Review Article - (2024) Volume 9, Issue 2
The effect of electroacupuncture on the management of pain and articular function related to primary knee osteoarthritis: systematic review and meta-analysis
Virginia Barbeitos Cruz1*,
Ana Lúcia Junger1,
Denise Pinheiro Marques Alves dos Santos2 and
Ana Luiza Lima Sousa3
1Post-graduate Program in Health Sciences, School of Medicine, Universidade Federal de Goiás, Goiânia, GO, Brazil
2School of Nursing, Universidade Federal de Goiás, Goiânia, GO, Brazil
3School of Nursing, Post-graduate Program in Health Sciences, School of Medicine, Universidade Federal de Goiás, Goiânia, GO, Brazil
*Correspondence:
Virginia Barbeitos Cruz,
Post-graduate Program in Health Sciences, School of Medicine, Universidade Federal de Goiás, Goiânia, GO,
Brazil,
Email:
Received: 25-Mar-2024, Manuscript No. IPJHCC-24-19317;
Editor assigned: 27-Feb-2024, Pre QC No. IPJHCC-24-19317 (PQ);
Reviewed: 10-Apr-2024, QC No. IPJHCC-24-19317;
Revised: 15-Apr-2024, Manuscript No. IPJHCC-24-19317 (R);
Published:
22-Apr-2024, DOI: 10.36846/2472-1654-9.2.9013
Abstract
Background: Osteoarthritis (OA) is the most prevalent joint disease in the world, causing pain, rigidity, and functional limitation of adults over 45 years.
Objective: We conducted a systematic review to synthesize the results of clinical randomized studies to measure the effectiveness of electroacupuncture (EA) in the management of pain and articular dysfunction in adults with primary knee OA (KOA), Kellgren-Lawrence grades 2 and 3.
Methods: Two independent reviewers searched for interventional clinical studies on the effectiveness of EA published on PubMed, Embase, Scopus, and Web of Science databases between January 2001 and January 2024. The statistical analysis focused on the effect size. Data summarization was performed through specific meta-analyses
for the outcomes of interest. For statistical analysis, R software version 4.3.2 was used. The quality of the studies was assessed according to Critical Appraisal Skills Programme (CASP) and Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).
Results: Three out of 7,428 articles were eligible. Meta-analysis showed no effect of EA on the attenuation of pain and joint dysfunction in KOA [2.67 standardized mean difference (SMD); -9.86; 4.52, p=0.249] and functional limitation (-2.02 SMD -6.86; 2.83 p=0.215), p<0.01. We observed compliance with STRICTA of 72.7% at 58.5%, with
moderate risk (54.5% and 63.6%) or low risk of bias (90.9%) in CASP.
Conclusion: In the meta-analysis, we identified that EA is not effective in treating pain and joint impairment in patients with primary KOA.
Trial registration: International Prospective Register of Systematic Reviews (PROSPERO) CRD42023469183 (https:// www.crd.york.ac.uk/prospero/display_record.php?RecordID=469183).
Keywords
Acupuncture therapy; Eletroacupuncture; Knee osteoarthritides; Intervention studies
Introduction
Osteoarthritis (OA) is the most prevalent joint condition and
symptomatic knee OA (KOA) affects approximately 18% of
women and 10% of men worldwide [1]. Women aged 60 years
and older are the most affected group and also have a higher
incidence of pain and radiological changes [1]. This condition
affects all components of the synovial joints, especially the knee, causing pain, morning stiffness, and gait instability,
effusion with or without crepitation, functional limitation, and
progressive impact on quality of life [2]. Local inflammation
may be present, but it is neither the primary source of joint
dysfunction nor associated with systemic symptoms [3].
Although the precise etiology of KOA remains unclear, obesity,
menopause, and muscle weakness are likely to influence injury
severity and functional impact [4]. Biomechanical factors, such
as a ± 2° variation in the angulation between the hip and the
knee, as well as genu varum, confer a higher risk for articular
cartilage degeneration in the medial compartment of the knee
[5]. Tricompartmental knee disease is seen in only 25% of these
individuals [2].
Given that the diagnosis is essentially clinical and the differential
diagnosis with other arthropathies of the knee, such as
ankylosing spondylitis and rheumatoid arthritis, is mandatory,
radiological assessment is of fundamental importance to
provide information on the degree of joint involvement and
enable grading the disease [6,7]. Early diagnosis of KOA is not
yet a reality. Radiological changes are unrelated to symptoms,
since 30% of individuals have structural changes detectable on
X-ray, of which only 40% are symptomatic [6,8]. The progression
of KOA is associated with the presence of cytokines and other
pro-inflammatory markers in synovial fluid and joint tissues,
and its specificity has not yet been demonstrated [9-11].
The classification system for KOA proposed by Kellgren and
Lawrence is based on the identification of osteophytes and
the measurement of the joint space in the medial and lateral
compartments of the knee [12]. Of interest in this review are
individuals with KOA, Kellgren-Lawrence (KL) grades 2 (small
osteophytes and small joint space reduction) and 3 (moderatesized
osteophytes and 50% joint space narrowing) [6,13,14].
The clinical management of KOA is challenging, considering that
the cure for the disease is not known to date [15]. Therapeutic
recommendations for symptom control are periodically
published and updated. Although electroacupuncture (EA) is
not consolidated as an effective intervention, acupuncture (AC)
is recommended by the European League Against Rheumatism
(EULAR) in the “miscellaneous therapies” category and
considered to have a moderate effect, level of evidence 1A [16].
In contrast, AC or EA are contraindicated in the latest National
Institute for Health and Care Excellence (NICE) guideline [17],
while the guidelines of the American College of Rheumatology
(ACR) published in 2020 conditionally recommend the use of
AC, because the available scientific evidence is considered
weak or very weak [18]. Moreover, the latest update of
the Osteoarthritis Research Society International (OARSI)
guidelines does not even mention AC [19].
