Research Article - (2021) Volume 0, Issue 0
Received: 10-Dec-2021 Published: 31-Dec-2021
Objective: Low Back Pain (LBP) is common and surgical treatment for LBP can fail for many different reasons, one being depressive symptoms and anxiety contributing to persistent symptoms. We prospectively analyzed Cortisol plasma levels and depressive symptoms on outcome regarding pain and quality of life after instrumented fusion.
Methods: Patients (n=50) underwent instrumented fusion for LBP. Before surgery, patients completed the Beck Depression Inventory (BDI) and the Core Outcome Measures Index (COMI). Demographic variables and history of depressive symptoms were noted and blood plasma cortisol measured. Outcome was evaluated at 3 and 12 months’ follow-up.
Results: There was a significant postoperative improvement in mean COMI total score and subscores. There was no association between preoperative cortisol levels and either depressive symptoms or clinical outcome. Preoperative BDI uniquely explained 6% variance in quality of life 12 months after surgery. Depressive symptoms correlated significantly with pre and postoperative symptoms of back pain, but not leg pain.
Conclusion: In this group of patients, higher scores for depression were identified as a negative predictor of quality of life 12 months postoperatively, independent of back pain and leg pain at 12 months. Depressive symptoms correlated significantly with pre and postoperative symptoms of back pain, but not leg pain. The present study highlights the importance of assessing psychological measures in this patient group to provide better clinical management before or alongside surgical treatment.
Low back pain; Leg pain; Depressive symptoms; Cortisol; Spine; Instrumented fusion; BDI
Low Back Pain (LBP) is common in industrialized countries with a lifetime prevalence of up to 85% and is the most frequently reported musculoskeletal impairment [1,2]. Since it is a frequent cause for reduced quality of life successful treatment is important [2]. Degenerative spine disease is considered one of the most frequent causes of LBP [3-6]. However, the factors determining the course of the disease are diverse. Among others, there is evidence for the impact of psychological factors on the course and severity of LBP [7-11].
Depressive states occur in up to 45% of patients with chronic LBP [10-12]. While the majority of patients with LBP experience improvement after surgical treatment, depression predicts a poor outcome with less or no pain relief. There is also preliminary evidence for an association of somatization and mental well-being with the outcome of surgical treatment [13-15]. Depressive states are characterized by a variety of symptoms and have different causes. Hormonal alterations have been studied and strong evidence was found for higher plasma cortisol levels in patients with depression [16]. Interestingly, the relation between pain and Hypothalamus-Pituitary-Adrenal (HPA) axis activity is less clear. There are only few divergent studies available reporting altered cortisol levels in LBP patients compared to healthy subjects [17-19].
There are surgical treatments options especially for patients suffering from LBP in presence of degenerative spine disease but the multiple influencing factors in LBP lead to surgical treatment failures in up to 32% [20].
To improve preoperative assessments in LBP-patients and to make appropriate use of possible treatment options, a better understanding of the complicated interplay between quality of life, depressive symptoms and the role of cortisol and pain experience is required. Therefore, the aim of this study was to examine the impact of self-reported depressive symptoms and blood plasma cortisol on patient-rated outcome after single segment lumbar decompression and instrumented Transforaminal Lumbar Interbody Fusion (TLIF) in patients with symptomatic single segment degenerative lumbar spine disease.
Study design and inclusion criteria
This was a prospective observational study including 50 patients operated for LBP due to degenerative lumbar spine disease at a designated spine center between November 2011 and July 2013. The study was approved by the local ethics committee (Kantonale Ethikkommission, Kanton Zürich, Switzerland-KEK-ZH 2011-0200) and all patients gave their written informed consent to participate prior to enrollment. Outcomes were collected through the prospective outcomes registry of the Schulthess Clinic Zurich, linked to EUROSPINE’s Spine Tango Registry.
Inclusion criteria were aged ≥ 18 years, with symptomatic single segment lumbar degenerative lumbar spine disease due to a history of repeated lumbar disc herniation or single segment disc degeneration with degenerative spondylolisthesis [21].
Exclusion criteria were a previous history of spine surgery other than lumbar micro discectomy, known neuropsychiatric disease other than a history of anxiety or depressive symptoms, history of substance dependency, insufficient knowledge of one of the languages in which the Core Outcome Measures Index (COMI) is available [22].
