- (2014) Volume 15, Issue 4
Simon Khagi, Muhammad Wasif Saif
Tufts Medical Center, Tufts University School of Medicine, Boston, MA, USA
Gastroenteropancreatic neuroendocrine tumors are a heterogeneous group of malignancies, characterized by varying degrees of biological activity and metastatic potential. A common thread between this wide mix of neoplasms has remained their sensitivity to hormonal modulation with somatostatin analogues. New analogues of somatostatin have been recently introduced and are beginning to shape a different picture of how we treat and monitor for response in patients with gastroenteropancreatic neuroendocrine tumors. Here we discuss three important abstracts presented at the annual meeting of the American Society for Clinical Oncology (ASCO) 2014 (#4107, #4108, and # 4111) that highlight the changing landscape of somatostatin-based therapy.
Carcinoid tumor; Lanreotide; Neuroendocrine tumor; Octreotide; Somatostatin
Gastroenteropancreatic neuroendocrine tumors (NET) remain a complex and heterogeneous subset of neoplasia to treat. Symptoms can vary depending on the location, subtype, and malignant potential of each lesion. Patients may present with symptoms of hormonal oversecretion with or without symptoms of mass effect on adjacent normal tissue. Neuroendocrine tumors can be characterized by assessing the proliferative rate of each tumor. Well differentiated tumors (grade 1 and grade 2) possess Ki-67 indexes of <2% to 20%, reflecting their benign biological behavior. Poorly differentiated (grade 3) NET usually have a Ki-67 index of >20% and behave in a much more malignant fashion with carcinoid symptoms being more pronounced through the secretion of vasoactive peptides [1].
Therapeutic options for gastroenteropancreatic NET depend on the size, location, symptoms and metastatic sites of each tumor. For a well circumscribed, localizable single lesion, surgery is potentially curative. However, in the setting of locally advanced or metastatic disease, the use of cytotoxic agents, targeted therapy and hormonally active agents become important modalities of treatment. For the purposes of this review, we will discuss somatostatin and its recently available analogues for the treatment of gastroenteropancreatic NET (Table 1). Treatment updates related to cytotoxic therapy and molecularly targeted agents have been reviewed by the authors in previous publications.
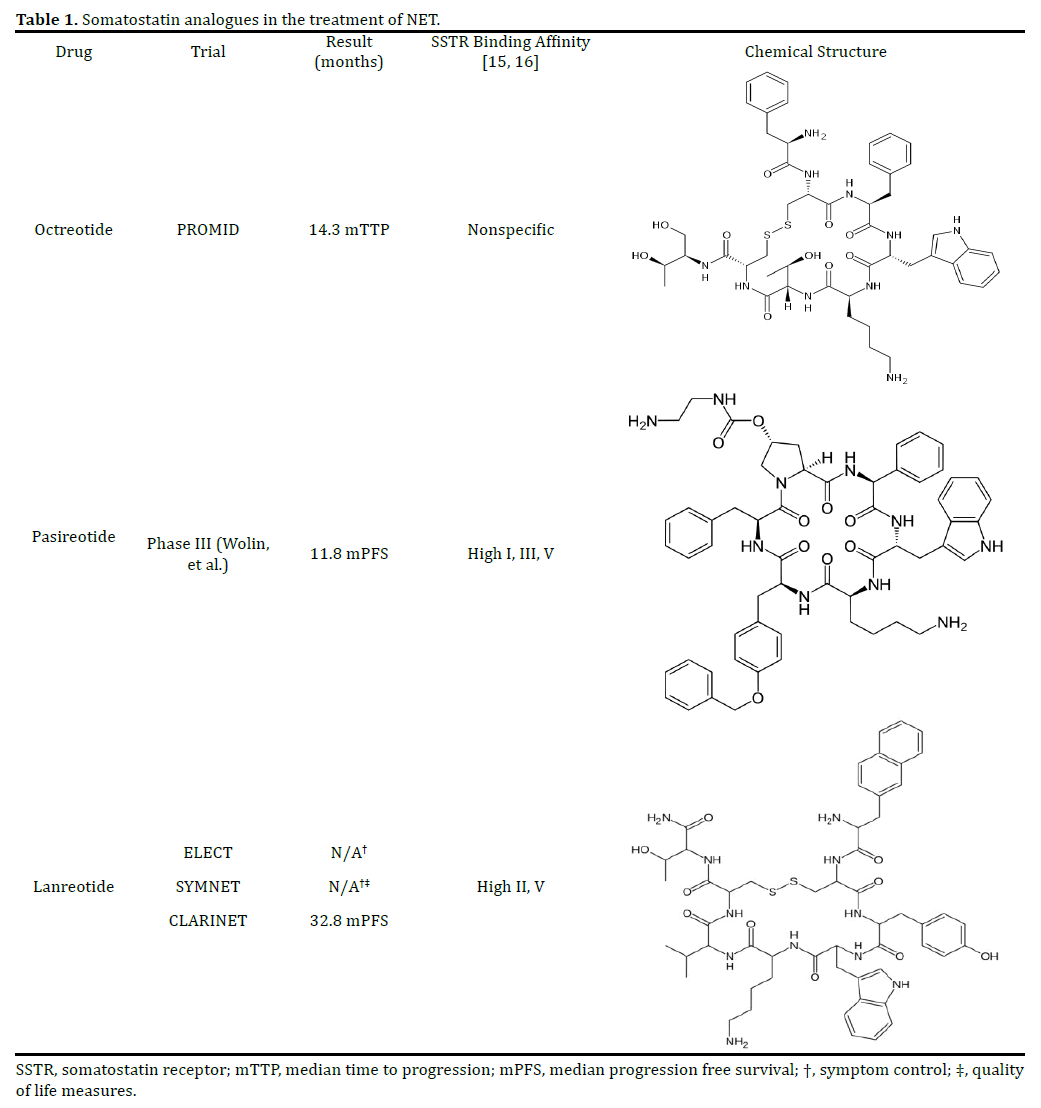
As noted in our recent review of the 2014 Gastrointestinal Cancer Symposium [2], somatostatin analogues have been used efficaciously to control carcinoid symptoms, as demonstrated by Rubin et al. [3]; however, the field has now evolved where somatostatin analogues are being used beyond the palliative setting with studies showing demonstrable improvement in parameters of survival. Among the first such trials, the PROMID (Placebo controlled, double-blind, prospective, Randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine MID gut tumors) study in 2009 demonstrated an improvement in median progression free survival (PFS) of 8.3 months with the use of octreotide 30 mg compared to placebo [4]. A subsequent follow up analysis of overall survival (OS) revealed that long acting octreotide improved overall survival; however, this benefit was mainly observed in patients with a low hepatic burden of disease [5].