The inconsistency of AC in updated guidelines is not only
related to the methodological fragilities of clinical studies,
but also to the lack of adoption of concepts that support its
rationality, as a therapeutic method, and the effectiveness
attributed to the intervention [20]. An example of this is the
interchangeable use of the terms AC and EA. By definition,
AC is the technique of inserting needles through the skin for
therapeutic purposes. This insertion of thin, lumenless metal
needles causes micro-injury to the tissue and activation of C- and
A-δ fibers peripherally, as well as extensive brain connectivity,
including the sensorimotor cortex and the autonomic nervous
system. From this stimulus, a cascade of neurochemical and
humoral events is triggered, giving rise to adaptive top-down
modulation mechanisms to control pain and inflammation.
A variant of AC, EA involves associating needles with electric
current, enhancing the therapeutic effects of the former [21].
The great advantage of EA lies in the definition of the design,
frequency, and intensity of the wave, according to the purpose
of the intervention, the parameters of which can be controlled
and reproduced [22-25].
From the date of publication of the Revised STandards for
Reporting Interventions in Clinical Trials of Acupuncture
(STRICTA), in 2001, the standards of notification of interventions
in AC clinical trials would be expected to have improved, but this
is not the case [26]. Therefore, the methodological criticisms
persist, generating insecurity about the reproducibility of the
protocols published to date [27].
Thus, we aimed to perform this systematic review to analyze
and synthesize the results from clinical studies that evaluated
the effectiveness of EA in the management of pain and
functional limitation in patients with primary KOA, KL grades
2 and 3.
Methods
A search was carried out on the databases PubMed, Embase, Scopus, and Web of Science. The study search, screening, selection, data extraction, and crosschecking were independently and blindly performed by two reviewers. The selection process was conducted from October 31st, 2023 to January 24th, 2024. Disagreements were solved by a master reviewer. The following hierarchy was adopted as a justification for excluding identified studies: Research format/design; type of publication, such as guidelines, protocols, letters to the editor, animal studies, book chapters, conferences, books; secondary KOA; joint postoperative status; other joint conditions; different from the topic; AC modality; comparator characteristics; different outcome of pain and function.
PICO Strategy
We adopted the PICO strategy to define our guiding questions and objectives as follows: P–patients with painful primary KOA, KL grades 2 and 3; I–EA; C–pharmacotherapy; O–pain and joint function.
Main question: Is EA effective in treating pain and functional limitation in adults with primary KOA, KL grades 2 and 3, compared to pharmacotherapy?
Secondary question: Do the reviewed studies adhere to the parameters of good practices for clinical research and scientific communication in AC, defined by STRICTA and Consolidated Standards of Reporting Trials (CONSORT) [26,28]?
Inclusion Criteria
Study design: Randomized clinical trials.
Years of publication: Between January 2001 and February 2023.
Patients and clinical conditions: Age ≥ 45 years; both sexes; diagnosis of KOA, KL grades 2 and 3.
Intervention: EA technique (material, needle dimensions, number of needles used per therapeutic session, anatomical site and insertion depth, retention time, number of therapeutic sessions, brand and model of the electrical stimulator and characteristics of the electrical wave adopted).
Comparators: Pharmacotherapy provided for in the current management and treatment guidelines (description of the medication, dose, and duration of treatment, route of administration, allowing systemic and intra-articular routes).
Measurement of efficacy: Visual Analogue Scale (VAS), numerical rating scale (NRS), and Western Ontario and McMaster Universities Osteoarthritis pain scale (WOMAC).
Exclusion Criteria
Study and design: Unpublished studies, research protocols, expert opinions, conferences and letters to the editor, and nonrandomized studies.
Patients and clinical conditions: KOA secondary to trauma or surgery.
Intervention: EA associated with other techniques.
Comparators: Auriculopuncture, moxibustion, cupping therapy, AC laser, sham AC, manual AC, minimalist/superficial AC, incandescent needle, acupotomy, surgical treatment, hyaluronic acid, phytotherapy/medicinal plants, biological medication, regenerative medicine, stem cells, plateletrich plasma, physiotherapy, physical exercise, massage, manipulation techniques, meditation, yoga, and mindfulness.
Variables of Interest
The following were adopted as variables of interest for the purposes of this review: Gender (nominal), age as completed years of life (continuous), KL grades 2 and 3 osteoarthritis (nominal), VAS and NRS (discrete), as well as the functional gain of the affected joint, measured by WOMAC (ordinal), a questionnaire suitable for assessing physical limitations imposed by pain, stiffness, and joint dysfunction.
Search Strategy
The descriptors used in the review process were previously consulted in the Medical Subject Headings (MeSH) of the Latin American and Caribbean Center on Health Sciences Information and MeSH of PubMed for publications exclusively in English, namely: “Acupuncture,” “electroacupuncture,” “clinical trials,” “randomized clinical trials,” “controlled study,” “knee osteoarthritis,” “primary knee osteoarthritis,” “joint disease,” “knee pain,” in different combinations (Tables 1-4).
