Review Article - (2018) Volume 0, Issue 0
1Department of Hepatobiliary and Pancreatic Oncology, Nationcal Cancer Center Hospital, Tokyo, Japan
2Department of Gastroenterology, Aichi Cancer Center Hospital, Aichi, Japan
3Department of Pathology, The Sol Goldman Pancreatic Cancer Research Center, The Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Received Date: July 19th, 2017; Accepted Date: October 31st, 2017
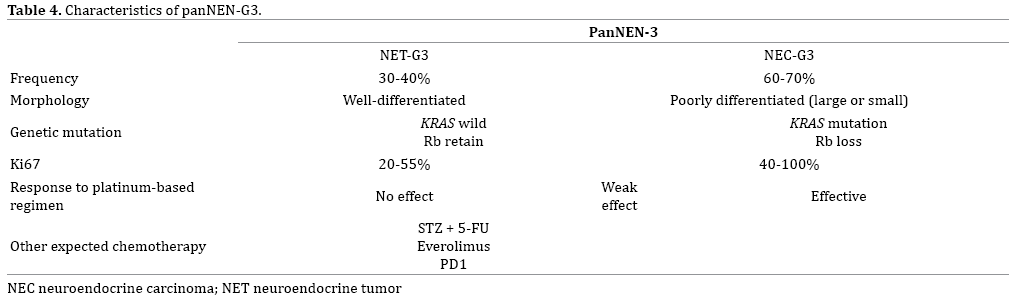
Pancreatic neuroendocrine carcinoma (panNEC; pancreatic neuroendocrine neoplasm NEN-G3) is expected to be divided into neuroendocrine tumor-G3 and neuroendocrine carcinoma-G3 in the World Health Organization 2017 classification of tumors of endocrine organs. The distinction is clinically important because the response to chemotherapy differs between the two. Evidence is accumulating on the molecular features of NET-G3, which supports the view that NET-G3 is more closely related to well-differentiated NET. Several molecular markers can be useful in predicting the effectiveness of platinum-based chemotherapies, including high Ki67 labeling index, loss of Rb expression, or KRAS mutation. However, appropriate chemotherapy for NET-G3 remains unclear. Appropriate classification of NET-G3/NEC-G3 and the adequacy of standard treatments depending on this classification are expected in the future with the accumulation of further cases.
Carcinoma, Islet Cell; Neuroendocrine Tumors
NEC neuroendocrine carcinoma; NET neuroendocrine tumor; panNEC pancreatic neuroendocrine carcinoma
According to the World Health Organization (WHO) 2010 classification of tumors of the digestive system, pancreatic neuroendocrine neoplasm (panNEN) is classified into NET-G1, NET-G2, or neuroendocrine carcinoma (NEC) based on its proliferative activity evaluated by mitotic counts or Ki67 labeling index (LI) [1]. However, the category of pancreatic NEC (panNEC; equivalent to NEN-G3) has been shown by multiple studies to include two clinically and genetically different types of tumors, and the WHO 2017 classification of tumors of endocrine organs divided panNEC into neuroendocrine tumor (NET)-G3 and neuroendocrine carcinoma (NEC)-G3.
Although a number of studies have investigated the characteristics of the NET-G3 and NEC-G3 subgroups in terms of imaging, genetics, and treatment regimens, many points still remain unclear.
In this review, we refer to WHO2010-NEC as NEN-G3 and divide this into NET-G3 and NEC-G3 that will be incorporated into to the WHO 2017 classification. We review the clinical and genetic characteristics of pancreatic NEN-G3 and discuss appropriate medical therapies.
Problems with the WHO 2010 Classification
Ki67 is a powerful prognostic marker for panNEN [1] and a major revision was therefore made from the 2000 WHO classification system to the WHO 2010 terminology system, in which mitotic count and/or Ki67 LI were adopted as pivotal indicators of stratification [1]. The revised WHO classification 2010 [2] has since become the standard and has been widely applied. In this WHO classification, NENs with Ki67 LI >20% or mitotic index >20/10 high-power fields were categorized as neuroendocrine carcinoma (NEC).
