Research Article - (2015) Volume 23, Issue 5
Bromley GP and GP Education Lead Bromley CCG, UK
Dr Simon A Tavabie. MB BS BSc
FY2 Trainee Brighton and Sussex NHS Trust, UK
Background: Workforce redesign is needed in general practice to recognise the health and social needs of an ageing population with complex co-morbidities. Developing new roles for existing receptionists is presented as one way to support clinicians in administration of complex care, reducing unplanned hospital admissions for housebound patients.
Aim: To implement a patient liaison officer role in primary care through development of receptionist skills to support housebound patients in the community
Design: A longitudinal retrospective cohort study, following 64 housebound patient over 2 years, before and after introducing a patent liaison officer. Setting: South London general practice with 7200 registered patients
Method: Audit of unplanned hospital admissions; Accident and Emergency (A&E) and Urgent Care Centre (UCC) attendance by house bound cohort, 12 months before and after introduction of a patient liaison officer, using computerised clinical records and hospital discharge reports to identify contacts
Results: Unplanned hospital admissions reduced by 50%, without concurrent increase in separate A&E and UCC attendance.
Conclusion: Early indicators suggest a non-clinical liaison role within general practice, improving communication and care-coordination between patients, carers and external agencies, can support housebound patients resulting in reduced unplanned hospital admissions and potentially reduced health inequality.
Patient liaison; general practice; care co ordination
How this fits in with quality in primary care?
What do we know?
Housebound patients represent particularly vulnerable groups in society[1-5], often experiencing inequalities in care through poorly co-ordinated provision for complex health and social needs. Vulnerable patients often need help to co-ordinate care input from increasing numbers of provider organisations. This is despite having named general practitioners (GPs) and use of care plans intended to improve health outcomes.
New roles are emerging to signpost and support patients (often serving those who are able to self-care, or with specific health needs, particularly cancer and mental health)[17,18]. The needs of those unable to self care, whose continued independent living is reliant on effective integrated care, requires sustained input. This is ideally suited to a liaison role in general practice, where they might also support the general practitioners’ role in continuity of care and care administration. Little has been published, to date, on the outcome of a new liaison role in general practice.
What does this paper add?
This new role fits with the agenda for adult safeguarding, promoting safer independent living in the community and reducing unplanned hospital admissions.
It supports integrated care, led through general practice, which is ideally placed to identify patients at risk, and implement protective care plans.
The patient liaison officer presents a viable and economically favourable way to support GPs in coping with increasing workload from vulnerable patients unable to self-care, concurrently developing the role of an existing workforce in general practice and giving a direction for their future career development.
Survival into old age is often accompanied by increasing frailty; disability and comorbidity, with significant numbers losing mobility and becoming housebound.[1-5] Potentially isolated and less able to access care or self-care, this population is particularly vulnerable, relying heavily on support from voluntary carers and multiple care agencies in order to maintain independent living, avoiding institutional care.
Integrated care with good coordination can both improve wellbeing for individuals and reduce unplanned hospital admissions.[6-10] Conversely, poor co-ordination of care between providers is often a cause of unnecessary suffering and breakdown of support for vulnerable members of our community, leading to potentially avoidable hospital admission and institutionalisation[11]. With an ageing population, surviving with multiple long-term conditions, the requirement for effective communication between multiple clinical and social care agencies, together with patient and carer engagement, is a priority for the UK National Health Service (NHS), driven by both population and economic needs [12-14]. Traditionally, general practitioners (GPs) have undertaken holistic provision of care, holding comprehensive patient records that place them in an ideal position to ensure that care is both monitored and effective. However, an out of hospital agenda; increasing workload, and expansion of the generalist role for GPs means that it is no longer feasible for GPs to shoulder this responsibility alone. New roles are evolving to support GPs, many of which focus on concepts of self-care and patient empowerment which underpin the NHS Five Year Forward View.[15] In this paper, the role of a patient liaison officer in general practice is considered as a way of supporting clinicians in care of the most vulnerable, housebound patients, often unable to self-care and having complex care issues associated with degenerative and long-term conditions.
