Original Article - (2016) Volume 17, Issue 3
Anwar Ahmad, Stalin Dharmayan, Nicolae Bostan, Mrinway Barua, Abraham Abiodun Ayantunde
Department of Surgery, Southend University Hospital, Prittlewell Chase, SS0 0RY, Essex, United Kingdom
*Corresponding Author:
Abraham Abiodun Ayantunde
Department of Surgery
Southend University Hospital
Prittlewell Chase, SS0 0RY, Essex
United Kingdom
Phone +01702435460
Fax +01702385856
E-mail biodunayantunde@yahoo.co.uk
Received November 11th, 2015 - Accepted December 30th, 2015
Introduction Acute idiopathic pancreatitis remains a challenge with no available strong recommendations. Its impact on patient outcome is not clear. This study compared the outcomes between patients with idiopathic pancreatitis and acute non-idiopathic pancreatitis. Methods A retrospective analysis of electronic prospectively maintained database of all episodes of acute pancreatitis over a 4-year study period. Patients’ clinicopathological data for hospital admissions were collected. Primary end points were organ failure, intensive care unit admission, pancreatic necrosis and mortality. Data analysis using SPSS version 19.0 with Chi-square test and unpaired Student t-test comparing the outcomes between idiopathic pancreatitis and non-idiopathic pancreatitis with p-value <0.05 set as statistically significance. Results 569 episodes of acute pancreatitis were recorded in 446 patients during the study period. The median age for all episodes was 62 (13-100) years with 264 males and 305 females. 142/569 (25%) and 427/569 (75%) were idiopathic pancreatitis and non-idiopathic pancreatitis respectively. Both groups were similar in their pre-admission co-morbidities (p=0.77) and demographics except for a preponderance of female patients in the idiopathic pancreatitis (63%) compared to the idiopathic pancreatitis (51%) (p=0.012). 21/142 (15%) patients with IP had overall poor outcomes compared with 30/427 (7%) in the non-idiopathic pancreatitis group (odds ratio 2.29; 95% confidence interval 1.27-4.16; P=0.006). Significantly poor outcomes noted in idiopathic pancreatitis compared with non-idiopathic pancreatitis for pancreatitis specific mortality (odds ratio 3.17; confidence interval 1.408-7.180; P=0.004), intensive care unit admission (odds ratio 2.73; confidence interval 1.36-5.46; P=0.003) and multi-organ failure (odds ratio 2.97; confidence interval 1.36-6.49; P=0.004). Conclusions Outcomes is significantly poor in idiopathic pancreatitis and this reflects our lack of understanding of the mechanisms of pancreatitis in this group of patients. We need rigorous management pathway to optimise their investigations and management.
Keywords
complications; Gallstones; Hereditary pancreatitis; Intensive care units; Mortality; Multiple organ failure
Abbreviations
CI confidence interval; MRCP magnetic resonance cholangiopancreatography; IP idiopathic pancreatitis; ITU intensive care unit; NIP non-idiopathic pancreatitis; OR odds ratio
INTRODUCTION
Acute pancreatitis is a severe disease with considerable morbidity and mortality. The incidence of acute pancreatitis is rising with mortality rate ranging between 3-10% [1, 2]. In 12-25% of patients, no cause is identified after initial diagnostic evaluation [1, 3, 4]. The group of patients in which after thorough history, physical examination, laboratory investigations and non-invasive imaging modalities no cause of pancreatitis is found is designated as having “Idiopathic Pancreatitis”.
Investigations employed to identify the cause of pancreatitis range from laboratory tests, non-invasive abdominal ultrasound scan (USS) and Magnetic resonance cholangiopancreatography (MRCP) to interventional investigations such as endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP). With these extensive evaluations, it is possible to identify the etiology in some of patients previously designated as having IP [5]. Identifying a cause in these patients is important, not only because it helps to direct treatment but also to improve the long-term prognosis by preventing recurrence.
The study evaluated the true reflection of the burden of idiopathic pancreatitis (IP) in our practice by comparing its outcomes with all other aetiological factors of pancreatitis. We also highlighted the areas needing improvement in the management of this challenging condition: the lost tribe of pancreatitis.