However, in 2013, the first clinical report was made by a Nordic group indicating that gastroentero-pancreatic (GEP) NECs according to the 2010 WHO classification is clinically a heterogeneous category based on 305 patient records from hospital charts from 12 Nordic hospitals [3]. In their study, the group with Ki67 LI <55% showed lower response rate to platinum-based chemotherapy (15% vs. 42%; P<0.01), and longer overall survival (MST, 14 months vs. 10 months; P<0.01) compared with the Ki67LI ≥55% group. Although no detailed histological subclassification was performed in that study, it became the first paper to question the uniform application of platinum-based chemotherapy for NEC (WHO2010-NEC). Subsequent to that report, National Comprehensive Cancer Network (NCCN) guidelines provided a general recommendation in footnotes that NECs, with high Ki67 LI (>50%), be treated with small cell lung cancer regimens, such as cisplatin/ etoposide or carboplatin/etoposide. However, evolving data suggest that tumors with intermediate Ki67 levels in the range of 20-50% may not respond as well to platinum/ etoposide as those with small cell histology or extremely high Ki67, and clinical judgment should thus be used [4].
The French group of Velayoudom et al. [5] subsequently examined 28 cases of WHO2010-NEC including gastroenteropancreatic (GEP), lung and pharyngeal/ laryngeal tumors in 2014. They showed that NEC that was morphologically well differentiated and resembled NET G2, but with Ki67 LI >20%, could be termed as “G3-welldifferentiated NET (G3-WDNET; equivalent to the current NET-G3).” They reported that response to platinum-based chemotherapies and the prognosis of G3-WDNET differed greatly from G3 poorly differentiated NEC (G3-PDNEC; equivalent to current NEC-G3). After that report, the presence of NET-G3 attracted substantial attention, with some articles reported over the course of 4 years [5, 6, 7, 8, 9, 10, 11, 12, 13]. The frequency of panNET-G3 among panNEN-G3 was 30-49%, and the frequency of GEPNET- G3 among GEP-NEN-G3 was 18-42%. Although the selection bias due to study design should be considered, panNETs-G3 may not be rare in NENs-G3.
Clinical Differences between NET-G3 and NEC-G3 Differences
panNEC-G3 progresses rapidly, with frequent early metastasis to other organs. Although there have been a few reports of surgical resection as attempted curative therapy, in most cases the cancer has recurred and the prognosis is extremely poor. These clinical and pathological characteristics, as well as its sensitivity to chemotherapy, possess similarities to those of SCLC and NSNLC. The symptoms of panNEC-G3 are dependent on the presence of metastasis, and include not only local symptoms such as pain and jaundice but also cachexic symptoms similar to those seen in pancreatic carcinoma, including loss of appetite, malaise, and weight loss. NEC is non-functioning in almost all cases, and rarely exhibits hormonal symptoms [14]. NEC-G3 is also almost never found in combination with the MEN type 1 or VHL hereditary neoplastic syndromes. In contrast, cachexia is seldom evident in patients with panNET-G3 and it may be functioning; it may also stem from a hereditary neoplastic syndrome. panNEC-G3 also has a higher rate of metastasis than panNET, and one study found that distant metastasis was already present at diagnosis in 46.3% of cases [14]. The liver is the most common site of metastasis, and other metastatic sites include the lymph nodes, bone, lungs, skin, and brain [15]. A report from the Surveillance, Epidemiology, and End Results (SEER) database found that the median overall survival of 2546 patients with poorly differentiated gastroenteropancreatic neuroendocrine carcinoma (GEPNEC-G3) was 14 months (95% CI: 13–15 months] for patients with advanced local disease (including lymph node metastasis and invasion of the surrounding tissue) and 5 months (95% CI: 4.5– 5.5 months) for those with distant metastasis. Overall survival for panNEC-G3 is conventionally considered to be 8.5–21 months [7, 16, 17, 18]. Some studies have found no difference in survival between SCNEC and LCNEC [19], but others have found that the duration is shorter for LCNEC [8], and no consensus has yet been reached. Overall survival for panNET-G3 is 41–52 months [5, 7, 8, 11]. Considering limitations including sample size and potential selection bias, further studies on the prognostic difference would be needed.