Table 1: Search strategy for PubMed
| Descriptors and Boolean operators |
| #1 |
"Rheumatic Diseases"[MeSH Terms] OR "Osteoarthritis"[MeSH Terms] OR "osteoarthritis, knee"[MeSH Terms] OR "Joint Diseases"[MeSH Terms] OR "Knee Joint"[MeSH Terms] OR "Rheumatic Diseases"[Title/Abstract] OR "Osteoarthritis"[Title/Abstract] OR "osteoarthritis knee"[Title/Abstract] OR "Joint Diseases"[Title/Abstract] OR "Knee Joint"[Title/Abstract] OR "Knee Osteoarthritis"[Title/Abstract] OR "Osteoarthritis of Knee"[Title/Abstract] OR "Osteoarthritis of the Knee"[Title/Abstract] |
| #2 |
"Electroacupuncture"[MeSH Terms] OR "Acupuncture Therapy"[MeSH Terms] OR "Electric Stimulation Therapy"[MeSH Terms] OR "Electroacupuncture"[Title/Abstract] OR "Acupuncture Therapy"[Title/Abstract] OR "Electric Stimulation Therapy"[Title/Abstract] OR "Electroacupuncture Therapy"[Title/Abstract] |
| #3 |
"Double blind method"[MeSH Terms] OR "Cross-over studies"[MeSH Terms] OR "Clinical Trial"[Title/Abstract] OR "Randomized Controlled Trial"[Title/Abstract] OR "Controlled Clinical Trial"[Title/Abstract] OR "controlled trial"[Title/Abstract] OR "trial"[Title/Abstract] OR "double blind procedure"[Title/Abstract] OR "Double blind method"[Title/Abstract] OR "crossover procedure"[Title/Abstract] OR "Cross-over studies"[Title/Abstract] OR "intervention"[Title/Abstract] |
| #4 |
#1 AND #2 AND #3 AND (2002:2023[PDAT]) |
Table 2: Search strategy for Embase
| Descriptors and Boolean operators |
| #1 |
'osteoarthritis'/exp OR 'knee osteoarthritis'/exp OR 'knee pain'/exp OR 'knee pain':ti,ab,kw OR osteoarthritis:ti,ab,kw OR 'knee osteoarthritis':ti,ab,kw |
| #2 |
'electroacupuncture'/exp OR 'electrotherapy'/exp OR electroacupuncture:ti,ab,kw OR electrotherapy:ti,ab,kw |
| #3 |
'randomized controlled trial'/exp OR 'controlled study'/exp OR 'randomized controlled trial':ti,ab,kw OR 'controlled study':ti,ab,kw OR 'controlled clinical trial':ti,ab,kw |
| #4 |
#1 AND #2 AND #3 AND 2002 PY TO 2024 PY |
Table 3: Search strategy for Scopus
| Descriptors and Boolean operators |
| #1 |
"Rheumatic Diseases" OR osteoarthritis OR "Osteoarthritis, Knee" OR "knee pain" OR "Osteoarthritis of the Knee" OR "Knee Osteoarthritides" OR "Knee Osteoarthritis" OR "Osteoarthritis of Knee" |
| #2 |
"Electroacupuncture" OR electrotherapy OR "Electric Stimulation Therapy" OR "Electroacupuncture Therapy" |
| #3 |
"Randomized Controlled Trial" OR "Clinical Trial" OR "Controlled Clinical Trial" OR "controlled study" |
| #4 |
#1 AND #2 AND #3 PUBYEAR>2001 AND PUBYEAR<2025 |
Table 4: Search strategy for Web of Science
| Descriptors and Boolean operators |
| #1 |
((((((((((ALL=(“Rheumatic Diseases”)) OR ALL=(“Osteoarthritis”)) OR ALL=(“Osteoarthritis, Knee”)) OR ALL=(“Joint Diseases”)) OR ALL=(“Knee Joint”)) OR ALL=(“Knee Osteoarthritides”)) OR ALL=(“Knee Osteoarthritis”)) OR ALL=(“Osteoarthritis of Knee”)) OR ALL=(“Osteoarthritis of the Knee”)) OR ALL=(“knee pain”)) OR ALL=(“knee disease”) |
| #2 |
((((((ALL=(“Electroacupuncture”)) OR ALL=(“Acupuncture Therapy”)) OR ALL=(“Electric Stimulation Therapy”)) OR ALL=(“Electroacupuncture Therapy”)) OR ALL=(“acupuncture”)) OR ALL=(“physical medicine”)) OR ALL=(“electrotherapy”) |
| #3 |
((((ALL=(“Randomized Controlled Trial”)) OR ALL=(“Clinical Trial”)) OR ALL=(“Controlled Clinical Trial”)) OR ALL=(“RCT”)) OR ALL=(“controlled study”) |
| #4 |
#1 AND #2 AND #3 |
Analgesic and anti-inflammatory drugs for systemic and intraarticular use, recommended in the guidelines of the American Academy of Orthopedic Surgeons, ACR, European Society for Clinical and Musculoskeletal Diseases, EULAR, NICE, and OARSI were included as pharmacological comparators [17-19,29-31].
Study Selection, Management and Data Collection
After searching the aforementioned electronic databases, the identified studies were exported to the Zotero reference manager (https://www.zotero.org/). The online tool Rayyan was used for screening and selection, following the order: Title, abstract, and full text [32]. Subsequently, the results of the selected studies were analyzed and the data of interest were extracted, synthesized, and analyzed.
Data Extraction
For the purposes of this review, the following data extracted from the selected studies were considered relevant:
1. Epidemiological results–sex, age, and duration of the disease
2. Diagnosis–Primary KOA, KL grades 2 and 3
3. Type of study, sample size, randomization method, followup, and justified withdrawals
4. Detailed description of the intervention, anatomical reference of the neuro-reactive points stimulated, number of knees treated in the same individual, quality and intensity of the electrical current associated with the needles, stimulation time, model and manufacturer of the electrical stimulation device used in the studies.
Statistical Analysis
The statistical analysis of the results focused on the effect size, understood as an estimate of the magnitude of the difference between the intervention groups. Data summarization was performed through specific meta-analyses for the outcomes of interest, namely VAS and NRS for pain and WOMAC for joint function and quality of life. For statistical analysis and graph plotting, R software version 4.3.2 was used [33]. All the statistical analyses were performed using the statistical package Meta: General Package for Meta-analysis (https:// cran.r-project.org/web/packages/meta/index.html).
To identify systematic errors, the Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) was used [34]. It has five domains: Bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, and bias in selection of the reported result.
Inverse variance models were adopted to determine the weight of each study in the meta-analysis, as well as random effect models [35], whose means, standard deviation, and sample size obtained from the comparison groups were used to estimate the standardized mean difference due to the heterogeneity of the population.
To assess the magnitude of the difference between the groups, Cohen's classification was used, whereas to assess heterogeneity Cochran's Q and I² statistics were used [36]. In all analyses p values<0.01 were adopted as significant.
Qualification of Selected Studies
In order to answer the second question, the articles selected for statistical analysis were read in full and critically assessed for quality using the Randomised Controlled Trial Standard Checklist of the Critical Appraisal Skills Programme (CASP) [37]. In this checklist, each of the 13 questions about the method of the studies must be answered as one of three options: Yes (Y), no (N), or can’t tell (CT). The risk of bias is calculated by the number of questions that are answered selecting Y in high, moderate, or low risk of bias. If any question is answered with CT, it is not considered in the calculation of the risk of bias. Above 70% it is considered low risk of bias, between 50% and 70% moderate, and up to 49% high. Also, the articles were checked for clarity, reproducibility, and compliance with STRICTA recommendations.
