Keywords
Innate immunity; Adaptive immunity; Vitamin; Steroid hormone biosynthesis; Drug metabolism; Inflammatory bowel disease; Obesity; Atherosclerosis; Neurodegenerative diseases; Fecal transplantation
Introduction
The basic aspects of molecular and cell biology are not only integral part of biomedical research but are also translated into patient care. Several global consortia have been launched and in part completed during the last decades. All of them continuously transform basic biomedical research and translate into medical applications and, after evaluation in randomized clinical trials, enter clinical practice with a tremendous potential to advance the diagnosis, treatment and prevention of human diseases.
More than 15 years ago, the international Human Genome Organization (HUGO) project established the complete sequence of the ca. 3 billion base pairs that make up the human genome. The data from the HUGO project greatly contributed to the understanding of disease pathogenesis and the individual patient’s natural course, prognosis and response to therapy (‘personalized/precision medicine’). In 2005 the international haplotype map (HapMap) project was initiated to identify, based on Genome-Wide Association Studies (GWAS) single nucleotide polymorphisms (SNPs) and their association with specific human diseases and individual phenotypic characteristics, respectively.
Overall, GWAS allow an increasingly better understanding of disease pathogenesis and a more accurate assessment of the individual risk to develop a specific disease.
The Human Microbiome Project
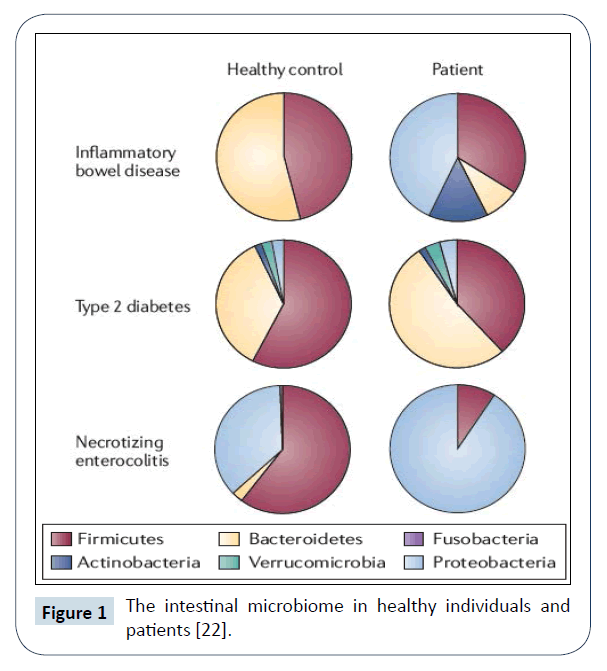
The Human Microbiome Project (HMP) was established in 2007 as a third global consortium [1]. It aims at the sequencing of all microbes (eukaryotes, archaea, bacteria, viruses) inhabiting human body sites, such as the mouth, throat and airways, stomach and intestine, the urogenital system and the skin, respectively. Recent data demonstrate that specific compositions of the microbial community are associated with health and disease and suggest that the detailed characterization, function and variation of the microbial community will reveal important commensal host-microbe as well as microbe-microbe interactions with pathogenetic, diagnostic, therapeutic and preventive implications [2,3]. HMP has meanwhile developed into a major field of biomedical research, in particular the intestinal microbial community (Figure 1) that turned out to play a major role in human health and disease [4].
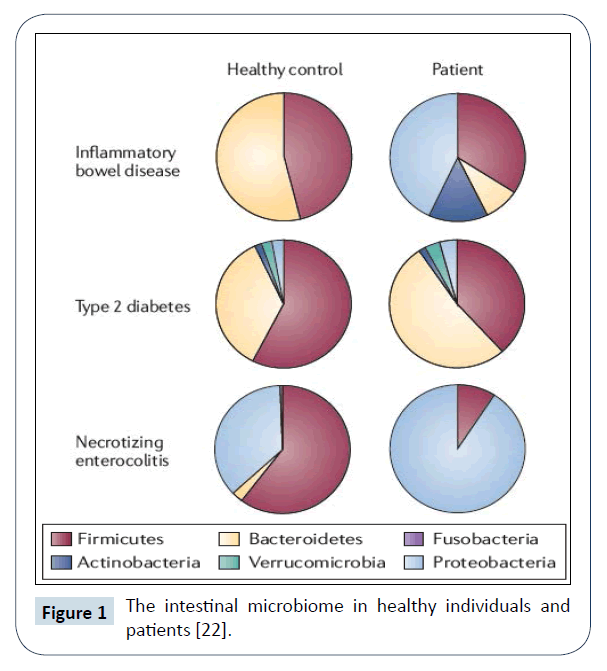
Figure 1: The intestinal microbiome in healthy individuals and patients [22].