Imaging Differences between NET-G3 and NEC-G3
Imaging findings for panNEC-G3 have little in common with those for panNET. On CT and EUS, panNET typically appears as a clearly demarcated, internally homogeneous, hypervascular tumor, whereas one study found that in 80% of cases panNEC-G3 exhibited a hypovascular pattern on contrast-enhanced CT, with stenosis of the main pancreatic duct visible in 65% of cases, and 81.8% of cases were preoperatively diagnoses as pancreatic carcinoma [9]. On MRI, compared with panNET, panNEC-G3 was hyperintense on diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) values were significantly lower than either healthy pancreatic parenchyma or panNET, a finding that is useful for differentiating between the two [20].
panNET has a low uptake rate of 29% on FDG-PET [21], whereas NEC-G3 has an FDG-PET positive rate of over 80% [22], a difference that is useful for the local diagnosis and staging of tumors. A positive FDG-PET reflects tumor grade, and tends to indicate shorter progressionfree survival and overall survival from the start of chemotherapy [23, 24]. Somatostatin receptor scintigraphy (SRS) reveals expression in 67%–92% of NET-G3 tumors compared with only 40%–50% of NEC-G3 tumors [5, 7, 11, 13]. A relatively new PET/CT technique, using somatostatin analogs labeled with the positron emitting isotope, 68Ga (68Ga-DOTA peptides), has been shown to offer advantages over conventional imaging modalities as well as additional important quantitative and qualitative diagnostic information [25, 26]. However, for both FDG-PET and SRS/68Ga-DOTA peptides, whether or not uptake will be present is unknown before imaging is performed. A recent study has reported that scoring on the basis of the performance of both imaging modalities (NETPET grade) is associated with prognosis [27].
Ki67 Differences between NET-G3 and NEC-G3
In 1996, La Rosa et al. showed that patients with NET expressing the MIB-1 epitope of Ki67 in >2% of cells displayed poorer prognosis compared with NET patients with MIB-1/ Ki67% <2% [28]. This finding was confirmed in other studies [29]. A 20% threshold was established during the Frascati consensus to define NEC [30, 31], and this ratio was validated during the validation clinical studies [32, 33].
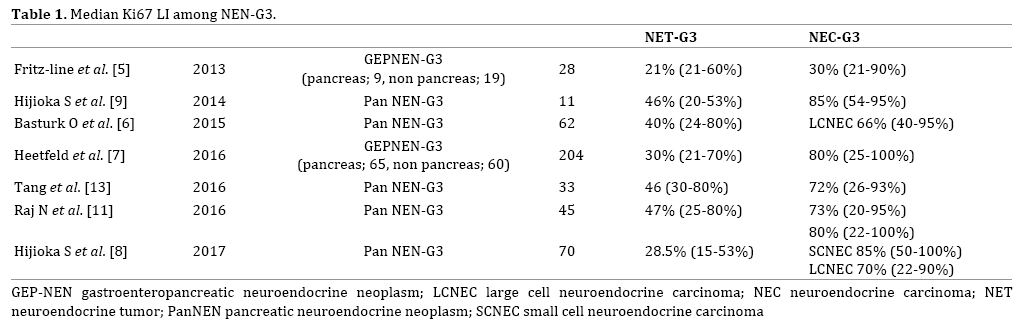
Is it possible to distinguish NET-G3 from NEC based on the Ki67 LI alone? Table 1 shows the median Ki67 LI among NEN-G3 reported in each article. Seven articles (four on panNEN-G3, three on GEPNEC-G3) mentioned Ki67 for NET-G3 and NEC-G3 [5, 6, 7, 8, 9, 11, 13]. Median Ki67 for NET-G3 was 21-47%, and median Ki67 for NEC-G3 was 30- 85%. From these results, setting a cut-off of Ki67 LI to 55% for dividing NET-G3 and NEC-G3 appears suitable [10], but still there is an overlap between the two and it would be difficult to separate NEC and NET-G3 based on the Ki67 LI alone, particularly tumors whose LI range between 20% and 50%. In addition, as Fazio et al. [34] mentioned, setting a clear-cut cut-off value of Ki67 LI seems difficult because of the various factors that affect the evaluation of Ki67, including formalin fixation time, measuring method on Ki67 LI [35, 36], and the existence of heterogeneity within tumors [37].