Results
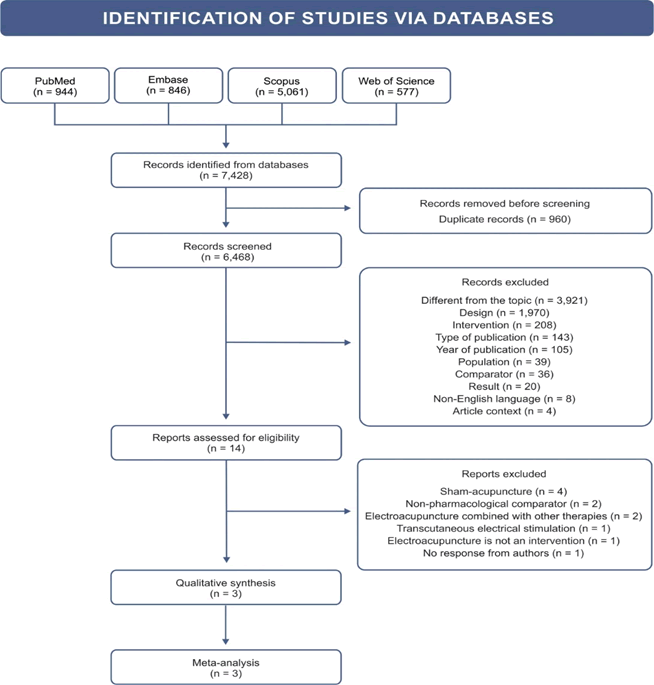
All the steps for the selection and extraction of data were recorded in a flowchart (Figure 1), constructed according to the recommendations of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [38]. We identified 7,428 potentially eligible studies, which were individually analyzed regarding their qualitative and quantitative characteristics. Of this total, 14 were directed to the full reading of the article, to check eligibility, and three were selected for final analysis [39-41].
The demographic characteristics of the populations studied, as well as the details of the therapeutic protocols adopted in each of the selected clinical trials are summarized in Table 5. The population of the three included studies totaled 176 individuals, of both sexes, aged over 48 years, randomly distributed into treatment groups, of which only those undergoing EA and pharmacotherapy were included. Important heterogeneity was observed in the design of interventions and their controls, especially regarding the following aspects: Different frequencies of the electrical wave; unjustified selection of anatomical sites/ AC points; different frequency, interval number, and duration of therapeutic sessions, factors that together and individually have the potential to affect the effect size.
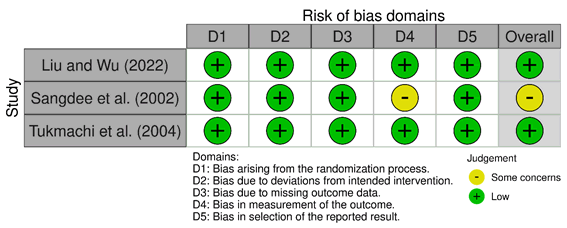
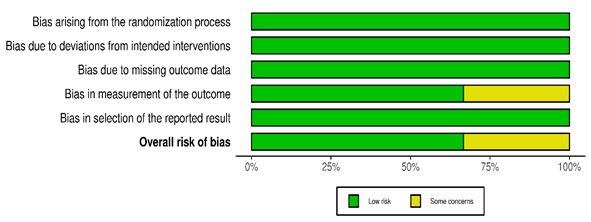
Using the RoB 2 tool [34], a low risk of bias was identified in the studies carried out by Tukmachi et al. [40], and Liu and Wu [41] (Figures 2 and 3). However, in the study conducted by Sangdee et al. [39], the lack of clarity in the blinding criteria and characterization of placebo EA and sham AC was the subject of some concern.
Of the three selected studies, the ones carried out by Sangdee et al. [39] and Tukmachi et al. [40] followed-up the treated populations for a period of two and one month, respectively, resulting in lasting therapeutic effects of EA.
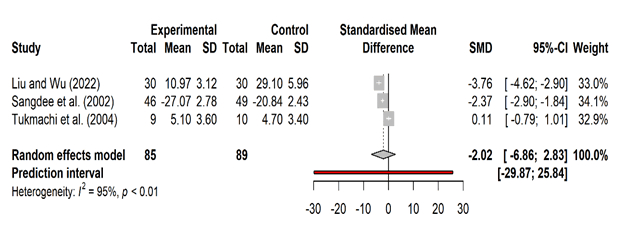
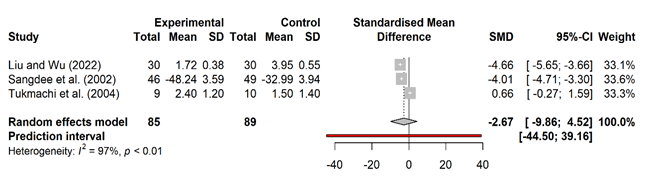
Although some tendency was observed in favor of the intervention, the effect size and the confidence interval lacked statistical significance, since they were clearly oriented towards centrality. Therefore, the meta-analysis showed that EA is not effective on the primary results related to pain attenuation (VAS) (Figure 4) and functional limitation (WOMAC) (Figure 5).