METHODS
A retrospective analysis of electronic prospectively maintained database in a District General Hospital was carried out. All episodes of acute pancreatitis between January 2011 and December 2014 were included in the study. Diagnosis of pancreatitis was based on raised serum amylase levels of at least greater than three times normal value. All patients had an initial abdominal USS to diagnose or exclude biliary pancreatitis. Patients with initial diagnostic uncertainty and/or those with complications of pancreatitis had computerized tomography (CT) scan and/or MRCP. Patients in whom no cause of pancreatitis could be determined after detailed history, laboratory investigations and imaging were labelled as having acute idiopathic pancreatitis (IP). Patients for whom a cause of pancreatitis was found were labelled as non-idiopathic pancreatitis (NIP). All patient episodes were scored using the modified Glasgow scoring system to predict severity during the admission episode. Patients requiring organ support were managed on either intensive care unit or high dependency unit.
Endpoints
Primary end points were organ failure, ITU admission, pancreatic necrosis and mortality. Significant organ failure was defined as deterioration in organ function compared to pre-admission state and patients requiring organ supports were admitted to ITU or at least to HDU bed. The diagnosis of pancreatic necrosis was made after confirmation on CT scan.
Data Collection and Statistics
Data on patient demographics, co-morbidities, length of hospital stay, ITU admission, organ failure, complications, interventions and mortality was collected. The data was analyzed using SPSS version 19.0 (SPSS, Chicago, Illinois, USA). Statistical significance was determined using Chisquare test and unpaired Student t-test comparing the outcomes between IP and NIP. Results were considered significant if p-value was <0.05.
RESULTS
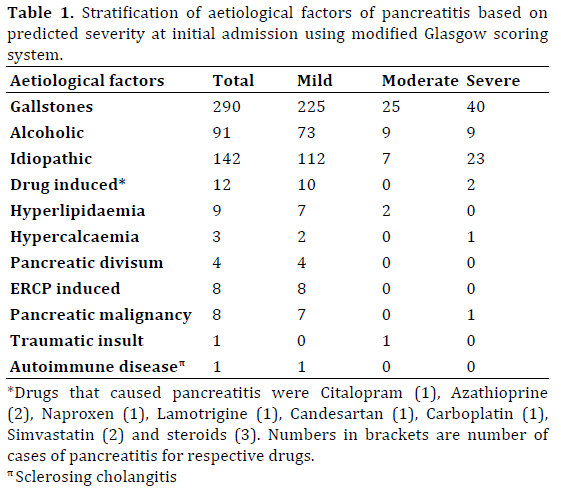
During the 4-year study period 569 episodes of acute pancreatitis were recorded in 446 patients (Table 1). The overall median age for all episodes was 62 (13-100) years with 264 males and 305 females. Out of all the episodes 142/569 (25%) were diagnosed as being IP and 427/569 (75%) were diagnosed as NIP. Both groups were similar in their pre-admission co-morbidities (p-value=0.77) and demographics except for a significantly higher incidence of female patients diagnosed with IP (63%) compared to the NIP group (51%; p-value=0.012). Clinicopathological factors are shown in Table 2.