A recent study has investigated changes in Ki67 at reassessment at the time of disease progression. According to this, 16.7% of panNETs transformed from NET-G2 to NET-G3, and the results suggested that tumors may transform from NET-G2 to NET-G3 with disease progression [38].
Genetic and Immunohistological Alterations of NET-G1/2 and NEC
Thanks to recent advances in the sequencing technologies and computational analyses of large-scale genomic data, key differences in genetic characteristics between NEC-G3 and well-differentiated NET G1/G2 have gradually been revealed. Although our knowledge on the molecular features of NET-G3 is limited because of the recent recognition and rare occurrence, studies consistently suggest that NET-G3 has similar molecular features of NET G1/G2 rather than those of NEC-G3.
Whole-exome sequencing of well-differentiated panNENs was first performed by Jiao et al. in 2011 [39]. First, somatic inactivating mutations in MEN1 were detected in 44% of cases. Second, somatic inactivating mutations in ATRX (thalassemia/mental retardation syndrome X-linked) and DAXX (death-domain-associated protein) were detected in 43% (18% and 25% of cases, respectively) [39]. Subsequent studies revealed a strong correlation between the inactivation of ATRX or DAXX and the telomerase-independent telomere maintenance mechanism termed “alternative lengthening of telomeres” (ALT) and chromosomal instability [39, 40, 41]. Third, somatic mutations in genes associated with the mTOR pathway were detected in 18% of patients [39]. Specifically, the prevalence of mutations was 7% for PTEN, 9% for TSC2 and 1% for PIK3CA. These findings were confirmed by other whole-exome and whole-genome sequencing studies [42]. Scarpa et al. reported the results of wholegenome sequencing for 102 panNETs [42]. Based on that report, clinically sporadic panNETs appear to contain a larger-than-expected proportion of germline mutations, including previously unreported mutations in the DNA repair genes MUTYH, CHEK2 and BRCA2. Together with mutations in MEN1 and VHL, these mutations are present in 17% of patients. Somatic mutations were commonly found in genes involved in four main pathways: chromatin remodeling; DNA damage repair; activation of mTOR signaling (including previously undescribed EWSR1 gene fusions); and telomere maintenance.
In addition to these key alterations, other recurrent mutations of NET-G1/G2 have also been reported, including YY1 (in insulinomas), SETD2, etc. [43].
In contrast, NEC appears to have distinct genetic and immunohistological features from NET-G1/G2 [44, 45]. Yachida et al. [45] performed immunohistochemical and mutational analyses for 19 poorly differentiated panNEC cases, and found abnormal immunolabeling of the p53 protein and Rb protein in 95% and 74% of cases, respectively. They also noted overexpressed Bcl-2 protein in 74% of cases. Other studies followed, consistently showing the recurrent mutations of TP53, Rb1 and KRAS in NECs, which were rarely found in NET-G1/G2 (Table 2). Taken together, NET-G1/G2 is characterized by frequent mutations of MEN1, DAXX, and ATRX, while NEC by mutations of TP53, Rb1, and KRAS. This feature gives reasonable grounds for the categorization of NET-G3 discussed below. NEC and pancreatic carcinoma possess genetic similarities, with NEC exhibiting the same “big four” genetic mutations (TP53, KRAS, CDKN2A, and SMAD4) seen in normal-type pancreatic carcinoma. However, the frequency of KRAS mutations, which are present in almost all cases of pancreatic carcinoma, is comparatively low in NEC, suggesting that pancreatic carcinoma and panNEC-G3 may have different genetic backgrounds. Tang et al. have proposed a diagnostic algorithm for panNEC-G3 that incorporates genetic data in addition to conventional morphological diagnosis [46]. Tumors with the morphological characteristics of NET that have lost DAXX and ATRX expression are classified as NET-G3, and those with Rb1 deletion or abnormal TP53 expression as NEC-G3. This may improve diagnostic accuracy in cases where diagnosis is difficult on the basis of morphology alone.