Table 5: Demographic data and interventions in the selected studies
| Authors (year)/country |
Patients’ n (%) |
Average age (years) |
KL grade |
Intervention |
Primary results |
Associations |
| F |
M |
EA |
PhT |
EA |
PhT |
VAS |
WOMAC |
| Sangdee et al. (2002)/Thailand [44] |
EA 38 |
EA 10 |
EA 65.10 (3.40) |
1-4 |
(n=48) |
(n=49) |
Week 0 |
Week 0 |
p=0.21 |
p=0.94 |
| PhT 38 |
PhT 11 |
PhT 62.14 (7.53) |
[ST35 (Dubi)+Xiyan medial]+ |
Week 0 |
VAS: 66.87 (SD 22.34) |
VAS: 64.79 (SD 23.41) |
| |
|
|
[PG+LR8 (Ququan)], |
Paracetamol 500 mg (rescue): 2 cp, up to 4x/day+placebo |
WOMAC: 52.60 |
WOMAC: 50.76 |
| |
|
|
superficial needles, biphasic pulses, 2 Hz, |
Weeks 1-4 |
(SD 18.13) |
(SD 17.98) |
| |
|
|
20 min 3x/week every other day |
diclofenac 25 mg 1 cp 3x/day+paracetamol 500 mg (rescue) 2 cp/day |
|
|
| |
|
|
Total: 12 sessions |
|
Week 4 |
Week 4 |
| |
|
|
|
|
VAS: -48.24 (SD 3.59) |
VAS: -32.99 (SD 3.94) |
| |
|
|
|
|
WOMAC: |
WOMAC: |
| |
|
|
|
|
-27.07 |
-20.84 |
| |
|
|
|
|
(SD 2.78) |
(SD 2.43) |
| Tukmachi et al. (2004)/United Kingdom [45] |
14 |
5 |
EA 61 |
1-3 |
(n=9) |
(n=10) |
Week 0 VAS: 6.0 |
Week 0 |
p=0.012 |
p=0.012 |
| PhT 61 |
Two Xiyan points (“eyes” of the knee); low frequency 6Hz, square-wave pulses 1 ms; duration, 20 min front+ |
Group A: AI withdrawal one week before the start of the study; Groups B and C: maintained AI and analgesics already used by patients |
(SD 1.9) |
VAS: 7.0 |
| |
20 min back |
|
WOMAC: 10.2 |
(SD 1.3) |
| |
|
|
(SD 3.0) |
WOMAC: 12.6 (SD 3.1) |
| |
|
|
|
|
| |
|
|
Week 5 |
Week 5 |
| |
|
|
VAS: 2.4 |
VAS: 1.5 |
| |
|
|
(SD 1.2) |
(SD 1.4) |
| |
|
|
WOMAC: 5.1 |
WOMAC: 4.7 (SD 3.4) |
| |
|
|
(SD 3.6) |
|
| Liu and Wu (2022)/China [46] |
43 (71.66) |
17 (28.33) |
EA 58 ± 7 |
NI |
(n=30) |
(n=30) |
Week 0 |
Week 0 |
p<0.01 |
p<0.01 |
| PhT 62 ± 8 |
ST34, SP10), ST35, EX-LE4, GB34, EX-LE2), SP6, uni or bilaterally, |
Celecoxib 0.2 g, 1 cp/day for 21 days |
VAS: 5.78 ± 1.39 |
VAS: 5.75 ± 1.40 |
| |
dense wave, 100 Hz; adjusted for patient Comfort 1x/day for 6 consecutive days, 1 day interval |
|
WOMAC: 33.37 ± 12.61 |
WOMAC: 33.23 ± 12.80 |
| |
Total: 21 days |
|
|
|
| |
|
|
Week 4 |
Week 4 |
| |
|
|
VAS: 1.72 ± 0.38 |
VAS: 3.95 ± 0.55 |
| |
|
|
WOMAC: |
WOMAC: |
| |
|
|
10.97 ± 3.12 |
29.10 ± 5.96 |
| AI, non-steroidal anti-inflammatory; cp, capsule; SD, standard deviation; EA, electroacupunture; VAS, visual analogue scale; F, female; PhT, pharmacotherapy; KL, Kellgren-Lawrence; M, male; NI, not informed; WOMAC, Western Ontario McMaster Osteoarthritis Index. |
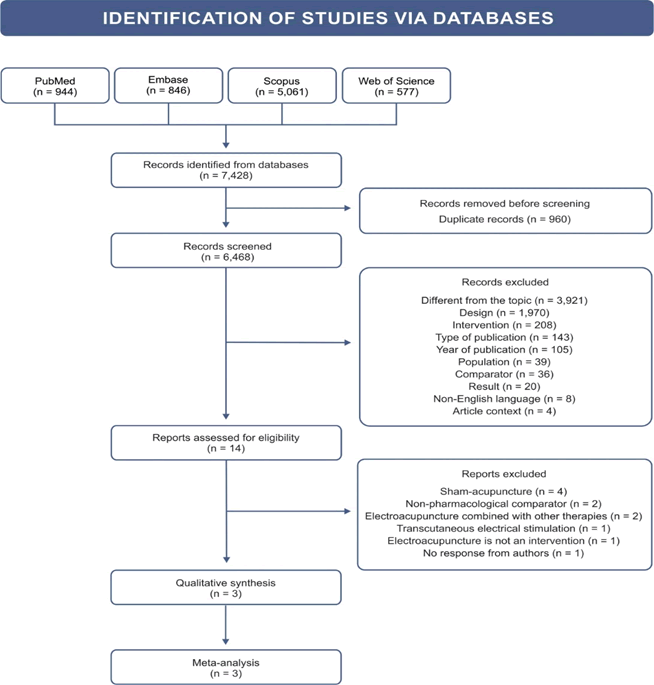
Figure 1: Flowchart of the selection process
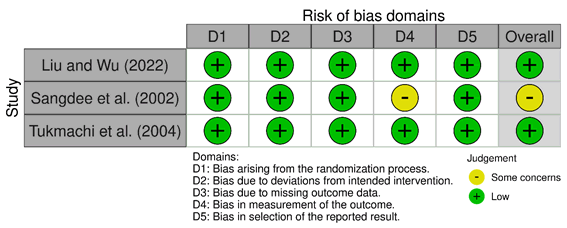
Figure 2: Risk of bias
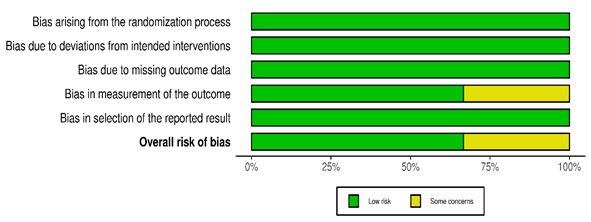
Figure 3: Categorization of risk of bias
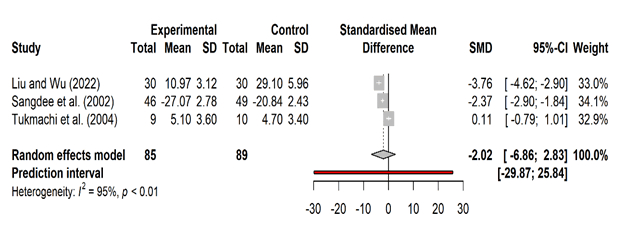
Figure 4: Meta-analysis of quality of life according to the Western Ontario McMaster Osteoarthritis Index guidelines
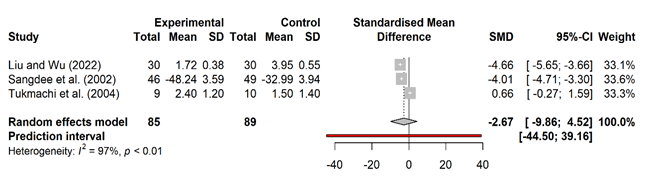
Figure 5: Meta-analysis of pain intensity according to the visual analogue scale
The compliance of the studies included in the meta-analysis to the CONSORT/STRICTA checklist [26] is available as Supplementary material (Table S1). Greater compliance of these assumptions was observed in the study of Liu and Wu [41], published more recently (67.6%), while that of Sangdee et al. [39] achieved the lowest (45.9%). Of the 37 items and subitems applicable that make up this guideline, only 7 (18.9%) (6b, 9, 11b, 14a, 14b, 23, and 24) were not met by any of the selected articles. To complement the qualitative analysis of the selected articles, we used the Randomised Controlled Trial Standard Checklist of CASP, available as Supplementary material (Table S2) [37]. The study carried out by Sangdee et al. [39] had moderate risk of bias (69.3%), while those conducted by Tukmachi et al. [40] and Liu and Wu [41] both presented low risk of bias (84.7%).