Conjugated therapy with a somatostatin analogue and molecularly targeted therapy has been assessed with the combination of long acting octreotide and everolimus, a potent mTOR inhibitor. With the RADIANT-3 (RAD001 in Advanced Neuroendocrine Tumors) trial helping establish everolimus as a viable option for pancreatic NET management [6], the RADIANT-2 trial went on to combine the mTOR inhibitor with long acting octreotide in a phase III study. Median PFS was noted to be 16.4 months, compared to 11.4 months in the placebo and octreotide arm (HR = 0.77 P = 0.026) [7]. A follow up subgroup analysis of colorectal NET by the same group found that median PFS within this particular group was 29.9 months compared to 6.6 months in the placebo and octreotide arm (HR = 0.34, P = 0.011) [8].
Other somatostatin analogues have been evaluated recently. Pasireotide and lanreotide have been assessed in multiple phase III studies. Pasireotide was looked at in a phase III study comparing its efficacy to octreotide. Symptom control was comparable; however, pasireotide was shown to improve PFS by 5 months as compared to octreotide (11.8 months versus 6.8 months, P = 0.045) [9]. The ELECT trial evaluated lanreotide as a rescue therapy and compared efficacy versus octreotide (both long and short acting formulations) in a randomized, doubleblinded phase III trial. As reported by Vinik, et al., the study demonstrated a 15% absolute reduction in the use of the short acting rescue formulation of octreotide; however, pre-defined criteria were not met [10].
The CLARINET trial, reported at the European Cancer Congress 2013, also assessed lanreotide. The study focused on the antiproliferative effects of lanreotide in a phase III double blind; placebo controlled, and randomized trial. As reported by Caplin, et al., patients with well to moderately differentiated gastroenteropancreatic NET and one-third of patients presenting with >25% hepatic tumor load, were assessed over a period of two years. The study concluded that PFS, as measured by RECIST criteria, was significantly improved compared to placebo (median in lancreotide not reached versus 18 months with placebo, HR = 0.47 P = 0.0002). By two years, the lanreotide group had 62% of its participants still alive compared to 22% within the placebo arm [11].
We attended the annual meeting of American Society of Clinical Oncology 2014 and reviewed many presentations.
We chose to discuss here three abstracts that build on the known benefits of somatostatin analogues in the setting of gastroenteropancreatic NET. These studies varied from a retrospective review to an observational cohort analysis to a prospective follow up extension study. Needless to say, this year’s abstracts have broadened our knowledge in the field of gastroenteropancreatic NET.
The Association Between Octreotide Dose And Tumor Control In Gastroenteropancreatic Neuroendocrine Tumors
As reported by Lau, et al., this retrospective study based in British Columbia, Canada assessed 170 patients with NET originating predominately in the mid gut and pancreas. A large proportion of these tumors were further characterized by metastases, particularly to the liver (87%). Additionally, these tumors were noted to be vasoactive with a majority of patients (72%) manifesting carcinoid symptoms. Patients were stratified into those that had received < 27 mg (n=92) every 28 days versus > 27 mg (n=78) every 28 days of octreotide. Patients fared better who received > 27 mg compared to those who received < 27 mg of octreotide (median OS 82 months versus 39 months, respectively) [12].