The concept of a patient liaison officer acting as the patient’s advocate is not new and has been widely used in secondary care settings (PALS - Patient Advisory Liaison Service).[16] However, their function has largely been to resolve complaints rather than prevent problems before they occur. In general practice, patient liaison officers have the potential to implement care plans designed by clinicians, ensuring that providers of care for individuals are communicating effectively with, and through the practice. A similar role of care navigator has been developed more widely for signposting and care facilitation, but has tended to focus on specific contexts, particularly cancer and mental health, with navigators coming from diverse backgrounds (nursing; social care and lay people) and working in a variety of settings.[10,17,18] In this study, the liaison officer role is an administrative role, developed through training of existing general practice reception and secretarial staff, with pre-existing local knowledge of patient populations and inhouse services; experience in dealing with patient requests by telephone and face-to-face contact, alongside the ability to use practice computer systems. They received additional training in communication; record keeping; facilitation of carers’ groups and case conferences; information about local services and providers.[19](Appendix 1) and were expected to demonstrate these capabilities, as defined in their job description (Appendix 2).The role was implemented, and evaluated in the authors’ practice.
The aims of this study were to identify ways in which the patient liaison officer might improve care for housebound patients, reducing unplanned hospital admissions through facilitating preventative action, supporting the out-of-hospital and integrated care agenda.
A housebound patient was defined as someone who was not in institutional care but was unable to leave their home independently, normally only accessing health care through home visits, or with total dependency on carers to attend the practice.
The study took place in one practice in South London which serves a predominantly Caucasian middle-class suburban population, and had 4 regular GPs throughout the 2 years. The practice had a registered patient list of 6685 at the outset, and 7263 at the end of the study, with the increase being largely from a younger age group. 1275 (19.1%) were aged over 65yrs at the outset (641(9.6%) over 75 yrs), and 1310 (18.1%) aged over 65yrs at the end of the study (652 (9.0%) over 75yrs). The practice had a longstanding policy of regular planned home visits to housebound patients and surgery assessments for those who could be brought to the surgery by relatives or carers, with case-finding through opportunistic consultations (face to face or telephone) and review of hospital discharge letters. The development of care plans by GPs with housebound patients began in 2011-12 through discussion between GP, patient and carers, addressing social, psychological and physical problems that might impact on the patient’s ability to remain living independently in the community. Each problem was listed and agreed, with actions points; named key agencies, carers and review dates. This format continued throughout the study.
During 2012-3 patient liaison officers underwent training in a workshop format (Appendix 1)[19], and from May 2013, worked with GPs to manage administrative aspects of care plans for housebound patients. This involved follow through of identified action points, such as engaging support from other agencies; prompting regular reviews; telephone or e-mail contacts with the patient and carer(s), and encouragement for carers to attend the established practice carers’ group. They met weekly with the GP to debrief and agree further actions. The liaison role deliberately avoided clinical responsibility, recognising their non-clinical background. However, their additional training in communication enabled them to develop effective relationships with patient and external care agencies.
This was a longitudinal retrospective cohort study, of 64 patients identified as housebound but living independently, with care plans developed within the practice during 2011-2012, followed over 2 years, to include one year where the care plan was managed by GP and patient, (2012-2013) and one year with the patient liaison officer additionally managing administrative aspects of the care plan (2013-2014). Patients were excluded if they died during the study; moved away from the practice or into residential care. Patients were also excluded where care plans were developed by agencies outside the practice, where there was minimal, or no, opportunity for the practice to influence them such as those with exclusive psychiatric conditions and those receiving tertiary care services for transplant and cancer care.
Current evidence suggests that upwards of 17% of the UK population is aged over 65 years, and that approximately 17% of these would meet the criteria for being housebound, equating to 2.9% of the total population.20 Housebound patient needs for patient liaison officer input were expected to vary over time, and between individuals. As such, a patient liaison officer was employed for 7 hours each week, representing an estimated 2 hours time for each housebound patient per annum, including both the study cohort and increasing numbers of other housebound patients identified through active case finding at the time.