Preoperative workup
All patients complained of LBP, some leg pain and reduced quality of life before surgery. The underlying pathology was diagnosed by X-Ray and MRI of the lumbar spine as well as neurological and clinical examination. Patients that satisfied the inclusion/ exclusion criteria were planned for elective surgery within 4-6 weeks. All patients completed the Beck Depression Inventory (BDI) at admission, and patients’ demographics, history of neuropsychiatric symptoms, medication use and neurological symptoms were noted. Patients’ self-rated multidimensional outcome was evaluated using the Core Outcome Measures Index (COMI; see below for further information) before admission and at 3 and 12 months’ follow-up, with the questionnaires being mailed in the post to the patients [23].
Surgical technique
Patients underwent single-level posterior lumbar decompression and instrumented Transforaminal Lumbar Interbody Fusion (TLIF) under general anesthesia the day after admission. Patients were transferred back to the ward after 3-4 hours' observation in the recovery room and were given instructions from the physiotherapist about postoperative exercises before being discharged from hospital care.
Measurement of outcome variables, severity of depression and plasma cortisol
Patient self-rated multidimensional outcome was evaluated using the COMI. The COMI is a short, multidimensional outcome instrument, with excellent psychometric properties, that has been recommended for use in monitoring the outcome of spinal surgery from the patient’s perspective. COMI (scored 0-10) consists of single items that cover the domains of pain (one question each for axial pain and peripheral pain), function, symptom-specific well-being, general quality of life, and social and work disability. Higher scores indicate a worse status. Some of the items were first proposed by a group of experts in 1998 and the index itself was later used for outcome evaluation of surgical treatment of degenerative spine disease [24,25]. The minimum clinically important change score for improvement has been defined as 2.2 points [26]. The questionnaire is feasible to implement on a prospective basis in routine practice, and is as responsive as many longer spine outcome questionnaires [25,26]. The shortness of the COMI and its multidimensional nature make it an attractive option to comprehensively assess all patients within a given Spine Centre and it is the primary outcome measure of the Spine Tango registry [25-28].
Since the surgical intervention aims to increase the well-being of the patient, considering the emotional, social, and physical aspects of chronic LBP, the general quality of life item from the COMI (scored 1-5) was defined as the primary outcome measure in our study.
To assess for depressive symptoms, patients completed the Beck Depression Inventory (BDI) at admission. The BDI is a well-validated self-assessment questionnaire to examine the extent of depressive symptoms [29]. It is often used in clinical or epidemiological study designs [30,31]. It contains 21 questions to be answered by the patient regarding the clinical condition during the week prior to the assessment. The patient can choose one of four degrees of a certain feeling. Summation of the scores for each item leads to an overall numeric score of 0 to 63. Scores of 14-19 are rated as mild, 20-29 as moderate and 30-63 as severe depressive symptoms [29-31].
After awakening on the day after admission, patients gave fasting blood samples for the analysis of plasma cortisol, used as a marker of the activity of the hypothalamic-pituitary-adrenal axis and a potential biomarker for depressive symptoms.
Statistical analysis
The demographic data of the patients was evaluated using descriptive statistics. After visual examination, changes in outcome data between the different time-points were evaluated using repeated measures ANOVA. All associations between variables were evaluated using Pearson correlations. Multiple regression analyses were used to identify independent predictors of general quality of life measured with the corresponding COMI item at 3 and 12 months' follow-up. Only variables showing a significant univariate correlation with the quality of life item at 12 months after surgery were included in the regression model. Preoperative BDI scores were entered to determine whether depressive symptoms made an additional contribution to the regression model, after COMI scores for back pain and leg pain intensity at 12 months, and quality of life at baseline had been entered. For the regression analysis, predictor variables were in the following order: Block 1-COMI Quality of life before surgery, Block 2-COMI back pain and COMI leg pain 12 months after surgery, and Block 3-Preoperative BDI score. Co-linearity problems because of associations between pain values and quality of life scores were assessed, but standard β values were low indicating that the association between pain and quality of life was not overpowered and the additional predictor variable BDI score could be added to the model. Statistical calculations were made using Microsoft Excel and SPSS Statistic Software Version 22. P values less than 0.05 were considered statistically significant.
Patient demographics
Overall, 50 patients agreed to participate in the study. Four patients were later excluded from the data analysis due to lack of either baseline or follow-up data. These four patients were all females with a mean age of 66.8 years (74,73,62,58) and one of them had had an intraoperative dural tear.