The Intestinal Microbial Community
The intestinal microbial community represents a microbial ecosystem consisting of a trillion microbial cells with an aggregate 9.9 million microbial genes across the fecal microbiome [5]. While the environment in utero has been considered sterile, DNA-based analyses identified bacterial species in maternal placenta, amniotic fluid and meconium. The colonization of the human gut begins at birth with a rapid expansion of bacterial diversity and is characterized by a successively changing composition that eventually becomes relatively stable in adulthood. Important factors for the composition of the intestinal microbial community are endogenous and exogenous factors. Examples are mode of delivery of the neonates, diet (dietary supplements, breastfeeding, formula-feeding), xenobiotics, including antibiotics and other drugs. Further, infections and exposure to environmental microbial agents are established risk factors for childhood diseases, such as obesity and allergy [6]. Recent evidence further suggests that human genetic variation also influences the abundance of specific members of the intestinal microbial community.
In view of the numerous and diverse physiological functions of the intestinal microbiota in human health (Table 1) it is not surprising that it is also involved in gastrointestinal as well as non-gastrointestinal diseases, such as obesity/metabolic syndrome, and atherosclerosis/cardiovascular as well as neurologic/ psychiatric diseases, making it one of the most dynamic current topics in biomedical research (Table 2). In the following, a few examples will be briefly discussed.
| Host Physiology |
Biosynthesis |
Metabolism |
| Adaptive immunity |
Neurotransmitters |
Dietary components |
| Autoimmunity |
Steroid hormones |
Bile salts |
| Innate immunity |
Vitamins |
Drugs |
| Cell proliferation |
- |
Xenobiotics |
| Bone density |
- |
- |
| Vascularization |
- |
- |
| Neurological signalling |
- |
- |
Table 1: Functions of the intestinal microbial community in human health (examples).
| Allergies/Allergy protection |
| Atherosclerosis/Thrombosis/Cardiovascular Disease |
| Cancer |
| Diabetes mellitus |
Immune-Mediated Inflammatory Diseases
• Inflammatory bowel diseases
• Multiple sclerosis
• Rheumatoid arthritis
• Psoriasis |
| Kwashiorkor |
| Liver Diseases |
| Metabolic Syndrome/Obesity |
Neurodevelopmental, psychiatric and neurodegenerative diseases
• Autism
• Depression
• Alzheimer’s Disease, Parkinson’s Disease |
Table 2: Disease associations with the intestinal microbial community (examples).
Inflammatory bowel diseases and colon cancer
The inflammatory bowel diseases (IBD) in humans include Ulcerative Colitis (UC) and Crohn disease (CD). These are characterized by inflammation limited to the mucosal layer of the colon in UC and the transmural involvement of the gastrointestinal tract, including extra intestinal sites in CD. While the pathogenesis of IBD is not fully understood, it is clear that its pathology depends among others on the intestinal microbial community [7].
The three components-environments, host genetics and the microbial community-interact to maintain homeostasis in the intestine. The disruption of the stability of this interaction may be a trigger for disease development. Two recent publications shed a new light on the pathogenesis of IBD through the change of the intestinal microbial composition involving helminth infection [8] and lipocalin-2 expression [9], respectively.