In September 2013, a pilot patient satisfaction survey (Appendix 3) was sent to the first 30 patients where the patient liaison officer had contacted both the patient and their main carer, where the main carer was not from a statutory body. Information was anonymous and used as feedback on acceptability of the new role to patients and potential future development.
At the end of April 2014 hospital admissions and attendances for the year prior to introduction of the patient liaison officer, and the year with a patient liaison officer in post for the study cohort were audited. Computerised patient records were analysed for attendance at Accident and Emergency centres(A&E); Urgent Care Centres(UCCs) and unplanned urgent hospital admission, with review of referral or discharge letters by the authors to identify the prime reason for attendance / admission.
Care plans were analysed to identify health and social issues experienced by the study cohort to highlight common problems.
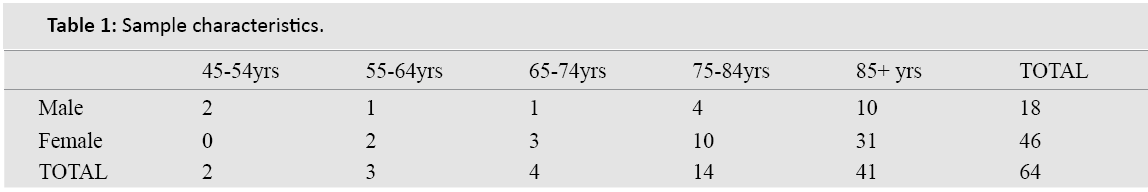
Initially, 78 housebound patients were identified as meeting entry criteria for the study. 14 of these patients died during the second year of the study, leaving 64 as the study cohort who was followed for the two years from 1st May 2012 - 30th April 2014. Age at 30th April 2014 ranged from 51-98yrs, with 65% (41 patients) being over 85yrs (Table 1). There was a 5:2 ratio of female to male patients (46:18). Care plans revealed multiple combinations of health problems (minimum 3 per patient). The most common problems identified were: heart disease (heart failure; angina; atrial fibrillation); falls; diabetes; COPD/asthma; anxiety/depression; memory problems/dementia; poor mobility; cancers; medicines concordance and uncontrolled pain.
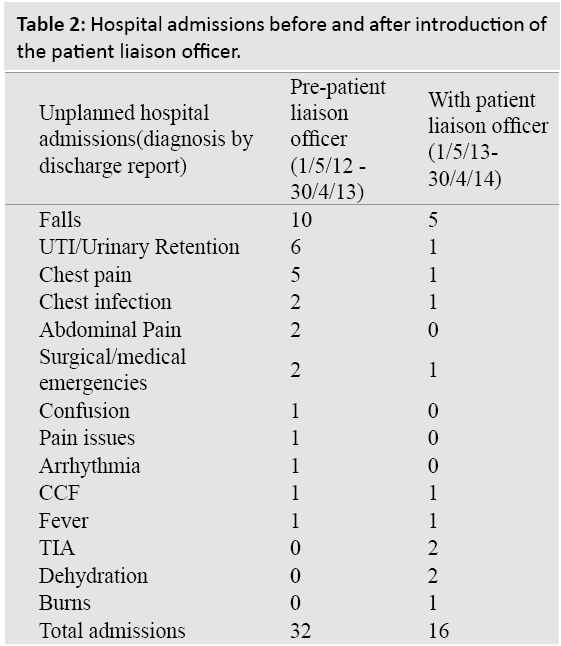
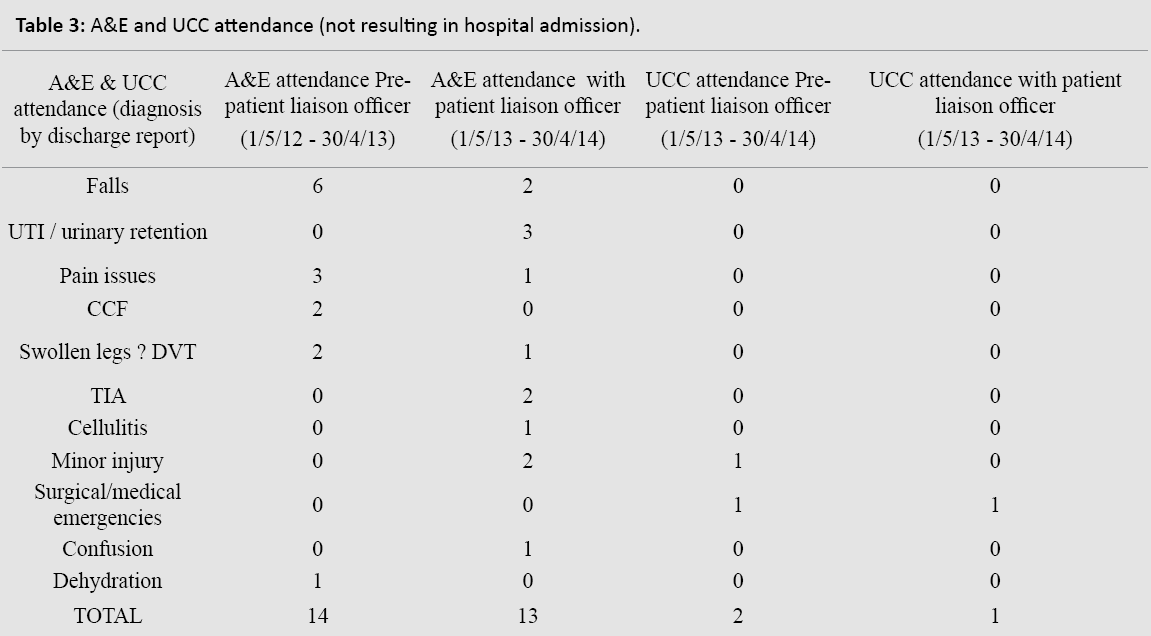
