Research Article - (2016) Volume 24, Issue 3
Glorianne Pullicino*
Visiting Assistant Lecturer, Department of Family Medicine, University of Malta, Specialist in Family Medicine, Primary Health Care Department, Malta
Philip Sciortino
Specialist in Family Medicine, Head of Department and Visiting Senior Lecturer, Department of Family Medicine, University of Malta, Malta
Liberato Camilleri
Head of Department and Associate Professor, Department of Statistics and Operations Research, University of Malta, Malta
Willemijn Schäfer
Researcher, International Comparative Health Services Research Primary care, Netherlands Institute for Health Services Research, Malta
Wienke Boerma
Senior Researcher and Consultant, Netherlands Institute for Health Services Research, Malta
Corresponding Author:
Dr. Glorianne Pullicino
MD MSc MRCGP (Int) MMCFD, Visiting Assistant Lecturer, Department of Family Medicine, University of Malta, Specialist in Family Medicine, Primary Health Care Department, 36, ‘Roma’, Triq l-Alwetta. Mosta. MST4502, Malta
Tel: 79252218
E-mail: glorianneb@gmail.com
Submitted date: June 03, 2016; Accepted date: June 21, 2016; Published date: June 28, 2016
Background: Social homogeneity and an almost indiscernible rural-urban difference are generally assumed to be strong factors that reduce any tendency for health inequities in a small island community. A strong primary health care system is one of the components that protect populations against inequities.
Aim: The aim of this study was to examine healthcareseeking behaviour in urban and suburban regions in Malta.
Methods: The dataset of the Maltese arm of the QUALICOPC Project was analysed. A descriptive, crosssectional study was designed. Seventy practicing general practitioners were selected randomly from the Malta Medical Council Family Medicine register after systematically removing the inactive practices. Ten patients presenting quasi-randomly in each primary care clinic completed a selfadministered questionnaire. The chi-square test was used to test for differences in demographic and health care characteristics between the urban and suburban primary health care service. Generalized Linear and Latent Mixed Models (GLLAMM) were used to perform the multilevel analysis using Stata/SE version 12.
Results: None of the 4 predictors (patients’ primary or secondary educational level, age and gender) emerged to be significant for coping better with illness after GP visit. 82% of the total variance in this response (Yes/No) was between patients, 13% was between clinics and 5% between regions. General practitioners offered more health promotion services and asked more about polypharmacy when their patients were older.
Conclusion: Such findings provide information for policy makers to improve equity and resource allocations within the setting of urban Malta to help improve patients’ outcomes, particularly for the at-risk or vulnerable population.
Keywords
Primary health care; Public health; Quality of care; Health care organization and management
Background
It was thought that the assessment of quality was within the remit of health care professionals and researchers only. However, there is growing recognition that the views and preferences of patients are relevant.1-3 Several countries have adopted methods and strategies to measure patient experiences in order to monitor the performance of healthcare providers and to facilitate consumer choice.4-8 Several studies have measured patient experience in healthcare in general, but the literature pertaining to primary care (PC) is more limited.9
The small size of countries contribute to a socially homogenous population and an almost indiscernible rural-urban difference.10,11 It is thought that this homogeneity reduce the tendency for health and social disparities in a discrete geographically defined population as in island communities.10,12 Amongst epidemiologists, rural health inequalities have been a topical focus of attention and made a priority for policy led improvement.13,14 Inequalities are unavoidable but inequities are generally accepted to be socially unjustifiable or unacceptable.14,15 Despite the small geographical size of the islands, little is known about inequities in this area.10 Several methodological and conceptual problems arise when discussing rural-urban health inequities.10,16
In Malta, patients are “nested” within PC physicians who in turn are “nested” within specific regional practices in urban or suburban areas.17,18 Much of the international research data collected in practice-based research networks have similar patterns of nesting (clustering). Therefore, statistical approaches to the data must take into account the multilevel nature of the data or its interpretation could be jeopardized. Multilevel models show that the effects of physician-level activities may vary from clinic to clinic as well as between rural and urban settings. This variability would not be detected in traditional linear regression approaches. Such models also offer opportunities to explore contextual effects and differences across sites.19
The aim of this study was to examine healthcare-seeking behaviour in urban and suburban regions in Malta.