While donor feces have been shown to be effective for the treatment of recurrent Clostridium difficile infection [10,11], recent randomized controlled trials demonstrated that fecal microbiota transplantation can induce clinical remission and endoscopic improvement in patients with active UC and is associated with distinct microbial changes that relate to outcome [3,12,13]. Fecal microbiota transplantation, therefore, may be a novel therapeutic option for UC and an alternative to standard drug treatment.
Further, it was recently discovered that the probiotic Lactobacillus casei strain ATCC 334 produces ferrichrome that inhibits colon cancer progression by apoptosis mediated through the c-Jun N-terminal kinase pathway [14], possibly representing a novel tumor-suppressing strategy.
Obesity
Obesity [15], insulin resistance [16] and khwashiorkor [17] are examples for which a correlation between microbial dysbiosis and the clinical state has been demonstrated. Further, in genetically susceptible hosts, the transplantation of fecal microbiota from healthy donors to patients resulted in clinical improvement. The underlying concept is a ‘common ground hypothesis’ that involves a leaky mucosa caused by various endogenous or exogenous factors, and the expansion of opportunistic microbes (dysbiotic pathobionts) which generate pathogenic gene products that can be transferred to genetically susceptible individuals [4].
Atherosclerosis and thrombosis risk
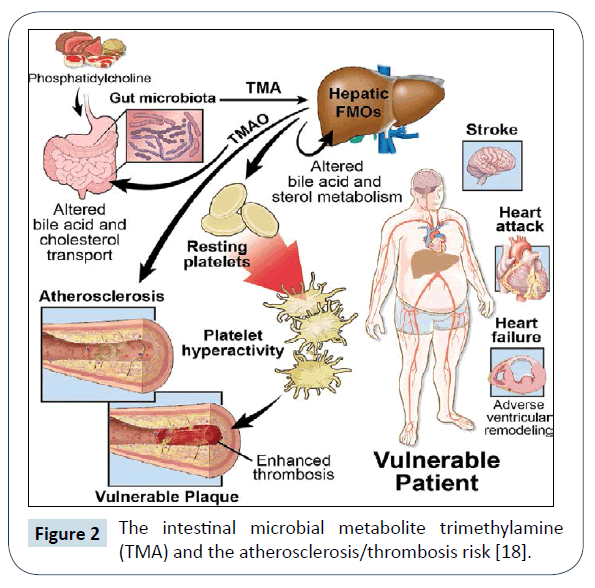
Interestingly, recent studies suggest that intestinal microbes are involved in atherosclerosis. In this context, foods rich in choline, phosphatidylcholine and carnitine such as meat, egg yolk and high-fat dairy products, serve as precursors of Trimethylamine (TMA) and TMA N-oxide (TMAO) that accelerates atherosclerosis and elevated TMAO blood levels are associated with an increased risk for atherosclerotic heart disease and incident major adverse cardiac events. Further, TMAO enhances platelet hyper reactivity and thrombotic events in studies of animal model, employing dietary choline or TMAO, germ-free mice and microbial transplantation, collectively confirming the key role of intestinal microbiota [18]. Taken together, these results reveal a previously unknown link between specific dietary nutrients, intestinal microbes and atherosclerosis/thrombosis risk (Figure 2).
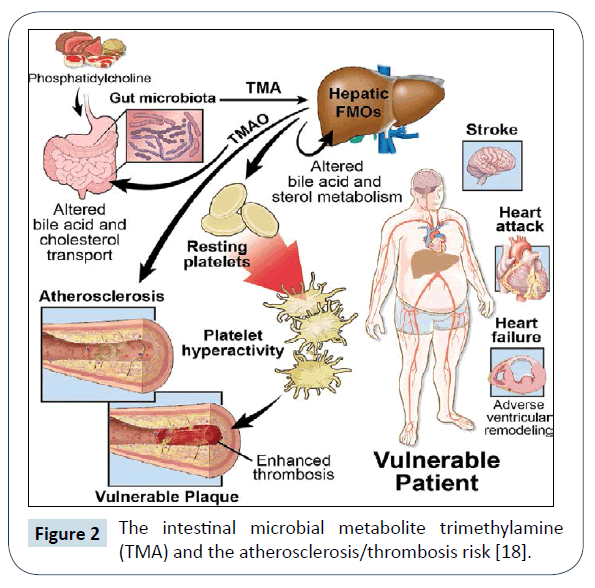
Figure 2: The intestinal microbial metabolite trimethylamine (TMA) and the atherosclerosis/thrombosis risk [18].