Data on genetic mutations may thus both improve diagnostic yield and provide predictive factors for response to treatment and prognosis. From the viewpoint of treatment strategy, too, accurate specimen collection and pathological diagnosis on the basis of EUS-FNA and resected samples will also become more important when starting chemotherapy for panNEC-G3.
Genetic and Immunohistochemical Abnormalities in NET-G3 (Table 2)
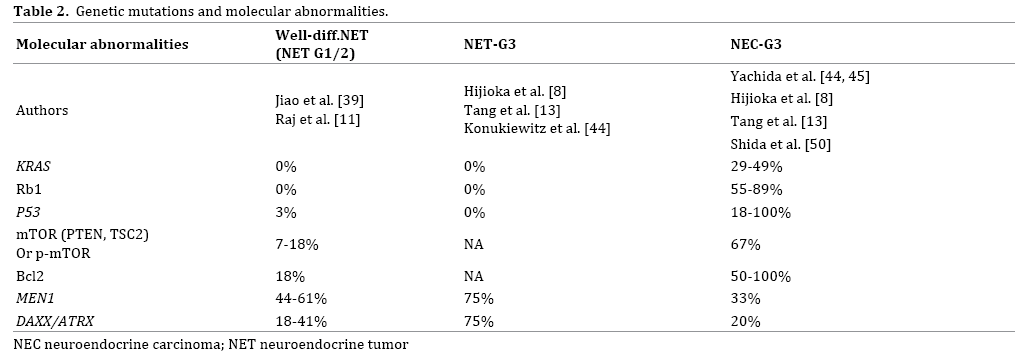
There are a few studies to date that focused on the genetic and immunohistochemical abnormalities in NET-G3. Tang et al. [13] performed targeted sequencing of RB1, DAXX, ATRX and MEN1 in 4 pancreatic welldifferentiated NETs with high-grade component and found DAXX/ATRX/MEN1 mutations in three of four pancreatic WDNETs in the high-grade component (NET-G3) as well as its lower-grade counterpart. RB1 gene mutations, along with loss of Rb protein expression or abnormal p53 expression on immunohistochemistry, were not detected in WDNETs of any grade within the tumors.
Hijioka and Hosoda et al. [8] examined 70 patients, analyzing 21 NETs-G3 (30%) and 49 NECs-G3 (70%). NET-G3 showed no abnormal Rb expression (0%), and no mutations in KRAS (0%), whereas NEC-G3 showed frequent Rb loss (54.5%) and KRAS mutations (48.7%).
Konukiewitz et al. analyzed TP53 mutation and immunohistochemistry of 9 cases of WDNET-G3, and found abnormal expression of DAXX or ATRX in 4/9 cases. The TP53 gene and immunolabeling of Rb1 and p53 proteins were intact in all cases [44].
NEC-G3 presents TP53 mutation found in 18-100% and KRAS mutation in 29-49% [45, 47], whereas NET-G3 does not show such mutation [8, 9, 13, 39]. Taken together, these molecular studies consistently support the view that NET-G3 is closely related to NET-G1/G2 rather than NEC. Moreover, these molecular features may serve as adjunct markers of distinction of NET-G3 from PDNEC, particularly large-cell NEC, when histological distinction between them was challenging [8, 12, 13, 44].