Methods
The target population was all patients attending PC clinics. Three major geographic regions were chosen and seventy general practitioners (GPs) were recruited. GPs were selected randomly from the Malta Medical Council Family Medicine register after systematically removing the inactive practices. ‘Inactive practices’ refers to GPs who were retired, working abroad, not practicing the specialty of Family Medicine or practicing outside the study areas. The study was conducted in four of five districts within Malta according to the NUTS classification.17 The urban and suburban regions were defined as considered in the EURO-URHIS project.20
Using convenience sampling, ten patients aged 18 years and older entering the GP waiting area, were invited to participate in the study. Only those patients who came to visit the participant GP were invited. Subjects had to fill in the questionnaire themselves or by means of assistance from a trained fieldworker but not someone else on behalf of the patient. Patients who came for solely an administrative procedure and those who were too sick to participate were excluded from this study. An overview of the methodology used in this study is shown in Figure 1.
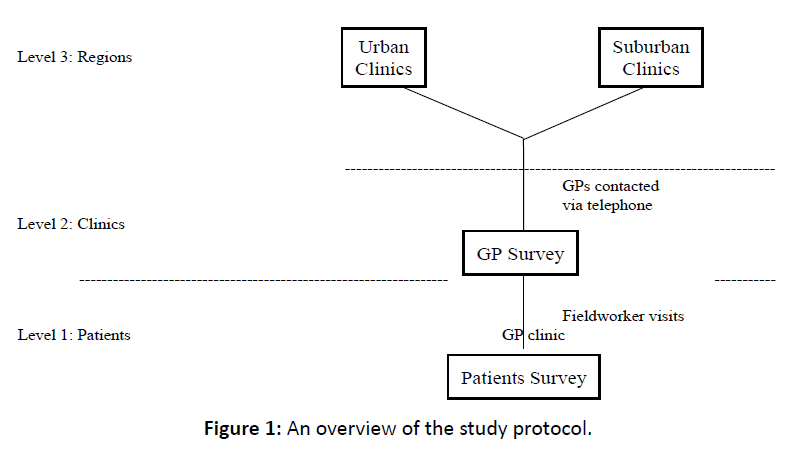
Figure 1: An overview of the study protocol.
The survey was conducted between 8 am and 9 pm to capture the whole range of service users. Patients’ consent was obtained. It was stressed that participation was voluntary, that the survey was anonymous and that participation or non-participation had no impact on the service provided. Participants were assured that their responses will be treated with strict confidentiality. The fieldworkers who were medical doctors checked the questionnaires for completeness, correctness and readability. It was made clear that answers could only be altered by the patient and not by the researchers. Patients were not allowed to take the questionnaire home.
We aimed to obtain 700 completed patients survey for the study. Using an online sample size calculator Pi-face for a confidence interval around a proportion, we considered the worst-case scenario and 50% proportion. With a sample of 700 patients, the confidence interval was +/-3.7%.
Measurements
A descriptive, cross-sectional study design was applied using the QUALICOPC Patients Experiences Questionnaire. The partners of the QUALICOPC consortium took several steps to develop and validate the questionnaires. A framework, which included important aspects regarding the process and outcomes of care, was defined. For the patient questionnaire the framework was based on the Consumer Quality Index of GP care.21
A pilot study was held in three countries in Europe (Belgium, the Netherlands and Slovenia) among a small sample of GPs and patients. GPs and patients were surveyed in the GP practice setting.9 The English version of the QUALICOPC questionnaire was translated into Maltese. A first translation was organized by a small team of people who were familiar with the PC practice in Malta and had a good understanding of English. A professional translator made an independent back-translation. Peer review indicated accepted face validity. Moreover, instrument development was further informed by focus groups. The researcher and the professional translator agreed on the final translated version. A pilot study was performed amongst fifty PC patients who did not form part of the sample. Further analysis indicated good test-retest reliability in both versions of the questionnaire.