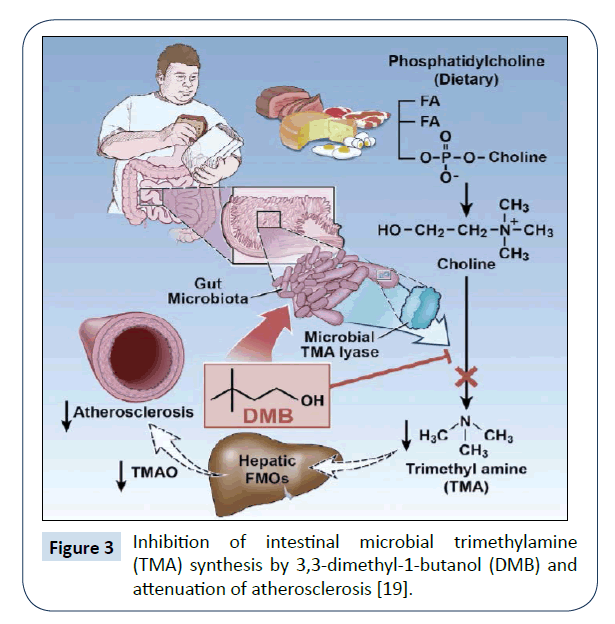
The intestinal TMAO formation is a two-step process involving the generation of TMA by intestinal microbes after food ingestion and the hepatic conversion of TMA to TMAO by host flavin Monooxygenase. In a recent, study Wang et al. [19] demonstrated that 3,3-dimethyl-1-butanol (DMB), a structural analog of choline, blocks the intestinal TMA formation through the inhibition of the microbial TMA lyase, and results in reduced TMAO levels. Thus, ‘drugging the microbiome’ with DMB may be a novel approach for the prevention/treatment of atherosclerosis (Figure 3).
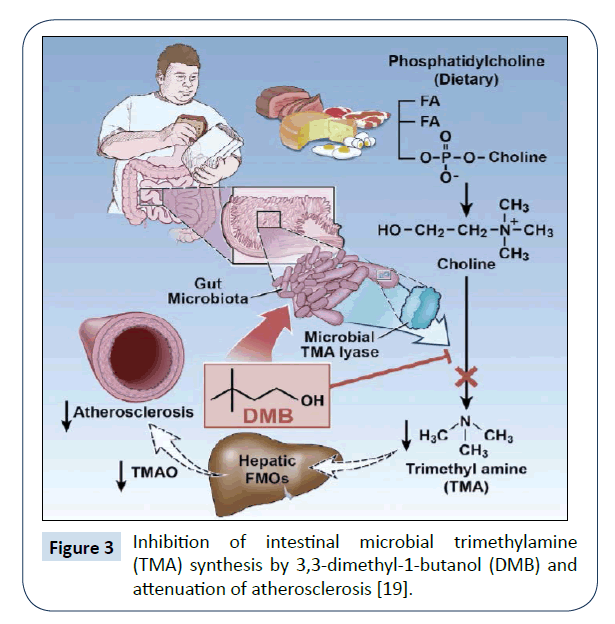
Figure 3: Inhibition of intestinal microbial trimethylamine (TMA) synthesis by 3,3-dimethyl-1-butanol (DMB) and attenuation of atherosclerosis [19].
Neurodevelopmental, psychiatric and neurode-generative diseases
Studies investigating the intestinal microbial-brain communication (gut-brain axis) demonstrate a critical role of the intestinal microbial community in modulating the maturation and function of tissue-resident immune cells in the Central Nervous System (CNS) as well as the activation of peripheral immune cells involved in neuroinflammation, brain injury, autoimmunity and neurogenesis [20]. Germ-free mice raised under sterile conditions or mice depleted of their intestinal microbiota by antibiotics show major alterations in behaviours or neuropathologies that characterize neurodevelopmental, psychiatric and neurodegenerative disorders. These include among others autism spectrum disorders, depression and Alzheimer’s or Parkinson’s disease (Table 2).