In the year prior to introduction of the patient liaison officer, there were 32 unplanned hospital admissions and 16 additional hospital A+E and UCC attendances. In the year after, there were 16 unplanned hospital admissions and 14 additional A&E / UCC attendances (Tables 2 and 3). Number of admissions for any individual in any one year ranged from 0 - 3. This represented a 50% reduction in unplanned hospital admissions after introduction of the patient liaison officer, particularly relating to falls; chest pains; urinary tract infections and urinary retention. Attendances at A&E or UCCs not requiring admission remained unchanged.
Independently, through active case finding, the number of registered housebound patients at the practice rose from the initial 78 to 139 by the end of the 2 year period. During this 2 years, 37 patients had died (including 14 from the study cohort), with 19 dying prior to introduction of the patient liaison officer and 18 with the patient liaison officer in post. Overall, practice mortality rates amongst housebound patients remained static during the study period, and there was no indication that reduced admission rates in the study group influenced mortality.
Throughout the study, GPs continued regular reviews, the frequency being determined by patients and their GP, ranging from monthly to 4 monthly. For patients requiring home visits (55), an average of 8 visits were made per year per patient, and for those brought to the practice (9), an average of 7 contacts were recorded per year. This did not change over the 2 year study although individual consultation rates varied by up to 50%. The GP, patient and carer(s) remained responsible for generating the care plan, using the same format throughout the study.
From the pilot patient satisfaction survey of 30 patients, 18 responses were received, 5 being completed by carers. 12 (66%) commented on easier access to services through the patient liaison officer, with carers particularly valuing information given about other services and attention to their needs as carers. 5 specifically felt better supported and 3 asked if the patient liaison officer might visit them at home. 2 remained unsure about the role but welcomed the prospect of more support.
