Original Article - (2017) Volume 18, Issue 1
Marta Sandini1, Nicolò Tamini1, Pietro Allegranza2, Cammillo Talei Franzesi2, Davide Ippolito2, Luca Gianotti1
1School of Medicine and Surgery, Milano-Bicocca University, San Gerardo Hospital, Monza, Italy
2Department of Radiology, San Gerardo Hospital, Monza Italy
Received August 02nd, 2016 - Accepted September 12th, 2016
Introduction The safety and the protective role of stenting the pancreato-jejunal anastomosis on the occurrence of pancreatic fistula is debated. Aim of this study was to evaluate the outcome of patients who received internal stenting during pancreatoduodenectomy and to review the literature on the related complications. Methods From 2007 to 2014 we performed 207 pancreatoduodenectomies with endto- side duct-to-mucosa pancreato-jejunal anastomosis. We retrospectively analyzed the outcome of 38 high-risk patients with an internal stent through the pancreato-jejunal anastomosis. The occurrence and severity of pancreatic fistula were defined according to International Study Group of Pancreatic Fistula classification. We evaluated the fate and complications of the stents by radiological and clinical follow-up. A literature review was performed through web-search. Results No patients had stent-related symptoms or complications. Seven patients (18.4%) developed clinically relevant pancreatic fistula. We had a mean of 1.9±0.9 (SD) postoperative imaging exams for 33 patients. The median time of follow-up was 3 months (range 1-62). The stent was no longer visible in 17 patients (51.5%); in 8 cases (24.2%) it was in the pancreatic duct, in 7 (21.2%) migrated in the jejunal limb and in 1 patient into the colon. By literature review we retrieved 13 papers reporting on long-term outcomes of internal pancreato-jejunal stenting. Discussion Internal stenting does not seem to be associated with major long-term morbidity, but the short follow-up does not allow definitive judgment on the fate of the stents still in place or dislocated into the jejunal limb. Literature describes a low rate of complications, mainly hepato-biliary infections due to stent migration.
Fistula; Jejunostomy; Pancreatoduodenectomy; Review; Stents
CRPOPF clinically relevant post-operative pancreatic fistula; ISGPF International Study Group of Pancreatic Fistula; MPD main pancreatic duct; PD Pancreatoduodenectomy; PF pancreatic fistula; PJ pancreato-jejunal
Pancreatoduodenectomy (PD) represents the most complex procedure in abdominal surgery. Although perioperative mortality rate has significantly decreased over the years in high-volume centers [1, 2, 3, 4], PDrelated morbidity rate remains relatively high, ranging from 20% to 50% [5, 6].
Clinically relevant post-operative pancreatic fistula (CRPOPF) is the commonest complication [7, 8], potentially affecting patient recovery and quality of life and increasing total health-care costs [9]. Peculiar patient characteristics such as age, sex, pathology, body composition [10, 11, 12] and intrinsic features of the gland such as pancreatic texture and diameter of main pancreatic duct [13, 14] have been identified as major risk factors for CRPOPF. Pharmacological treatments to mitigate the CRPOPF rate have been suggested [15], and alternative surgical strategies such as pancreatogastrostomy [16], early drains removal [17] duct-tomucosa anastomosis [18], invagination technique [19], stapling off the transected stump of the pancreas [20] and omental wrapping [21], have been described but with poor reproducibility. Also, external and internal stenting of the main pancreatic duct (MPD) has been suggested as a technique to reduce the risk of POPF. Yet, studies on the fate and complications related to internal short stenting are sparse, reporting conflicting results and raising doubts on its safety [22, 23, 24, 25]. In fact, early and late complications such as cholangitis, hepatic abscess, small bowel obstruction, bleeding and pancreatitis have been anecdotally described as consequences of displacement of the internal MPD stent [26, 27, 28].