Lanreotide Autogel/Depot Treatment for Carcinoid Syndrome Symptoms
In an observational, multinational study of patient reported outcomes (PRO), the authors of the SYMNET study evaluated the efficacy of lanreotide as it relates the management of carcinoid symptoms in 273 patients. The primary endpoint was control of diarrhea. Using two questionnaires to assess health-related quality of life (EORTC QLQ-C30 and GINET21), the group found that 76% of patients reported improvement in diarrhea control, with a median duration of treatment of 11 months. The authors went on to report that overall symptom management and quality of life measures improved as defined by PRO using the aforementioned questionnaires [13].
Progression Free Survival with Lanreotide Autogel/Depot in Enteropancreatic Nets Patients
As mentioned in the section preceding our discussion of this year’s abstracts, the CLARINET trial was a randomized, double-blind, placebo-controlled study assessing survival based on the proposed antitumor effects of lanreotide. The study was initially reported at the European Cancer Congress in 2013. As reported by Caplin, et al., the CLARINET extension study provides us with mature results related to PFS, as well as a look at safety over a five year period. As previously noted, the study enrolled patients with well to moderately differentiated tumors, with onethird of patients presenting with liver metastases. Roughly 200 patients were evenly distributed to receive either lanreotide or placebo. The extension phase of the study involved patients taking lanreotide with stable disease or patients who had either progressed or remained stable on placebo to enter into a single arm assessment period, which primarily looked at safety, and with a primary efficacy endpoint of PFS.
The study reported that 44% of the total study population enrolled into the extension phase, with roughly half deriving from the lanreotide and placebo arms, respectively. The most common adverse reaction was diarrhea. Median PFS for patients taking lanreotide in the extension period was 32.8 months. The previously reported median PFS for those in the placebo arm was 18 months. The authors went on to report that patients, who had switched to lanreotide from placebo, had a median time to progression of 14 months following the initiation of lanreotide [14].
The study of somatostatin analogues in the management of gastroenteropancreatic NET remains an active area of research. These agents remain the mainstay of therapy, as cytotoxic therapy can be reserved in refractory cases of NET. This year’s ASCO abstract symposium provided us with a closer look at octreotide and lanreotide, with varying viewpoints of how to assess for response and efficacy.
Although, the use of octreotide has been established in the literature as a first line agent in the treatment of symptomatic gastroenteropancreatic NET, convincing data suggesting a PFS and OS advantage had been limited to the PROMID trial. Furthermore, the dose of long acting octreotide has not been fully established. The Lau, et al. abstract gave us important insights into what an optimal dosing regimen should be when treating metastatic gastroenteropancreatic NET. A dose of > 27 mg every 4 weeks appeared to be most efficacious [12], with a survival advantage far exceeding figures reported in the PROMID trial. With that said, the Lau study is a retrospective cohort analysis with limitations in its ability to generalize the results and control for certain confounding variables. Additional information would have been welcome as it related to patients with measurable hepatic disease burdens, since a lower disease burden portended an improved overall survival based on PROMID results [5].
Data regarding patient reported outcomes, particularly the frequency of diarrhea, was the focus of the SYMNET trial. Although a novel approach to measuring efficacy of lanreotide, this observational cohort analysis did not have a control arm. Nor did it account for other medications that patients may have taken for symptom relief (i.e. loperamide) throughout the course of the study. The primary measure of diarrhea seems to also conflict with the known adverse reaction that patients report while being on somatostatin analogues [2]. Although, it is encouraging to note that a majority of patients experienced less diarrhea from their baseline; however, this again, brings to mind the possibility of these patients were using other pharmacologic means to offset the effects of lanreotide, carcinoid symptoms, or both while enrolled in this study.
The extension to the CLARINET trial, as reported by Caplin et al., suggests that lanreotide provides patients with symptom relief, as well as a survival advantage. The study goes on to report a PFS and OS advantage for patients who were started and continued on lanreotide; however, OS was also assessed in placebo group subjects who had crossed over into the lanreotide arm of the study as part of the extension phase. This may confound the results as they relate to OS, but it does appear that lanreotide provided a survival advantage in this patient group via an objectively evaluable method (i.e. RECIST criteria).
Taken together, this year’s abstracts suggest that patients suffering from gastroenteropancreatic NET may have multiple options of somatostatin analogues to choose from. However, based on what has been presented, it appears that octreotide continues to warrant its front line status. Further research is needed to elucidate if there is truly an advantage of using lanreotide in place of octreotide for the treatment of gastroenteropancreatic NET.
The authors have no potential conflicts of interest.