Discussion
Despite the increasing number of reviews published each
year on the effectiveness of AC for treating KOA, the volume
of evidence generated does not exactly reflect consistency or
safety, a fact that is partially attributed to neglect of protocols
dedicated to promoting transparency and reproducibility
of clinical studies such as PRISMA, CONSORT, and STRICTA,
compromising the use of the results obtained to create farreaching
public policies [26,28,38,42]. To illustrate the obstacle
to transparency, several and different techniques, from the
simplest ones such as the minimalist AC, to the most bizarre
such as the fire-needle AC, are sheltered under the aegis of AC,
making it difficult to understand the rationality of the method
and the measurement of its effects [42,43]. Moreover, active
placebo controls are still regular practice in research sets [44].
The present systematic review aimed to verify the effectiveness
of EA treatment compared to pharmacotherapy, in patients
diagnosed with primary KOA, taking as reference pain
attenuation, as well as the functional gain of the affected
joint. The inclusion and exclusion criteria adopted were
even more rigorous than those recommended by CONSORT/
STRICTA, because no AC variants other than EA were included
as intervention of interest, nor did we admit sham AC as a
physiologically inert comparator, since the devices used for
this are not capable of controlling the same effects expected
for EA [45]. Given the greater rigor adopted, we anticipated
difficulty in selecting studies, since the vast majority use the
traditional Chinese AC model, by definition, not scientific,
based on inserting metal needles into points along the
“meridians”, understood as “energy channels”. Given its
subjective nature and the lack of understanding of the “AC
point” and “meridians” as anatomical entities, measuring the
effectiveness of this treatment becomes a challenge and is
often a source of methodological bias as well [46-48].
The meta-analysis showed that EA is not effective on the
primary results related to pain attenuation [2.67 standardized
mean difference (SMD); -9.86; 4.52] and functional limitation
(-2.02SMD -6.86; 2.83), p<0.01. Great heterogeneity was
observed in the configuration of the comparator groups in
selected studies, although this does not reflect negatively on the risk of bias, which was considered low to moderate.
Despite the low risk of bias, the selected articles deserve some
reflection. Sangdee et al. [39], for instance, considered the
effect of EA superior to diclofenac for the outcomes of pain,
using VAS, and joint function, mean values of WOMAC total
score, with an improvement by 50% in symptoms, both with
a p<0.05. Liu and Wu [41] used celecoxib as a comparator,
with anti-inflammatory potency [49,50], and reported an
improvement in symptoms by 70% in the comparator group
and by 86.67% in the group treated with EA, both with p<0.05.
In turn, Tukmachi et al. [40] left the choice and dosage of
drugs already used to patients' discretion. Group A underwent
EA while Group B underwent EA plus analgesics and antiinflammatories
already in use, even before the study, showing
improvement in outcomes of interest by 61% and 83%,
respectively, whose means were adjusted to p<0.05. This last
result is corroborated by the trial performed by Berman et al.
[51] and the systematic review conducted by Kwak et al. [52],
in which EA proved to be more effective in treating pain and
joint function as an adjuvant to drug treatment, and not as na
isolated intervention.
Another aspect subject to criticism is the design of the study
performed by Tukmachi et al. [40], who left it to the patients
own discretion, in one of the treatment groups, the choice
of dose and medication to be used, in addition to EA, which
can be understood as a confounding variable. These authors
also stimulated the AC points electrically on each of the knee
extensor and flexor surfaces for 20 minutes, disregarding the
central effects of EA. These effects, widely discussed by Langevin
et al. [53], involve complex neural connectivity, including pain
control mechanisms, such as bottom-up and top-down, which
elicit adaptive reactions from all elements of the pain matrix
that transcend the adopted peripheral mechanistic model. In
none of the three articles included in the statistical analysis the
results were presented separately for sex or KOA radiological
grading strata, compromising sensitivity.
We consider it urgent to update the guiding concepts for
clinical research in this area of knowledge based on available
scientific data, so that research can move forward. Still
anchored in Chinese tradition, the designs of clinical studies
into the efficacy of EA in the management of KOA symptoms
remain inconclusive, while the life expectancy of the world's
population has been steadily increasing, and consequently the
prevalence of degenerative arthropathies, which so negatively
impact the quality of life of these individuals. Given that the
current guidelines are unanimous in their encouragement
of non-pharmacological therapy, they should include EA as
adjuvant treatment, since it is a relatively simple and safe
neuromodulatory technique.
Conclusion
The meta-analysis showed that EA is not effective in treating
pain and joint dysfunction in primary KOA, KL grades 2 and 3.