Since in our institution we routinely stent the MPD in cases of high risk of CRPOPF, the aim of this study was to retrospectively evaluate the long-term outcome of patients who received internal stenting during pancreatoduodenectomy and to review the available literature on the complications of this technique.
Patients
We retrospectively retrieved, from a prospectively collected database, all patients who underwent PD at our Institution from January 2007 to December 2014 and had an internal short stent placed in the MPD through the pancreato-jejunal anastomosis. Despite there were no formal and stringent indications for stenting, there was high agreement among pancreatic surgeons of our center to use internal stent in patients considered at high-risk for the development of POPF, i.e. the evidence during operation of a soft parenchyma and pancreatic duct diameter ≤3 mm in diameter. From the database we also obtained data on the postoperative outcome and the rate and severity of POPF onset, according to the ISGPF classification and grade B and C fistula were defined as clinically relevant.
Surgical Procedure
Whipple or pylorus-preserving PD was performed by three different experienced pancreatic surgeons with standardized procedures in all patients. A two-layer endto- side pancreato-jejunostomy with either Child or Rouxen- Y technique was used for reconstruction. The external layer (pancreatic parenchyma-to-the jejunal seromuscolar layer) was built with interrupted 3-0 polyglactin sutures, while the duct-to-mucosa layer was performed with interrupted 4-0 polydioxanone cardinal stitches. An internal polyvinylchloride (PVC) stent (Bracci type) was inserting across the duct-to-mucosa anastomosis and secured to the jejunal mucosa using one 4-0 polyglactin stitch in high risk cases. The size and length of the stent were selected according to the diameter of the MPD and the length of the pancreatic remnant. At the end of operation, two abdominal closed suction drains were placed: one next to the bilio-jejunal anastomosis and one closed to the pancreato-jejunal anastomosis. Continuous intravenous infusion of octreotide (600 mcg/day) was given to all patients starting during surgery and ending at the resumption of oral feeding.
Follow-Up
Up to December 2014, from our radiologic imaging server, we retrieved all the available exams (CT or MRI scan), performed for any purpose after patient discharge, in which reconstructions for upper and lower abdomen were included. Expert radiologists revised the scanning to describe the position of the stent, when present, and potential indirect signs of related complications. Patient clinical status was assessed at scheduled postoperative office visits or by telephone interviews. Follow-up was considered concluded in absence of radiological retrieval of the stent or at the latest available imaging.
A literature web search was performed using MEDLINE, Embase, PubMed, Scopus, Web of Science, and the Cochrane Library Medline from January 1990 up to June 2015. The following medical subjects search headings terms and all their possible combinations were used: “pancreatic resection”, “pancreatoduodenectomy”, “pancreatic fistula”, “postoperative fistula”, “complication” and “stent” “stenting”, “catheter”, “pancreatic duct”, “wirsung”. The “related articles” function and the references list of the studies retrieved for full-text review were used to broaden the search.
We did not perform a systematic review using the recognized domains and check-list, since the available reports did not provide sufficient methodological requirements for a formal systematic review.
During the study period we performed 207 PD. Internal stenting was carried out in 38 (18.4%) patients, with a median age of 74 years (range 45-85). Indications for PD were pancreatic adenocarcinoma (28/38, 73.7%), ampullary carcinoma (3/38, 7.9%), distal cholangiocarcinoma (4/38, 10.5%), duodenal carcinoma (2/38, 5.2%) and chronic pancreatitis (1/38, 2.7%). Five out of the 38 high risk patients were lost at follow-up for these reasons: one patient died during the postoperative course because of cardiac infarction and the other four underwent oncologic treatment in other centers and no radiologic imaging was retrievable.
The characteristics of the 38 patients studied are depicted in Table 1. Clinically relevant POPF occurred in 7 patients (18.4%). No evident correlation between the rate of CRPOPF and sex, age, pancreatic texture or main pancreatic duct diameter was observed, although the median diameter of the pancreatic duct diameter was smaller in patients who experienced CRPOPF (Figure 1). The incidence of CRPOPF was similar in patients with soft or hard pancreatic texture (Figure 2).