Statistical Analysis
The chi-square test was used to test for differences in demographic and health care characteristics between the urban and suburban primary health care service. The data was analysed using the Statistical Package for Social Sciences (SPSS) version 20. Generalized Linear and Latent Mixed Models (GLLAMM) were used to perform the multilevel analysis using Stata/SE version 12.
Results
Seventy-eight GPs were invited to participate in this study. Eight of the latter did not consent to participate yielding an overall response rate of 88.6%. The response rates amongst the public and the private GPs were 94.3% and 82.9% respectively. A small remuneration was offered to the GPs. Amongst the private GPs who refused, four claimed that they were too busy to participate; another said that his patients would be very busy and another doctor claimed that his private clinic was too small for the fieldwork to occur. A public GP claimed that he was not interested in participating whilst another public GP was on long vacation leave during the time of the fieldwork. The patients’ response rate in this study was 73%. Reasons for patients’ non-participation included literacy issues, being too busy, disinterested or impatient.
The majority of the participants were females (61.9%, n=386). The sample population had an age distribution of 18-88 years with a mean of 48.2 years ± 17.6 years. 53% of patients (n=332) visited GP clinics in urban areas whereas 47% (n=294) attended PC clinics in suburban villages. The highest level of education completed by the majority of participants was secondary education (45.1%, n=282) while tertiary education was completed by 36% (n=225) of the participants. Table 1 shows the socio-demographic and healthcare service characteristics among primary care patients in urban and suburban clinics.
| Patients' Characteristics | Urban | Suburban | ||
|---|---|---|---|---|
| (n=332) | (n=294) | |||
| No. | % | No. | % | |
| Gender | ||||
| Female | 191 | 57.5 | 195 | 66.3 |
| Male | 140 | 42.2 | 98 | 33.3 |
| Level of Education | ||||
| Never went to school/ | 65 | 55.1 | 53 | 44.9 |
| Primary Education | ||||
| Secondary Education | 143 | 50.7 | 139 | 49.3 |
| Postsecondary/Tertiary | 123 | 54.7 | 102 | 45.3 |
| (E.g.: University) | ||||
| Age | ||||
| 15-29 | 63 | 19 | 47 | 16 |
| 30-44 | 80 | 24.1 | 86 | 29.3 |
| 45-59 | 88 | 26.5 | 81 | 27.6 |
| 60-74 | 75 | 22.6 | 57 | 19.4 |
| 75-89 | 26 | 7.8 | 23 | 7.8 |
| Patient's Experiences and Views | ||||
| In past 2 years, a GP from the | 105 | 50.5 | 103 | 49.5 |
| practice had asked about all | ||||
| the medications | ||||
| In the past 12 months, a GP | 95 | 52.5 | 86 | 47.5 |
| had talked about how to stay | ||||
| healthy | ||||
| Patients were able to cope better | 266 | 52.1 | 245 | 47.9 |
| with their health problem or illness | ||||
| after the GP visit | ||||
Table 1: Socio-demographic and healthcare service patients’ characteristics in urban and suburban primary care clinics.
Multilevel models showed that the effects of physician-level activities differed amongst clinics as well as between urban and suburban settings. Patients were asked whether in past 2 years, a GP from the practice had asked them about all the medications. 82% of the total variance in the responses (Yes/No) is between patients and 18% is between clinics. There was no variation between urban and suburban regions. Since the parameter estimate for each was positive, this indicated that the probability that the patient replied yes increased with an increase in age.
Log (p/1-p) = -1.4995 + 0.0599 primeduc - 0.3362 seceduc – 0.1147 sexpat + 0.0192 agepat
Health promotion was assessed by asking patients whether in the past 12 months, a GP had talked to them about how to stay healthy. 88% of the total variance in the responses (Yes/No) was between patients, 12% was between clinics and 0% between regions. Since the regression coefficient for each was positive, it indicated that the probability that the patient answered yes increased with an increase in age.