The qualitative analysis of the selected articles showed partial
compliance to the guidelines for reporting clinical studies,
namely CONSORT, STRICTA, and CASP, and they were classified
as low risk of bias.
Strength and Limitation
The small number of articles selected per se does not constitute
a limitation of this review, considering the rigor of our eligibility
criteria. We adopted only EA as the intervention, and no other
variation of conventional AC, nor did we adopt sham AC or
minimalist AC as inert comparators. Only pharmacological
comparators accepted by the current guidelines for the
management and treatment of KOA were included. Nonetheless,
in the title selection phase, we observed that many article titles
generically had the word “acupuncture”, when, in fact, they
were related to “electroacupuncture”, mentioned only in the
abstracts or methods, which may have led to a loss of articles
at this stage. Additionally, in the selected studies, the desirable
subgroup analysis, guided by the KL classification for KOA, was
not performed. However, patients diagnosed with primary KOA,
KL grades 2 and 3, the reference for our systematic literature
review, were covered in all of them.
Author Credit Statement
VBC (1st reviewer): Conceptualization, methods, investigation,
analysis, data curation, writing-original draft preparation,
and editing, submission; ALJ (2nd reviewer): Search strategy,
investigation, data curation, writing-review, and editing;
DPMAS: Writing-review and editing; ALLS (master reviewer):
Supervision, analysis, writing-review and editing.
Funding
The authors declare they did not receive any specific grant
from funding agencies in the public, commercial, or not for
profit sectors.
Acknowledgement
The authors would like to thank Suzana Oellers for her
commitment and impeccable work in translating the text and
organizing the data.
Conflict Of Interest
The authors declare no conflicts of interest.
References
- Allen KD, Thoma LM, Golightly YM (2022) Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 30(2):184-195.
[Crossref] [Google Scholar]
- Stoddart JC, Dandridge O, Garner A, Cobb J, van Arkel RJ (2021) The compartmental distribution of knee osteoarthritis-a systematic review and meta-analysis. Osteoarthritis Cartilage. 29(4):445-455.
[Crossref] [Google Scholar]
- Block JA (2019) Clinical features of osteoarthritis. In: Hochberg MC, Gravellese EM, Silman AJ, Smolen JS, Weinblatt ME, et al. (7th edition), Rheumatology, Elsevier, Philadelphia, USA. 1522-1529.
- Heidari B, Hajian-Tilaki K, Babaei M (2016) Determinants of pain in patients with symptomatic knee osteoarthritis. Caspian J Intern Med. 7(3):153-161.
[Google Scholar] [PubMed]
- Dell'isola A, Steultjens M (2018) Classification of patients with knee osteoarthritis in clinical phenotypes: Data from the osteoarthritis initiative. PloS One. 13(1):e0191045.
[Crossref] [Google Scholar]
- Malas FU, Kara M, Kaymak B, Akinci A, Ozcakar L (2014) Ultrasonographic evaluation in symptomatic knee osteoarthritis: Clinical and radiological correlation. Int J Rheum Dis. 17(5):536-540.
[Crossref] [Google Scholar]
- Jang S, Lee K, Ju JH (2021) Recent updates of diagnosis, pathophysiology, and treatment on osteoarthritis of the knee. Int J Mol Sci. 22(5):2619.
[Crossref] [Google Scholar]
- Boesen M, Ellegaard K, Henriksen M, Gudbergsen H, Hansen P, et al. (2017) Osteoarthritis year in review 2016: Imaging. Osteoarthritis Cartilage. 25(2):216-226.
[Crossref] [Google Scholar]
- Samuels J, Krasnokutsky S, Abramson SB (2008) Osteoarthritis-a tale of three tissues. Bull N Y U Hosp Jt Dis. 66(3):244-250.
[Google Scholar] [PubMed]
- Varady NH, Grodzinsky AJ (2016) Osteoarthritis year in review 2015: Mechanics. Osteoarthritis Cartilage. 24(1):27-35.
[Crossref] [Google Scholar]
- Van der Kraan PM, Berenbaum F, Blanco FJ, Cosimo B, Lafeber F, et al. (2016) Translation of clinical problems in osteoarthritis into pathophysiological research goals. RMD Open. 2(1):e000224.
[Crossref] [Google Scholar]
- Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 16(4):494-502.
[Crossref] [Google Scholar]
- Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA (2006) Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology. 239(3):818-824.
[Crossref] [Google Scholar]
- Altman RD, Gold GE (2007) Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 15(Suppl A):A1-A56.
[Crossref] [Google Scholar]
- GBD 2021 Osteoarthritis Collaborators (2023) Global, regional, and national burden of osteoarthritis, 1990-2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 5(9):e508-e522.
[Crossref] [Google Scholar]
- Geenen R, Overman CL, Christensen R, Aseniof P, Capela S, et al. (2018) EULAR recommendations for the health professional's approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 77(6):797-807.
[Crossref] [Google Scholar]
- National Institute for Health and Care Excellence (2020) Osteoarthritis: Care and management.
- Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, et al. (2020) 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 72(2):220-233.
[Crossref] [Google Scholar]
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, et al. (2019) OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 27(11):1578-1589.
[Crossref] [Google Scholar]
- Langevin HM, Wayne PM (2018) What Is the point? The problem with acupuncture research that no one wants to talk about. J Altern Complement Med. 24(3):200-207.
[Crossref] [Google Scholar]
- Liu W, Fan Y, Wu Y, Hou X, Xue B, et al. (2021) Efficacy of acupuncture-related therapy in the treatment of knee osteoarthritis: A network meta-analysis of randomized controlled trials. J Pain Res. 14:2209-2228.
[Crossref] [Google Scholar]
- Cruz VB, Sousa ALL (2024) STRICTA and the traditional acupuncture paradigm: Time to update? J Healthc Commun. 9(1):12-17.
[Crossref] [Google Scholar]
- Napadow V, Ahn A, Longhurst J, Lao L, Stener-Victorin E, et al. (2008) The status and future of acupuncture mechanism research. J Altern Complement Med. 14(7):861-869.
[Crossref] [Google Scholar]
- Miller E, Maimon Y, Rosenblatt Y, Mendler A, Hasner A, et al. (2011) Delayed effect of acupuncture treatment in OA of the knee: A blinded, randomized, controlled trial. Evid Based Complement Altern Med. 2011:792975.