Response of NET-G3 to Platinum-Based Chemotherapy (Table 3)
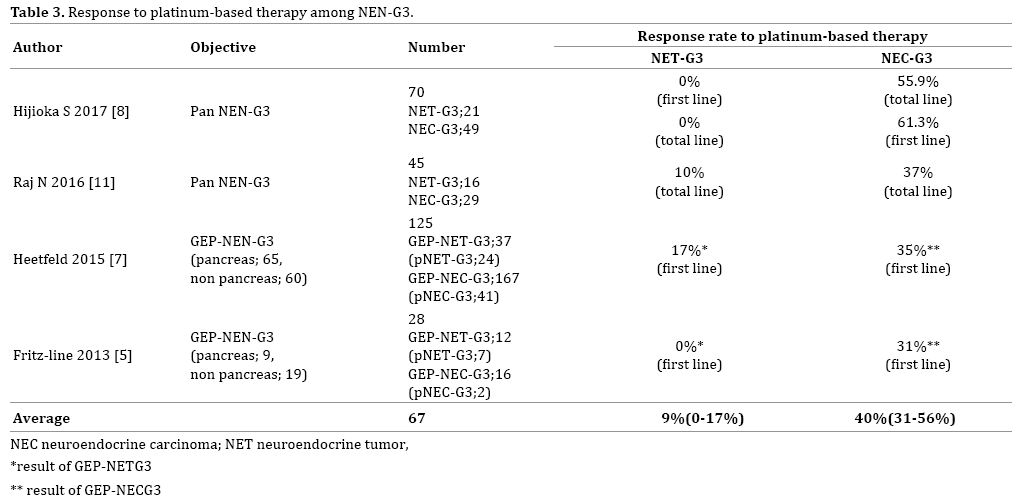
Vélayoudom-Céphise et al. [5] investigated 20 patients with gastroenteropancreatic and thoracic NEC who had been treated with platinum-based chemotherapies. No cases of NET-G3 exhibited response to platinum-based chemotherapy (0%), whereas 31% (5 of 16) large cell NECs showed response. Heetfeld et al. [7] reported 12 patients with gastroenteropancreatic (GEP) NET-G3 and 113 patients with GEP-NEC treated using platinumbased chemotherapy and revealed that the response rate was lower for GEP NET-G3 (17%) than for GEP NEC-G3 (35%; P=0.18). Nitya et al. [48] reported that one of 10 panNET-G3 patients (10%) responded to platinumbased chemotherapies, whereas 10 panNET-G3 patients (37%) responded to platinum-based chemotherapies. In a Japanese panNEN-G3 study, response to platinum-based chemotherapy for NET-G3 was extremely poor, with a RR of 0%. In comparison, the RR for NEC-G3 was good, at 55.9% (P<0.001).
Taken together, the distinction between NET-G3 and NEC-G3 is extremely important in determining treatment options for patients with panNEN-G3, and platinum-based chemotherapy should not be used as the first-line therapy for NET-G3.
In addition, when stratifying PanNEN-G3 according to Rb and KRAS status, panNEN-G3 with Rb loss or with mutated KRAS showed significantly higher RR to platinumbased chemotherapy than those without (Rb loss, 80% vs. normal Rb, 24%, p=0.006; mutated KRAS, 77% vs. wild-type, 23%, p=0.023). Rb was a predictive marker of response to platinum-based chemotherapy even in NEC-G3 (P=0.035). As a result, Rb and KRAS offer promising predictors of response to platinum-based chemotherapy for PanNEN-G3, and Rb also predicts response for NEC-G3.
Chemotherapy for NET-G3
As mentioned above, cases of NET-G3 show poor response to platinum-based chemotherapy. So, what is a useful regimen for NET-G3?
Among panNET patients, the PI3-K/AKT/mTOR pathway is reportedly activated, and expressions of TSC2 or PTEN inhibiting activity of the mTOR pathway are decreased in most cases of panNET. These patients reportedly show a shortened progression-free survival period [46].