Patients’ demographics, surgical procedures and complications are shown in Table 1. The mean (SD) age of the patients was 65.4 ± 9.7 years and (32/46; 69.6%) were female. Hypertension (26.1%), obesity (17.4%) and history of depressive symptoms (10.1%) were the most common comorbidities. The L4/5 segment was most frequently affected (27/46; 58.7%). The surgical complication rate was 4/46 (8.5%) with dural tear (6.5%) being the most common complication.
| Demographic or clinical variable | Number (%) |
|---|---|
| Patients | 46 |
| Sex male/female | 14 (30.4%)/32 (69.6%) |
| Mean patient age (SD) (years) | 65.4( ± 9.7) |
| Occupation | |
| Skilled labour | 7(15.2%) |
| Physical labour | 8(17.4%) |
| Retired | 14(30.4%) |
| Housewife | 10(21.7%) |
| Unknown | 7(15.2%) |
| Marital status | |
| Unmarried | 3(6.5%) |
| Married | 33(71.7%) |
| Divorced | 4(6.5%) |
| Widowed | 4(8.7%) |
| Unknown | 2(4.3%) |
| Spinal segments treated | |
| L2/3 | 1(2.1%) |
| L3/4 | 9(19.6%) |
| L4/5 | 27(58.7%) |
| L5/S1 | 9(19.6%) |
| Degenerative disc disease | 46(100%) |
| Degenerative spondylolisthesis | 30(65.2%) |
| Most frequent comorbidity | |
| Hypertension | 12(26.1%) |
| Obesity | 8(17.4%) |
| Depressive disorder | 5(10.1%) |
| Diabetes | 4(8.7%) |
| Panic disorder | 1(2.2%) |
Table 1: Patients’ demographic and clinical information.
Symptoms, self-rated depressive symptoms and cortisol measurements at baseline
Table 2 (left column) shows the preoperative scores for the COMI and four of its sub-domains (back pain, leg pain, symptomspecific well-being and quality of life). The mean BDI score was 8.6 ± 4.9 (range 1-20). The preoperative scores for COMI back pain were significantly higher in the 7 patients that were categorised as depressed (BDI total score ≥ 14) than in the 41 who were not depressed (7.9 ± 1.5 vs. 5.8 ± 2.4, respectively; P=0.037, F(1)=4.610, ηp2=0.091). However, there was no significant difference between them for COMI Leg pain (6.4 ± 2.3 vs. 5.8 ± 2.6, respectively; P=0.517, F(1)=0.427, ηp2=0.009) (Figure 1). The mean preoperative fasting plasma cortisol was 494.6 ± 153.6 nmol/l (range 185-814 nmol/l). There was no significant correlation between baseline plasma cortisol levels and depressive symptoms (BDI score) (r=-0.072, P=0.633) Compared with baseline values, statistically significant improvements in COMI Back pain, COMI Leg pain, COMI Quality of life, COMI Symptom-specific well-being and overall COMI score were seen at 3 months (p ≤ 0.001) and 12 months (P<0.001) after surgery. There was a significant correlation between preoperative BDI scores and both preoperative and 12-month postoperative COMI Back pain scores (r=0.46,P=0.001 and r=0.32,P=0.027; respectively) but not between BDI and gender, age, 3-month COMI Back pain scores or COMI Leg pain scores at any time-point (Table 3). Plasma cortisol levels showed no significant correlation with patient-rated outcome at any time point (Table 4).
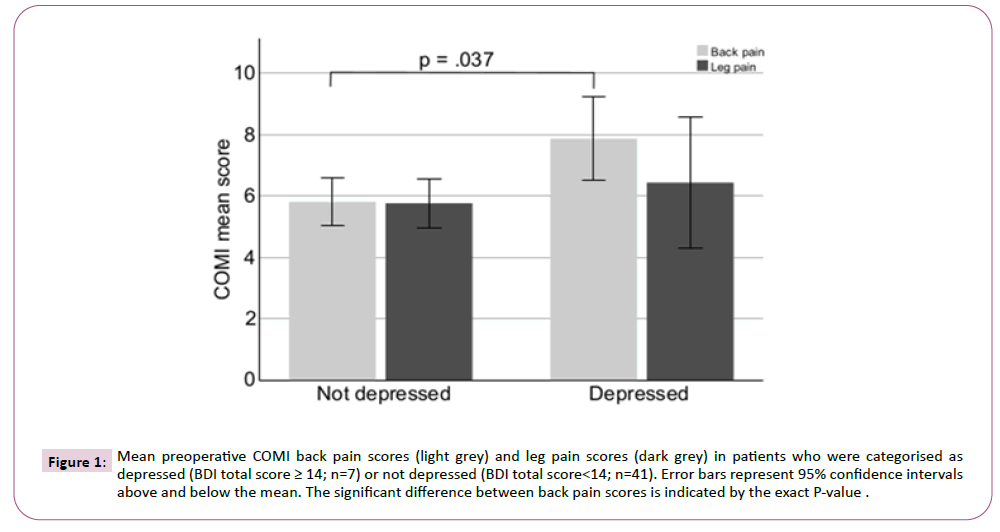
Figure 1: Mean preoperative COMI back pain scores (light grey) and leg pain scores (dark grey) in patients who were categorised as depressed (BDI total score ≥ 14; n=7) or not depressed (BDI total score<14; n=41). Error bars represent 95% confidence intervals above and below the mean. The significant difference between back pain scores is indicated by the exact P-value .