Log (p/1-p) = -2.5912 + 0.0041 primeduc - 0.0009 seceduc – 0.0420 sexpat + 0.0332 agepat
Patients’ outcome was assessed by asking them whether they were able to cope better with their health problem or illness after the GP visit. None of the 4 predictors (patient’s educational status, sex and age) emerged to be significant since their p-value exceeded the 0.05 level of significance. 82% of the total variance in the responses (Yes/No) was between patients, 13% was between clinics and 5% between regions.
Log (p/1-p) = 2.7570 - 0.0702 primeduc - 0.5101 seceduc – 0.5628 sexpat + 0.0204 agepat
Patients in suburban regions tended to be able to cope better with their illness after they visited their GP.
Discussion
International research showed a lack of health promotion by GPs in the elderly.22 Conversely, in the present study, older patients were more likely to receive health promotion advice. One may question whether there is the unmet need for such services in the younger population. It could also be that the younger patients regard themselves as being healthy and do not value or seek health promotion services. Nevertheless, there may still be a lack of these services in the elderly, as the need may be a lot higher in this population. This means that there may also be unmet needs amongst the elderly. PC services could be responding to patients with different age groups in sync with their demands.
Similarly, elderly patients were more likely to be asked about polypharmacy. Younger PC patients might not have chronic diseases since they might be managed in secondary care specialized clinics. Moreover, the GP could associate polypharmacy with old age. Challenges of polypharmacy in the PC patient population can be addressed by collaborating with a pharmacist who can review the patient’s medical records, make recommendations about low priority drugs or simplify regimes, for example, using long-acting medications, so that all tablets can be taken in the morning.23
Rurality can contribute to the vulnerability of patients with chronic diseases through geographical barriers, financial constraints and limited availability of healthcare professionals.24,25 Moreover, patients may feel culturally marginalized in the urban health care context particularly if health literacy is low.24 However, in the current study, patients in suburban regions tended to be able to cope better with their illness after they visited their GP. Qualitative systematic review and meta-synthesis postulated that rural communities supported long-term mutual doctor-patient relationships, feelings of a sense of belonging, self-reliant behavior and adaptation.24,25 In suburban Malta, it is unlikely for weather conditions or geographic distance to pose major barriers to access. These factors might mitigate feelings of vulnerability in suburban regions.24
Potential limitations were identified in this study. Due to time and resource constraints, PC activities occurring in private hospitals and during home visits were excluded from this study. This study did not capture general practice activities carried out by other healthcare professionals, hospital-based specialists, private independent community-based specialists and unregistered medical practitioners. Participation and recall biases could have occurred. Participants could have tried to answer in the way they believed the researcher or their GP wanted them to answer, rather than according to their own beliefs (the ‘halo effect’). Respondents could have altered their responses in reaction to the researcher’s presence or to the realization that they were being studied (the ‘Hawthorne effect’). A training session was delivered to all fieldworkers to try to limit the inter-observer bias.
In view of the fact that this was a cross-sectional study, it was not able to demonstrate causality. There might have been an overrepresentation of patients who are frequent users of PC services. The reported improvement in the suburban areas might be the result of the service responding to the GPs’ or the patients’ demands rather than needs. Moreover, need might have been unperceived by patients, for example, in mental illnesses, and therefore, might not have led to demand. This study did not assess whether the services in urban and suburban areas were cost-effective and grounded in evidence-based medicine. Future quantitative research can address these limitations to ameliorate resource allocation and use, achieve value for money and improve patient outcomes.
Conclusion
In our study, we have analyzed a data set related to PC patients’ experiences using multilevel modelling, which overcomes the limitations of normal regression models. Its findings would be useful to inform PC physicians, policy makers and health service researchers who aim to strengthen the primary health care system.
Ethical Approvals
The study was approved by the University Research Ethics Committee and the Data Protection Officer of the Primary Health Care Department.
Acknowledgement
The Malta College of Family Doctors and the Malta Foundation Programme supported this project.
Source Of Funding
This work was co-financed by the European Commission in the 7th Framework Programme under the Grant Agreement Number 242141.