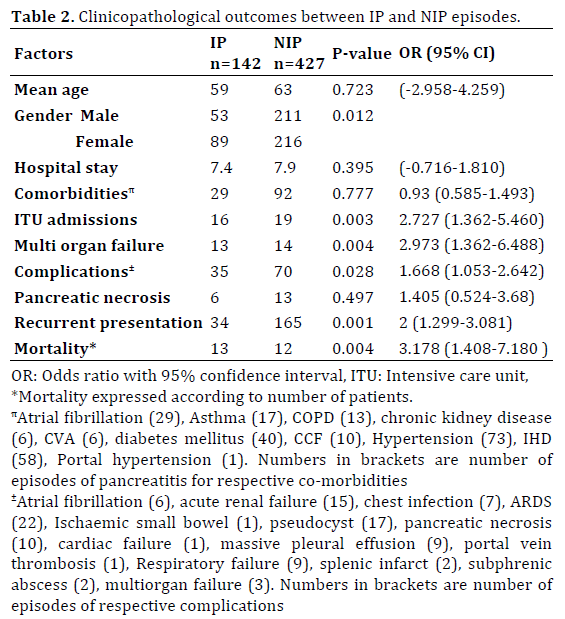
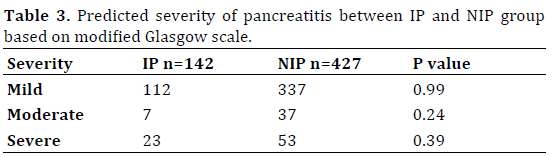
The severity of pancreatitis was equally distributed between the two groups (p-value=0.216; Table 3). Patients with NIP had a higher re-admission rate compared with the IP group (p-value=0.001). The overall median hospital stay was 6 (1-60) days with no difference between the two groups. The outcomes between the two groups are summarized in Table 3. The laboratory parameters between the two groups were similar except the liver function tests that were worse for the NIP group.
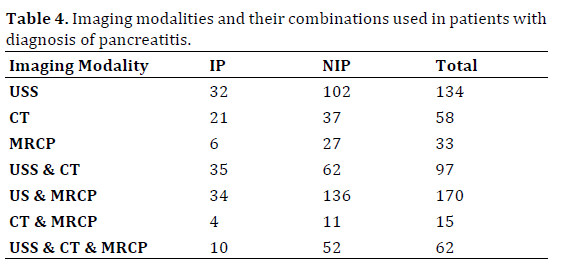
Abdominal ultrasound scan was the most commonly used imaging modality (81%) with equal distribution between the two groups (IP 78% vs. NIP 82%). The least commonly utilized imaging modality was MRCP (49%) and it was used for a significantly higher number of patients in the NIP group (IP 38% vs. NIP 53%) mainly to exclude biliary tract stone before cholecystectomy. Many patients had more than one investigation done at various episodes of their admission (Table 4).
Importantly, 21/142 (15%) episodes of IP had overall poor outcomes compared to 30/427 (7%) episodes in the NIP group (OR 2.29; 95% CI 1.27-4.16; p-value=0.006). Pancreatitis specific mortality was significantly worse in the IP group compared with NIP group (OR 3.17; CI 1.408-7.180; p-value=0.004), as was ITU admission (OR 2.73; CI 1.36-5.46; p-value=0.003) and multi-organ failure (OR 2.97; CI 1.36-6.49; p-value=0.004). The total overall pancreatitis specific mortality was 5.6% (25/446).
DISCUSSION
Patients with idiopathic pancreatitis have worse outcomes when compared with NIP group. The diagnostic dilemma in IP not only impacts on patient outcomes but also puts significant burden on healthcare facilities and resources as shown in our study with increased admissions to ITU and multi-organ failure needing supports.
The incidence of idiopathic pancreatitis varies between 12-25% [1, 3, 4]. Although the current UK guidelines aim for less than 20% of patients to be diagnosed with idiopathic pancreatitis [6], yet our cohort had a slightly higher incidence of IP. A possible explanation for this could be because EUS and/or ERCP with manometry were not used in the evaluation of our patients labelled as IP. Although this would have been ideal, yet in the settings of many District General Hospitals like ours where these facilities are not readily available, such limitations may have to be accepted as part of the normal practice. At our institute, ERCP was only done for proven obstructive jaundice and the aim is always that of therapeutic intervention. We have no facility for ERCP manometry.
Although the outcomes in patients with IP were significantly worse for multi-organ failure, overall complications and mortality, yet readmission rates in this group of patients was significantly better than the NIP group. We suspect this trend may have been due to the higher proportion of gallstone induced acute pancreatitis in the NIP group who did not undergo cholecystectomy at the first admission and/or within 2 weeks of admission as recommended by the UK guidelines for the management of gallstone pancreatitis [6].