| Preoperative | 3 month | 12 month | Repeated measure ANOVA | |||
|---|---|---|---|---|---|---|
| F | Sig. | ηp2 | ||||
| COMI score | 7.5 ± 1.8 | 4.2 ± 2.5 | 3.5 ± 2.3 | 64.58 | <0.001 | 0.58 |
| COMI back pain | 6.1 ± 2.3 | 3.0 ± 2.5 | 2.7 ± 2.0 | 44.58 | <0.001 | 0.48 |
| COMI leg pain | 5.6 ± 2.5 | 2.6 ± 2.5 | 2.0 ± 2.1 | 52.62 | <0.001 | 0.52 |
| COMI higher pain | 7.0 ± 1.7 | 3.6 ± 2.7 | 3.1 ± 2.1 | 49.48 | <0.001 | 0.51 |
| COMI symptom-specific wellbeing | 3.9 ± 1.0 | 2.6 ± 1.1 | 2.4 ± 1.1 | 52.1 | <0.001 | 0.53 |
| COMI quality of life | 3.8 ± 0.9 | 2.4 ± 1.0 | 2.4 ± 1.0 | 55.47 | <0.001 | 0.54 |
Table 2: Patient-rated outcome scores (N=46) before, and 3 and 12 months after TLIF.
|
COMI back pain | COMI leg pain | ||||
|---|---|---|---|---|---|---|
| Preoperative | 3 month | 12 month | Preoperative | 3 month | 12 month | |
| Preoperative | 0.458 (.001)* | 0.208 | 0.318 | 0.087 (0.556) | 0.041 | 0.148 |
| BDI | - | -0.156 | (0.027)* | - | -0.782 | -0.315 |
Note: *P ≤ 0.05
Table 3: Pearson correlation coefficients (significance) of BDI score and COMI back pain and COMI Leg pain before and after T-LIF.
|
BDI | COMI back pain | COMI LEG pain | ||||
|---|---|---|---|---|---|---|---|
| Preop. | Preop. |
3 month | 12 month | Preop. | 3 month | 12 month | |
| Plasma | -0.072 | -0.032 |
0.104 | 0.152 | -0.037 | 0.018 | 0.002 |
| cortisol | -0.633 | -0.828 |
-0.482 | -0.301 | (-0.803) | -0.902 | -0.991 |
Table 4: Pearson correlation coefficients (significant) of cortisol levels and BDI score COMI back pain and COMI Leg pain.
Preoperative predictors of COMI Quality of life at 12 months' follow-up
The results of the stepwise regression analysis to investigate the influence of preoperative depression on quality of life at 12 months after instrumented fusion are shown in Table 5. The overall model was able to account for 47% (adjusted R2) of the variance in 12-month COMI Quality of life scores, with preoperative BDI scores being a significant predictor, but accounting for just 6% of the variance. The association of a standard β<.5 and a VIF<2 indicated only moderate collinearity in the regression analysis for the independent variables COMI Leg pain (VIF=1.23) and COMI Back pain (VIF=1.35), suggesting that the preoperative BDI score was a unique predictor of postoperative COMI Quality of Life at 12 months’ follow-up, independent of COMI Back pain and COMI Leg pain scores.