However, as in well-differentiated NET, mutation to the PI3K/AKT/mTOR pathway has been found in small-cell lung cancer [49]. Furthermore, overexpression of mTOR has been reported in 67-80% of pancreas NEC [50, 51]. From these findings, some degree of efficacy is anticipated for everolimus, an mTOR inhibitor for panNEC-G3. Actually, some reports have noted that everolimus was effective for NET-G3 and high-grade NEC [52, 53], and NECTOR studies [54] are ongoing in Japan. Also, in more recent years, the RR to alkylating agent among 45 pancreas NET-G3 was 50% [48]. The 2016 European Neuroendocrine Tumor Society (ENETS) guidelines recommend alkylating agent-based combination therapy e.g. STZ+ 5-FU or temozolomide (TMZ)+capecitabine(CAP) for panNET-G3 [55]. Recently, multicenter study evaluated the response of STZ based, platinum-based and dacarbazine/TMZbased chemotherapy regimens as first-line treatment in 74 patients with pNETs and KI-67 LI > 10% (31% included NET-G3) [56]. There was no difference in the PFS between the three regimens; shorter NET-G3 cases (HR 2.15, 95% CI: 1.18-3.92, p=0.012) and age above 55 years (HR 1.84, 95% CI: 1.06-3.18, p=0.030) were associated with shorter median PFS.
Multiple clinical trials are ongoing for GEP-NETG3. The ECOG-ACRIN Cancer Research Group is performing a randomized, controlled phase II study of etoposide +cisplatin vs. temozolomide+capecitabine for non-small cell carcinoma and GEPNET-G3. The registration was started with the goal of 126 cases from 2015. TEM+CAP can be expected to achieve high response from NET-G3.
Haukeland University Hospital is performing a phase II study of everolimus+TEM for GEPNET-G3 (Ki67, 20-55%) in 40 patients from 2014 (primary endpoint, DCR).
Preliminary evidence of immune dysregulation in the NET microenvironment has been recently provided. Expression of programmed death-ligand 1 (PD-L1) and programmed death-ligand 2 (PD-L2) by tumor cells [57, 58, 59] may drive immune evasion in GEP-NETs, and immune checkpoint inhibitors are currently under intensive clinical investigation (NCT02955069, NCT02939651, NCT02923934).
Because NET-G3 is a new disease classification, little evidence is available for treatment regimens in particular, and this is an important topic for future studies.
Chemotherapy for NEC-G3
Regarding drug therapy for NET G1 and G2, therapeutic drugs differ for the pancreas and gastrointestinal tract, but the treatment strategy for NEC-G3 is basically the same as for the pancreatic/gastrointestinal tract.
As noted earlier, poorly differentiated NEC (small cell carcinoma or large cell carcinoma) occurs in organs such as the lung, pancreas and gastrointestinal tract, but regardless of the organ, the biological malignancy and genetic background are similar. The loss of RB protein expression seen in lung small cell carcinoma has been reported even in pancreatic NEC [16, 25].
For these reasons, and likewise for extrapulmonary NEC, various guidelines recommend administering the same platinum-based regimens used for chemotherapy for small cell lung cancer (European Neuroendocrine Tumor Society [55], NCCN Clinical Practice 2017 version 3 [4]). The current standard chemotherapy for small cell lung cancer is cisplatin+etoposide combination therapy (EP therapy) or cisplatin+irinotecan combination therapy (IP therapy). EP therapy has mainly been used in the United States and Europe. ENETS guidelines recommend EP therapy for NEC, regardless of the organ [55]. However, cytotoxic drug treatment for small cell lung cancer has shown little improvement in therapeutic results over many years.