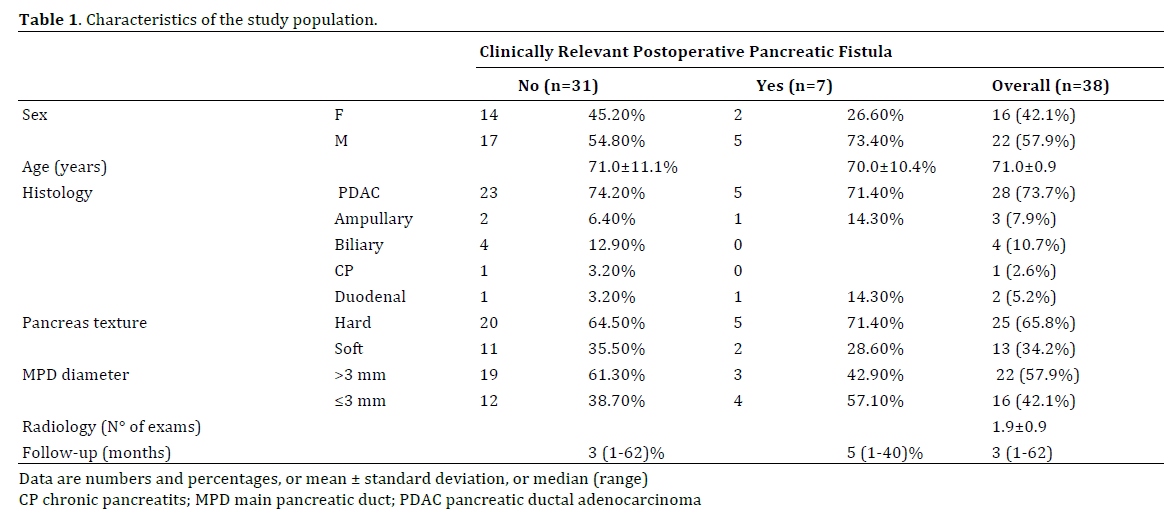
Figure 1. Diameter of the main pancreatic duct diameter according to the occurrence of clinically relevant post-operative pancreatic fistula. Median MPD diameter was 5 mm (IQR 3-6 mm) and 3 mm (IQR 2-7 mm) in those patients who did not experienced CRPOPF and who did, respectively. boxplot legend upper horizontal line of box: 75th percentile; lower horizontal line of box: 25th percentile; horizontal bar within box: median value; vertical line: minimum-maximum value
The median postoperative observation period was 3 months (range 1-62) for patients who had the stent ejected and 5 months (range 1-40) in subjects with the retained stant. Defecation of the stent was confirmed in 17 patients (51.5%). while 16 patients (48.5%) retained the stent. In 8/33 patients (21.2%) the stent was still in place, in 7/33 (18.2%) it was visible inside the lumen of the ileum and in one patient the stent was disrupted into two fragments inside the colon lumen.
No stent-related complications occurred during the follow-up period.
Table 2 summarizes the information on the 13 studies describing stent-related long-term complications. 53.8% (7/13) papers were case reports [28, 29, 30, 31, 32, 33, 34, 35] and the others were retrospective analyses [26, 27, 36, 27, 38]. In 5 studies the stent material was not reported, PCV tubes were used in 2 studies, silastic tubes in 5, and a Soft-flex stent in one case. Pancreatic internal stents were either free-floating (3/8) or anchored (5/8) with one or more stitches to the duct-jejunal anastomosis.