| Block number | Independent variables | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Std. β | T-value | P-value | Std. β | T-value | P-value | Std. β | T-value | P-value | ||
| 1 | (Constant) | - | - | - | - | 1.808 | 0.078 | 1.498 | 0.142 | |
| COMI quality of life before TLIF | 0.136 | 0.909 | 0.368 | 0.087 | 0.753 | 0.455 | 0.06 | 0.587 | 0.561 | |
| 2 | COMI leg pain 12 months after TLIF | - | - | - | 0.291 | 2.304 | 0.026 | 0.29 | 2.398 | 0.021 |
| COMI back pain 12 months after TLIF | - | - | - | 0.482 | 3.787 | 0 | 0.4 | 3.163 | 0.003 | |
| 3 | Preoperative BDI | - | - | - | - | - | - | 0.27 | 2.351 | 0.024 |
Note: Model 1: R2=0.018, adjusted R2=0.00, R2 change=0.02, F change=.826, significance of F change p=0.368; Model 2: R2=0.453, adjusted R2=0.41, R2 change=0.43, F change=16.7, significance of F change p=0.000; Model 3: R2=0.52, adjusted R2=0.47, R2 change=0.06, F change=5.53, significance of F change p=0.024.
Table 5: Results of the multiple regression analysis showing the influence of preoperative BDI score on COMI quality of life 12 months after TLIF.
In this prospective single-center study, we investigated the role of preoperative BDI score and blood plasma cortisol on postoperative COMI subscores in patients suffering from LBP undergoing lumbar instrumented fusion.
Overall, LBP, leg pain and quality of life showed significant improvements compared with baseline over the 12-month follow-up. Mild depressive symptoms before surgery were frequent (34.8% patients) and preoperative BDI scores were found to predict a low but statistically significant proportion of the variance in patient-rated quality of life at 12 months' followup. There was neither correlation between cortisol levels and mild depressive symptoms nor influence of cortisol levels on outcome. Depressive symptoms correlated with LBP before and at 12 months' after surgery, but not with leg pain at either timepoint.
Preoperative depressive symptoms and quality of life
Depression is frequent among patients with poor surgical outcome [7,9,32]. Trief, et al. [9] studied 102 patients 6 months after undergoing lumbar surgery. They found that depression predicted failure to return to work, persisting pain and failure to report improved functional abilities [9]. Mannion, et al. showed that two psychological predictors (fear-avoidance beliefs and depression) were able to explain 17% of the variance in COMI quality of life in 163 patients, 6 months after undergoing spine surgery [7]. A recent review including 42 clinical trials related to psychosocial determinants of outcome after lumbar spinal fusion surgery also showed that depression is one of the most powerful predictors of adverse outcomes after lumbar fusion [32]. In the present study, 6% of the variance in COMI quality of life 12 months after surgery was explained by the BDI scores. This is not a large effect size, but when combined with other potentially negative predictors for a given individual, it may play a relevant role in effecting a worse patient-rated outcome. Potentially the assessment of self-rated depression before surgery may provide a simple marker that can be used to identify patients who may benefit from surgery to a lesser degree than others.
Plasma cortisol and depressive symptoms
The effect of alterations of the hypothalamic-pituitary-adrenal axis and especially the role of cortisol levels in relation to depressive states has been studied widely in recent years. A relationship has been found between the diagnosis of major depressive disorder and significantly altered cortisol awakening response compared to healthy controls [16]. In the present study we were not able to find any correlations between plasma cortisol in fasting blood samples and preoperative depressive symptoms. A possible explanation might be the relatively low burden of depressive symptoms in our study group. Furthermore, a metaanalysis by Burke, et al. [33] showed that the cortisol levels of depressed and non-depressed individuals did not differ at baseline or in response to stress; they only differed significantly during recovery from stress, with depressed patients exhibiting higher levels of cortisol. Studies with blood samples taken in the afternoon showed higher baseline levels of cortisol, as well as a blunted stress reactivity and impaired recovery, in the depressed patients [33]. In the present study, afternoon cortisol levels were not evaluated; these might have shown a better relationship with self-reported depressive symptoms. The cortisol awakening response does not appear to differ between patients with LBP and healthy subjects [34], but differences have been observed in relation to the cortisol levels recorded during experimental pain stimulation, one study reported lower salivary cortisol levels with experimental pain in LBP patients compared with either healthy participants or (38) depressed patients, and another showed that patients with chronic LBP have higher levels of salivary cortisol than (39) healthy control subjects [19,18]. A recent interventional study found increased evening but not morning salivary cortisol release in LBP patients after a Mindfulness-Based Stress Reduction (MBSR) program [35]. In summary, the mechanisms linking chronic LBP, depressive states and cortisol are poorly understood and deserve further study.