So, what are the treatment results of platinum regimens for panNEC? To date, no results have been obtained from prospective clinical trials, and studies have mainly been retrospective. The Nordic NEC study [3] in Northern Europe and the multicenter GEP-NEC retrospective study by Yamaguchi et al. [16] are instructive. In the Nordic NEC study [3], the most frequently used methods were EP therapy at 51%, followed by etoposide+CBDCA therapy at 27%, showing the frequent use of etoposide. Meanwhile, the Japan GEP-NEC study was characterized by the fact that IP therapy was overwhelmingly used, at a rate of 62%, followed by EP therapy at 18%. Response rates to IP therapy and EP therapy in the treatment of hepatobiliarypancreatic NEC were reported as 39% (7/18) and 12% (4/34), respectively. The reason why RR with platinum chemotherapies were low is considered that not only NEC-G3, NET-G3 cases were also included in this report.
Gene mutations in the PI3-K/AKT/mTOR pathway were found not only in well-differentiated NET but overexpression of mTOR was reported in 67% (6/9) to 80% (29/36) of panNEC patients [50]. Based on this background, everolimus, an mTOR inhibitor, is expected to prove effective even for NEC-G3.
Emerging Issues Regarding NEC-G3
In the Japan PanNEN-G3 study, KRAS gene mutation and loss of Rb protein expression were each found in about half of NEC-G3 patients: 48.7% and 54.5% [8]. Moreover, the first-line response rate to platinum-based regimens for NEC-G3 was 61.3%. Conversely, about 40% of panNEC-G3 does not respond to platinum-based regimens. Based on these results, predictive factors of platinum-based regimens for the response to NEC-G3 is important.
When we excluded NET G3 and analyzed 49 patients diagnosed with NEC-G3, only retained Rb immunolabeling group showed significantly worse response for platinumbased chemotherapy compared with loss of Rb (P=0.031). Loss of Rb immunolabeling was only a predictor of platinum-based chemotherapy response even in NEC-G3 (OR=7.7; 95% CI, 1.16–51.1; P=0.035). Indeed, response to platinum-based regimens for NEC-G3 without retained Rb immunolabeling group (abnormal Rb group) was 80% (12 of 15), whereas response to platinum-based regimens for NEC-G3 with retained Rb immunolabeling group (normal Rb group) was significantly lower (38.4%; 5 of 13) than abnormal Rb group (P=0.031). From genetic and morphological perspectives—as shown in Table 4. NEC-G3 may be divided into two groups, with NEN-G3 as a whole divided into 3 groups.
As for NET-G3, the NEC-G3 group without Rb abnormality is less likely to respond to platinum chemotherapy. Accordingly, future studies need to elucidate whether the same treatment as for NET-G3 should be used, or whether new treatment options are required.
This research was supported by the Practical Research for Innovative Cancer Control from Japan Agency for Medical Research and development, AMED.
S. Hijioka has received honoraria from Pfizer, Novartis, Fuji film, Novel pharma, and research funding from Teijin and Novartis.
C. Morizane received honoraria from Pfizer, Novartis, Fujifilm, Novel pharma, Yakult Honsha and research funding from GlaxoSmithKline, Pfizer, Nobelpharma, Eisai, Yakult Honsha, ONO PHARMACEUTICAL, Taiho Pharmaceutical.
N.Mizuno has received research funding from Zeria Pharmaceutical, Taiho Pharmaceutical Co. Ltd., Merck Serono, AstraZeneca, NanoCarrier, Eisai, and MSD, and honoraria from Taiho Pharmaceutical Co. Ltd., Elli Lilly Japan K.K., Yakult Honsha, Novartis, Pfizer, and Kyowa- Hakko Kirin.
T Okusaka received honoraria from Novartis Pharma, Taiho Pharmaceutical Merck Serono, Eli Lilly, Dainippon Sumitomo Pharma, Bayer Yakuhin, Yakult, Nobelpharma, Nippon Kayaku, Baxter, Astellas Pharma, FUJIFILM RI Pharma, AstraZeneca, Ono Pharmaceutical, EA Pharma, Nippon Chemiphar, Daiichi Sankyo, Celgene, Eli Lilly Japan K.K., and research funding from Eisai, Novartis Pharma, Yakult Honsha, Taiho, Nippon Boehringer Ingelheim, Kowa Company, Kyowa Hakko Kirin.
W hosoda and K hara does not have conflict-of-interest.