An impressive example for a pathogenic role of the intestinal microbial community is Parkinson’s disease (PD). In patients with PD, plaques in brain cells as well as in the intestine containing the neurotoxic protein Alpha-Synuclein (AS) are a hallmark of the disease. For example, in PD patient’s gastric motility is frequently impaired and AS levels in the intestine is elevated.
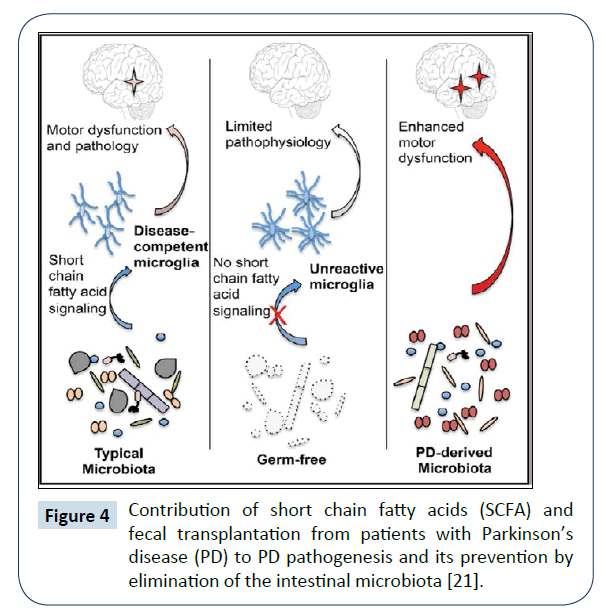
In an animal model, mice overexpressing AS indeed develop neurologic deficits resembling those of patients with PD. Recently, three lines of evidence demonstrated a central role of the intestinal microbial community in the pathogenesis of PD (Figure 4): (1) In the PD mouse model germ-free animals developed fewer plaques and almost no neurological deficits as compared to conventionally colonized controls, (2) Treatment of PD mice with antibiotics resulted in an improvement of the neurological deficits and (3) Fecal transplantation from patients with PD to germ-free mice resulted in neurological deficits resembling PD [21].
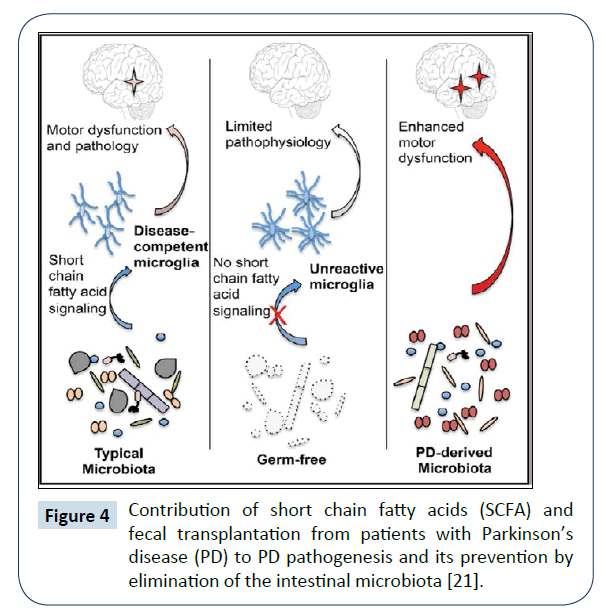
Figure 4: Contribution of short chain fatty acids (SCFA) and fecal transplantation from patients with Parkinson’s disease (PD) to PD pathogenesis and its prevention by elimination of the intestinal microbiota [21].
The underlying concept is the central contribution of the microbial community to a defect of the microglia via short-Chain Fatty Acids (SCFAs) that represent bacterial fermentation products. While germ-free mice showed a reduced microglia, SCFAs modulate microglia and enhance PD pathophysiology [22]. The identification of the disease-causing bacteria and the mechanism leading to the deposition of the neurotoxic AS plaques await further clarification.