Preoperative depressive symptoms, LBP and leg pain
Our study showed that affective symptoms are most strongly associated with LBP, rather than leg pain, both before and after surgery. This is an interesting finding, since the believed origin of LBP and leg pain differs. Back pain is a condition of multiple causes such as disc pain, muscle pain and joint pain whereas concomitant radicular leg pain is thought to be most frequently due to a single nerve root being compressed by degenerative tissue [36,37]. In our study, depressed patients reported stronger back pain compared to not depressed patients. This difference could not be found in the leg pain intensity (Figure 1). There is not much evidence on the association between affective symptoms and pain in different anatomical sites and the results of the existing studies are somewhat conflicting. A recent systematic review in patients undergoing lumbar disc surgery stated that there is slightly better evidence for an association between back pain and depressive symptoms than for leg pain [13]. In the crosssectional study of Hakkinen, et al. higher scores for depression were associated with both greater back pain and greater leg pain two months after lumbar disc surgery [38]. However, depression was measured after surgery, so each-higher back or leg pain-may has led to greater depression making it difficult to establish cause and effect. In a group of chronic musculoskeletal pain patients, no differences in depression scores were found between those with LBP and those with upper or lower extremity pain [39]. However, the value of these findings is limited because patients with upper and lower extremity pain were grouped together and the patients in the LBP group reported only low pain levels. Interestingly there is also another perspective on back pain and depressive states. One study found that physical pain was frequent among outpatients seeking psychotherapy, with 82% reporting pain in at least one location. LBP was the most frequently reported location of pain. Leg pain-often seen as a concomitant symptom in patients suffering from predominant LBP in the presence of degenerative spine disease-was rare. Muscular symptoms and subsequent back pain are also observed as somatic symptoms considered being of diagnostic significance for depression [40]. Consequently, complementary therapy with a focus on pain management and cognitive control of muscle tension should be added to the treatment program of chronic pain patients to address depressive symptoms prior to surgery [15].
Another important consideration is that MRI studies of patients without symptoms related to the spine frequently reveal severe degeneration of the spine, especially in the elderly population [41,42]. This being the age group that frequently undergoes spine surgery, there might be some patients who-despite showing coincidental degeneration of the lumbar spine in imaging studiessuffer from LBP for reasons unrelated to degeneration of the spine. If these patients are then operated with fusion for this incidental degeneration, this could lead to no or minimal pain relief, a poor overall outcome, remaining poor quality of life, and ongoing depression after surgery. This might explain why affective symptoms correlated with postoperative back pain, but not with postoperative leg pain, in our study. One of the steps before considering surgical treatment options in patients with severe-and assumed symptomatic-degenerative changes of the lumbar spine should be a thorough work up for other causes of LBP and depressive symptoms. If these other causes are missed during the preoperative workup, the chance of persistent LBP after surgery increases.
In summary, our findings fit well with the existing evidence that depressive symptoms are a statistically significant predictor of patient outcome after spine surgery. Specifically, we showed that depressive symptoms are predictors of quality of life at 12 months' follow-up in a homogenous study population with a standardized presurgical evaluation. We were not able to identify any association between cortisol measurements and either depressive symptoms or outcome.
In this homogenous group of patients, mild depressive symptoms were frequent (34.8%) and higher scores for selfrated depression were identified as a negative predictor of quality of life 12 months postoperatively, independent of back pain and leg pain at 12 months. Furthermore, depressive symptoms correlated significantly with pre and postoperative symptoms of back pain, but not leg pain. Even though there is some evidence in the literature that cortisol measurements, as a marker for the hypothalamic-pituitary-adrenal stress axis, are altered in patients with major depressive disorder and chronic pain, we could not find any correlation between cortisol levels and either depressive symptoms or clinical outcome among our patient group. The present study highlights the importance of assessing psychological measures prior to instrumented fusion. This may help the clinician to better provide personalized clinical management, including possible supplementary psychological therapy before or alongside surgical treatment.
Although this was a prospective study of patients from a high volume spine center, the study group was only a patient cohort from a single institution. The results only apply to a subgroup of patients with single level degenerative segment disease, surgically treated with instrumented fusion. The highest BDI score recorded for any of the patients was 20 and the average was 9, which indicates only mild to moderate depressive symptoms in our patient group. Furthermore, the BDI alone explained only 6% of the variance in quality of life 12 months after surgery.
Citation: Bellut D, Mannion AF, Burkhardt JK, Mutter U, Porchet F, et al. (2021) The Effect of Depressive Symptoms and Blood Plasma Cortisol on Pain and Quality of Life after Single Segment Lumbar Fusion Surgery. Clin Psychiatry Vol.7 No.S6: 117.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.