Patients with idiopathic pancreatitis have been a focus of various investigations to determine the hidden aetiological factors in this peculiar group in the past. With the advent of EUS and ERCP with manometry, many underlining pathological factors have been linked with a possible cause for idiopathic pancreatitis. These include microampullary lesions, micro-choledocholithiasis, gallbladder micro-lithiasis, pancreatic divisum and sphincter of Oddi dysfunction [7]. The theories about possible detachment of gallbladder polyps causing obstruction of pancreatic duct have also been postulated [8]. In addition, genetic defects have also been implicated as a cause of IP [9, 10]. For all the structural pathologies EUS, MRCP and ERCP with manometry would suffice but possible link between gene mutations and idiopathic pancreatitis remains difficult to establish on routine clinical practice. This aspect has been raised in the recent guidelines published by the International Association of Pancreatology (IAP) where they have suggested considering genetic counselling after a second attack of idiopathic pancreatitis [11]. The place of genetic testing has not been well determined but may then be considered in specialized centres where there is a positive family history after recurrent attacks of acute idiopathic pancreatitis [9, 10].
We deliberately looked at the episodes of pancreatitis in this study as each episode is a separate financial burden and clinical episode in the same patient can present with different severity of pancreatitis on different episodes.
Current published literature strongly suggests the use of minimally invasive techniques such as EUS to be employed prior to getting to the diagnosis of idiopathic pancreatitis [7, 12]. Based on a recent review by Wilcox et al. EUS should be the first investigation to be considered for evaluation of patient in whom aetiology of pancreatitis has not been identified after routine investigations and cross-sectional imaging [13]. The non-availability of EUS at our institute remains an inevitable limitation in our study.
A relatively more invasive investigation like ERCP with or without manometric measurements has also been utilized for establishing a cause for pancreatitis. A study by Testoni et al. suggested decreased rates of recurrent idiopathic pancreatitis after ERCP and pre-emptive sphincterotomy, thereby suggesting a role of ERCP in all patients diagnosed with idiopathic pancreatitis [14]. Similar results for the diagnostic use of ERCP in idiopathic pancreatitis were also suggested in another study where 79% of patients with IP were found to have a cause for pancreatitis after ERCP [5].
Although ERCP service is available at our institute but it was not mandatory prior to making a diagnosis of IP. However, it must be emphasized that if ERCP is to be used to identify a cause of pancreatitis, sphincter of Oddi manometry should also be available in order to make the full use of its diagnostic ability as sphincter of Oddi dysfunction may be responsible for up to a third of all the cases of previously diagnosed IP [2]. This again is a specialized investigation that is not easily available in most District General Hospitals.
Based on the published literature mentioned above and our current results, we therefore suggest that a deep consideration should be given to the use EUS and/or ERCP with manometric measurements in patients with idiopathic pancreatitis. This submission is also supported by two randomized controlled trials, which compared EUS and ERCP in the settings of choledocholithiasis and did not show any significant difference in complications between the two groups [15, 16]. However, no trials have been done to compare effectiveness of investigations like contrast CT, EUS and ERCP in patients with IP.
A regular link with a specialist hepatobiliary unit by means of a monthly multidisciplinary meeting may be invaluable for District General Hospitals. This will not only provide the means to discuss these complicated cases but will also provide an opportunity to direct access to specialized investigations like EUS and ERCP with manometry. Also, lack of emphasis on the use of EUS in the current UK guidelines for the management of acute pancreatitis [6] does not compel most clinicians to try for the investigations that are not routinely available in their own institutes. These multidisciplinary meetings may also provide an opportunity to refer patients with recurrent attacks of idiopathic pancreatitis for genetic counseling.
Our study is a true reflection of the burden of acute pancreatitis in a typical District General Hospital and IP group is truly a lost tribe that tends not to get much attention it deserves. We have highlighted the importance of establishing aetiological factors in acute pancreatitis and the need for revisiting the current UK guidelines on this subject in order to develop evidence based pathways for patients with idiopathic pancreatitis.
Conflict of Interest
The authors have no potential conflicts of interest.