[Crossref] [Google Scholar]
- Lee S, Kim JH, Shin KM, Kim JE, Kim TH, et al. (2013) Electroacupuncture to treat painful diabetic neuropathy: Study protocol for a three-armed, randomized, controlled pilot trial. Trials. 14:225.
[Crossref] [Google Scholar]
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, et al. (2010) Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. J Altern Complement Med. 16(10):ST1-ST14.
[Crossref] [Google Scholar]
- Lu L, Zhang Y, Ge S, Wen H, Tang X, et al. (2022) Evidence mapping and overview of systematic reviews of the effects of acupuncture therapies. BMJ Open. 12(6):e056803.
[Crossref] [Google Scholar]
- Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Br Med J. 340:c332.
[Crossref] [Google Scholar]
- American Academy of Orthopaedic Surgeons (2022) Management of osteoarthritis of the knee (non-arthroplasty). Appropriate use criteria.
- Arden NK, Perry TA, Bannuru RR, Bruyere O, Cooper C, et al. (2021) Non-surgical management of knee osteoarthritis: Comparison of ESCEO and OARSI 2019 guidelines. Nat Revi Rheumatol. 17(1):59-66.
[Crossref] [Google Scholar]
- Fernandes L, Hagen KB, Bijlsma JWJ, Andreassen O, Christensen P, et al. (2013) EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 72(7):1125-1135.
[Crossref] [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev. 5:210.
[Crossref] [Google Scholar]
- R Core Team (2018) R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing.
- Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, et al. (2019) RoB 2: A revised tool for assessing risk of bias in randomised trials. Br Med J. 366:l4898.
[Crossref] [Google Scholar]
- Harrer M, Cuijpers P, Furukawa TA, Ebert DD (2021) Doing meta-analysis with R: A hands-on guide.
[Crossref] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis. Hoboken: John Wiley & Sons.
- Critical Appraisal Skills Programme (2018) CASP Randomised controlled trial standard checklist.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br Med J. 372(71).
[Crossref] [Google Scholar]
- Sangdee C, Teekachunhatean S, Sananpanich K, Sugandhavesa N, Chiewchantanakit S, et al. (2002) Electroacupuncture versus diclofenac in symptomatic treatment of osteoarthritis of the knee: A randomized controlled trial. BMC Complement Altern Med. 2:3.
[Crossref] [Google Scholar]
- Tukmachi E, Jubb R, Dempsey E, Jones P (2004) The effect of acupuncture on the symptoms of knee osteoarthritis-an open randomised controlled study. Acupunct Med. 22(1):14-22.
[Crossref] [Google Scholar]
- Liu Y, Wu H (2022) Effect of electroacupuncture on knee osteoarthritis and relevant inflammatory factors: A randomized clinical trial. World J Tradit Chin Med. 32(4):329-335.
[Crossref] [Google Scholar]
- Ho L, Ke FYT, Wong CHL, Wu IXY, Cheung AKL, et al. (2021) Low methodological quality of systematic reviews on acupuncture: A cross-sectional study. BMC Med Res Methodol. 21(1):237.
[Crossref] [Google Scholar]
- Jia P, Tang L, Yu J, Lee AH, Zhou X, et al. (2018) Risk of bias and methodological issues in randomised controlled trials of acupuncture for knee osteoarthritis: A cross-sectional study. BMJ Open. 8(3):e019847.
[Crossref] [Google Scholar]
- Xiu WC, Gang WJ, Zhou Q, Shi LJ, Hu XY, et al. (2024) Factors and their impact on treatment effect of acupuncture in different outcomes: A meta-regression of acupuncture randomized controlled trials. Chin J Integr Med. 30(3):260-266.
[Crossref] [Google Scholar]
- Birch S, Lee MS, Kim TH, Alraek T (2022) Historical perspectives on using sham acupuncture in acupuncture clinical trials. Integr Med Res. 11(1):100725.
- White P, Prescott P, Lewith G (2010) Does needling sensation (de qi) affect treatment outcome in pain? Analysis of data from a larger single-blind, randomised controlled trial. Acupunct Med. 28(3):120-125.
[Crossref] [Google Scholar]
- Lundeberg T (2013) To be or not to be: The needling sensation (de qi) in acupuncture. Acupunct Med. 31(2):129-131.
[Crossref] [Google Scholar]
- Chen FI, Antochi AD, Barbilian AG (2019) Acupuncture and the retrospect of its modern research. Rom J Morphol Embryol. 60(2):411-418.
[Google Scholar] [PubMed]
- Breivik H (2017) NSAIDs relieve osteoarthritis (OA) pain, but cardiovascular safety in question even for diclofenac, ibuprofen, naproxen, and celecoxib: What are the alternatives? Scand J Pain. 16:148-149.
[Crossref] [Google Scholar]
- Huang H, Luo M, Liang H, Pan J, Yang W, et al. (2021) Meta-analysis comparing celecoxib with diclofenac sodium in patients with knee osteoarthritis. Pain Med. 22(2):352-362.
[Crossref] [Google Scholar]
- Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, et al. (2004) Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: A randomized, controlled trial. Ann Intern Med. 141(12):901-910.
[Crossref] [Google Scholar]
- Kwak SG, Kwon JB, Seo YW, Choi WK (2023) The effectiveness of acupuncture as an adjunctive therapy to oral pharmacological medication in patient with knee osteoarthritis: A systematic review and meta-analysis. Medicine. 102(11):e33262.
[Crossref] [Google Scholar]
- Langevin HM, Wayne PM, MacPherson H, Schnyer R, Milley RM, et al. (2011) Paradoxes in acupuncture research: Strategies for moving forward. Evid Based Complement Alternat Med. 2011:180805.
[Crossref] [Google Scholar]
Citation: Cruz VB, Junger AL, Alves dos Santos DPM, Sousa ALL (2024) The Effect of Electroacupuncture on the Management of Pain and Articular Function Related to Primary Knee Osteoarthritis: Systematic Review and Meta-analysis. J Healthc Commun. 9:9013.
Copyright: © 2024 Cruz VB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.