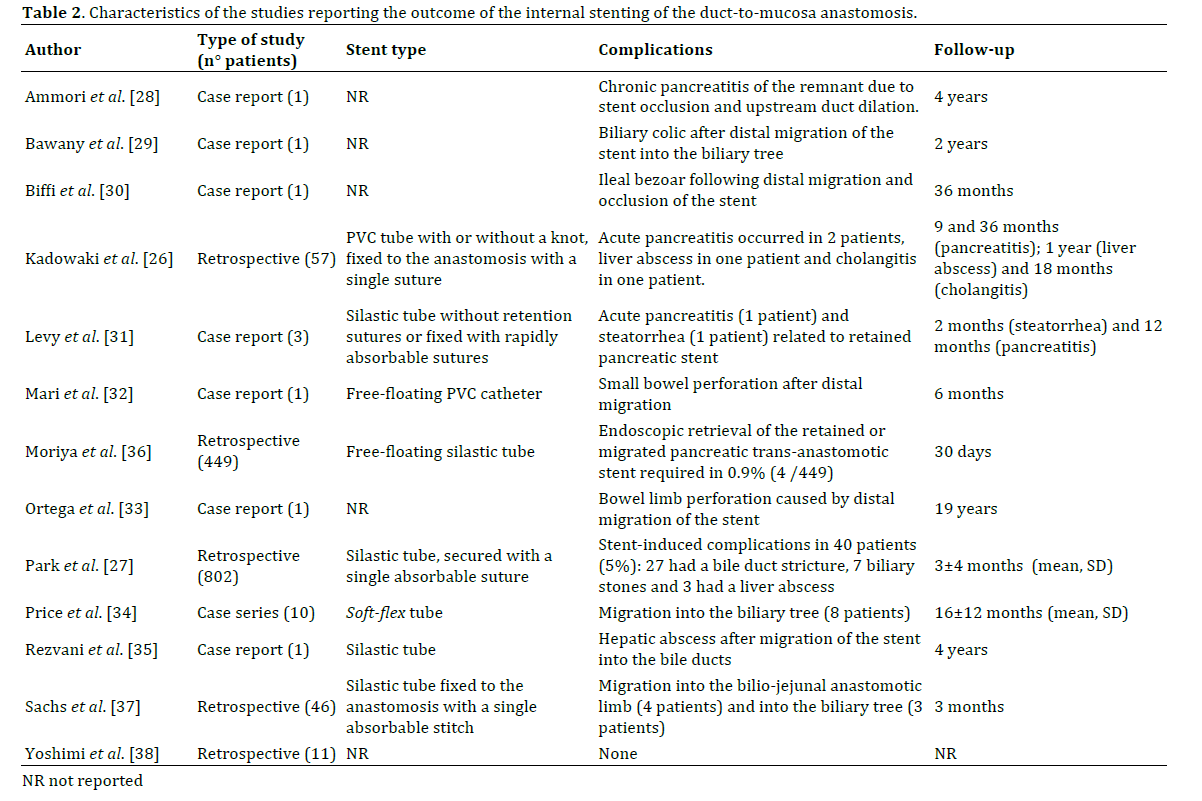
Regardless the type of study, the overall stent-related complication rate was 4% (55 out of 1365 patients) and were mainly hepato-biliary complication: cholangitis in 3 studies, migration without infection in 5 studies and pancreatitis in 3 reports.
Defecation of the stent was confirmed in all patients analyzed by Yoshimi et al. [38] by the 176th day after surgery and in 41% of the cases with a median time of 454 days in the report by Kadowaki et al. [26].
Long time retention of the stent in the bile system was the only factor associated with the onset of morbidity [27]. Complications occurred in a period ranging from 3 months to 19 years.
During the last decade the use and the value of transanastomotic pancreatojejunal stenting has been extensively debated. Stenting the main pancreatic duct may be useful for diversion of pancreatic juice, decompression of the pancreatic remnant and assuring the patency of the duct during the construction of the duct-to-mucosa layer. On the other side, internal stent may migrate into the biliary tree or the jejunum and account for severe complications [29, 30] whereas external stents may be uncomfortable for patient, can accidentally dislodge, and may represent the entry port for contamination and infection [23].