Conclusion and Perspectives
Basic biomedical research has made major advances in recent years and holds the promise to increasingly provide individual diagnostic, preventive as well as therapeutic options for patients with inherited or acquired, malignant or non-malignant diseases. In this context the individual microbial community is central for the barrier between microbes and hosts and is involved in a large number of normal biological physiological functions in health, such as for example (Table 1). Importantly, the intestinal microbiome is central in the pathogenesis of numerous common, gastrointestinal as well as non-gastrointestinal diseases, such as obesity/metabolic syndrome, atherosclerosis/thrombosis or neurodevelopmental, psychiatric and neurodegenerative diseases (Table 2). Dietary interventions targeting intestinal microbiota, such as calorie restricted diets rich in fiber and vegetables as well as fecal microbial transplantation are examples for health benefits in humans. In recent years, the intestinal microbiome thus has become one of the most dynamic areas of biomedical research and holds an enormous potential for interventions regarding human health and disease.
Acknowledgement
The excellent secretarial assistance of Mrs. Mariette Gutgsell is gratefully acknowledged.
References
- Human Microbiome Project (2012) A framework for human microbiome research. Nature 486: 215-221.
- Morgan XC, Segata N, Huttenhower C (2013) Biodiversity and functional genomics in the human microbiome. Trends Genet 29: 51-58.
- Rossen NG, Fuentes S, van der Spek MJ, Tijssen JG, Hartman JH, et al. (2015) Findings from a randomized controlled trial of fecal transplantation for patients with ulcerative colitis. Gastroenterology 149: 110-118.
- Lynch SV, Pedersen O (2016) The human intestinal mMicrobiome in health and disease. N Engl J Med 375: 2369-2379.
- Li J, Jia H, Cai X, Zhong H, Feng Q, et al. (2014) An integrated catalog of reference genes in the human gut microbiome. Nat Biotechnol 32: 834-841.
- Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, et al. (2016) Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Nat Med 22: 1187-1191.
- Kostic AD, Xavier RJ, Gevers D (2014) The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology 146: 1489-1499.
- Ramanan D, Bowcutt R, Lee SC, Tang MS, Kurtz ZD, et al. (2016) Helminth infection promotes colonization resistance via type 2 immunity. Science 352: 608-612.
- Moschen AR, Gerner RR, Wang J, Klepsch V, Adolph TE, et al. (2016) Lipocalin 2 protects from inflammation and tumorigenesis associated with gut microbiota alterations. Cell Host Microbe 19: 455-469.
- van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, et al. (2013) Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 368: 407-415.
- Youngster I, Russell GH, Pindar C, Ziv-Baran T, Sauk J, et al. (2014) Oral, capsulized, frozen fecal microbiota transplantation for relapsing Clostridium difficile infection. JAMA 312: 1772-1778.
- Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, et al. (2015) Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology 149: 102-109 e106.
- Paramsothy S, Kamm MA, Kaakoush NO, Walsh AJ, van den Bogaerde J, et al. (2017) Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet 389: 1218-1228.
- Konishi H, Fujiya M, Tanaka H, Ueno N, Moriichi K, et al. (2016) Probiotic-derived ferrichrome inhibits colon cancer progression via JNK-mediated apoptosis. Nat Commun 7: 12365.
- Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, et al. (2013) Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341: 1241214.
- Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, et al. (2016) Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 535: 376-381.
- Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, et al. (2014) Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature 510: 417-421.
- Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, et al. (2016) Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell 165: 111-124.
- Wang Z, Roberts AB, Buffa JA, Levison BS, Zhu W, et al. (2015) Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell 163: 1585-1595.
- Fung TC, Olson CA, Hsiao EY (2017) Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci 20: 145-155.
- Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, et al. (2016) Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson's disease. Cell 167: 1469-1480.
- Spor A, Koren O, Ley R (2011) Unravelling the effects of the environment and host genotype on the gut microbiome. Nat Rev Microbiol 9: 279-290.