Current role in orthopaedics. Clin Orthop Relat Res. 468(2):2572-2580.
[Crossref] [Google Scholar]
- Brega AG, Cifuentes M, Barnard J, Mabachi NM, Albright K, et al. (2015) Guide to implementing the health literacy universal precautions toolkit. Agency for healthcare research and quality.
[Google Scholar]
- Centers for Medicare and Medicaid Services (2023) Guidelines for effective writing.
- Plain Language Action and Information Network (2011) Federal plain language guidelines.
Citation: Carter BU, Nayak K, Vembenil I (2024) The Accuracy of Readability Formulas in Health Content: A Systematic Review. J Healthc Commun. 9:9002.
Copyright: © 2024 Carter BU, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.