Four meta-analyses on randomized clinical trials have been published [39, 40, 41, 42]. Markar et al. [39] showed a trend towards a reduction of the rate of pancreatic fistula with the use of pancreatic stents in pancreato-jejunostomy. Dong et al. [40] observed that the use of external stents, when compared with no stenting, was associated with a significant reduction in the risk of pancreatic fistula, rate of delayed gastric emptying and wound infection, and a significantly shorter length of hospital stay. Similarly, Wang et al. [41] reported a reduction in the overall morbidity rate in case of external stent placing versus no-stent, while no differences was found by comparing internal stent versus no-stent, or internal versus external stent. However, some studies included in those meta-analyses preceded the ISGPF classification of POPF, limiting the reliability of such results for the lack of homogeneous definition and also because the prevention of grade A pancreatic fistulas has to be considered of partial clinical relevance. Thus, despite evidences faintly suggested that placing a stent across the pancreato-jejunostomy may reduce the incidence of morbidity, its use is not generally recommended or left to the surgeon habit.
At our Institution internal stent is the preferred strategy in case of high-risk anastomosis, i.e. in case of small pancreatic duct diameter or soft pancreata. Our data showed that the rate of CRPOPF in those selected patients was 18.4%, similar to those observed in our overall population (17.7% - data not shown) and to other centers [43]. Nonetheless, the present series includes patients operated before the publication of the most used clinical score to assess the fistula risk [13, 44] and consequently the assessment of each patient risk and the use of stenting were based on subjective surgeon judgment. When we analyzed potential risk factors associated with POPF, we did not observe a clear correlation between the MPD diameter and the rate of CRPOPF. Moreover, we observed that most of patients with CRPOPF had hard pancreata and most of patients with soft texture POPF did not experienced fistula formation. Similarly, Sachs et al. [37] observed a higher fistula rate in patients with hard texture and stent, and conversely a lower rate of CRPOPF in soft pancreata and no-stenting. The explanation of these results may lie in the potential traumatic effect of the stent on the pancreatic duct, leading to a local inflammation delaying the healing of the anastomosis. Likewise, ductal alterations were described in patients with a pancreatic stent placed for long periods [45].
We retrieved no stent-related complications during the follow-up period and the radiological imaging showed no related side effects in those patients who had the stent in place. Moreover, despite the relative high percentage of our patients with retained stent and hence with potentiality for detrimental effects, in most of our cases the stent was beyond the biliary anastomosis, suggesting an uneventful course. The present results are in accordance with the largest series by Park et al. [27] reporting an incidence of pancreato-jejunal stent migration in the bile ducts of 16.8%, with a rate of major related-morbidity of less than 1%. However, since the stent was still in place in 8/33 patients (24.2%) at the end of the follow-up period, no definitive judgment on the fate of those stents may be reached.
The appraisal of the retrieved studies suggests that complications may occur even years after the placement of an internal stent [28, 30, 33], however this result are not supported by studies with large cohorts, for the short follow-up period [27, 36]. Finally, except for anecdotal reports of unusual small bowel complications [30, 32, 33], most stent-related adverse events occurred for the migration to the biliary tree [26, 27, 34, 36, 37]. Since it has been observed that the probability of complication is associated with the persistence of the stent in a peripheral biliary duct, preventive removal of the migrated stent may be considered in selected cases [27].
Potential pitfalls of the present study are the limited number of patients, the short follow-up time, the retrospective design, and the lack of an objective fistula risk assessment. Additional investigation with a larger sample size and a priori definition of risk classes are needed.
In conclusion, internal PJ stenting does not seem to be associated with major long-term morbidity, but the short follow-up does not allow definitive judgment on the fate of the stents still in place or dislocated into the jejunal limb. Current evidences describe a low rate of complications mainly infections due to stent migration in the biliary tree. The potential protective role of MPD internal stenting in selected cases has to be assessed by properly designed randomized trials.
All authors declare having no conflict of interests or financial disclosures.