This study suggests that a new administrative role, with protected time to support housebound patients can reduce unplanned hospital admissions, and support the out-of-hospital and adult safeguarding agenda. Implementation of care plan action points and better access for patients and carers may have led to a reduction in avoidable admission, particularly for falls and common infections. Although this is a small study, other studies looking at interventions of case managers and care navigators in other care settings with different groups of vulnerable patients (cancer and nursing home patients), have shown similar reductions in unplanned hospital admissions [9,10], through support and guidance through complex health and welfare systems. Increased contact between the practice; patients; carers and external providers enabled greater sharing of information; earlier detection of problems and greater patient involvement in care. Patients and carers felt better supported, and although this requires further evaluation, this finding is mirrored in other studies where care navigation and case management are valued by patients with complex care needs [21].
Attempts were made to minimise variability over time and address confounding factors to measure impact of the patient liaison officer in addition to the care plan or GP input. A time period of one year was used before and after introduction of the patient liaison officer to allow for seasonal influence on hospital and UCC attendance.
Housebound patients are a dynamic group, with increasing age and frailty tending to increase health and social problems over time. Active case finding was underway at the practice, aiming to identify emerging vulnerable patients (including the housebound) at risk of unplanned hospital admission and loss of independent living. There were also deaths amongst this group during the study. With active case finding and deaths, patients were entering and leaving the housebound group throughout the two years. The UK Evercare study recognised that such issues may have led to a failure to demonstrate influence on hospital admission rates despite perceived reductions by clinicians [22].Therefore, in order to maintain integrity of comparison of information before and after introducing a patient liaison officer, only the 64 patients identified at the outset, meeting the entry criteria, were included in this study. Inclusion of only those who survived the 2 year period allowed those patients to act as their own control. This was advantageous to the study given the clinical heterogeneity of the cohort. However, patient liaison officer input required for those who died and were consequently excluded, could therefore not be analysed.
Recruiting patients who had care plans developed routinely and in place for the year before introducing the patient liaison officer meant the cohort was not identified through recent crisis, which could have triggered increased hospital attendance and reflected in higher admission rates in the first year with regression to the mean thereafter [23]. Patients were not classified beyond being housebound, enabling the study to focus on the types of problems for which a liaison role might influence unplanned admissions, rather than sub-populations. It may be that accelerated and thorough implementation of care plan action points in different sub-populations could impact on other factors leading to hospital admission. However, this requires further study in larger populations. Increasing age and frailty in the cohort could not be controlled for but this may have been expected to result in an increased admission rate rather than reduction.
Problems for which admissions were reduced were consistent with the impact of the patient liaison officer offering personal support and implementing care plan action points. Within the 7 hours per week (of which approximately half was used for the study cohort), the patient liaison officer followed up referrals for social care; physiotherapy and occupational health support and home adaptations; coordinated services and established communication channels through the practice. This may have reduced risk of falls. A designated e-mail address allowed patients; carers and external care agencies to communicate more effectively. It allowed easier monitoring of medicines usage and developed closer links with local pharmacists, who often delivered medicines to these patients. The patient liaison officer offered additional access for patients and carers to report signs of early deterioration, particularly in cases of urinary tract infection, where early assessment and treatment could contribute to reduced hospital admission.
Number of attendances at A&E and UCCs, separate from admissions, were low, and showed little change during the study, although attendance for falls was reduced. That attendances did not increase, suggests that those who were previously being admitted were no longer needing to attend, rather than any change in management at urgent care services. Not all attendance may be preventable but further study is needed to see if patterns of patient behaviour might change over time, or outcome be influenced with a larger cohort.
The patient liaison officer role is both feasible and desirable given increasing automation of traditional receptionist roles; the need to retain staff who have significant local knowledge and relationships with patients, and economic drivers to reduce avoidable use of secondary care services. An ageing population is already impacting on the increasing workload for GPs, and whilst this study does not attempt to measure reduced administrative time spent on housebound patient care by GPs, it is possible that time invested by GPs to review care plans and progress with patient liaison officers would be offset by reduced administrative workload and ultimate reduction in clinically driven home visits. We believe this is an important area of workforce development that needs further exploration through larger studies, to refine the training; embed the role and measure impact on a broad range of health outcomes.
- A larger study is required to confirm the impact on unplanned admissions and further investigate attendances at A&E and UCCs.
- Satisfaction surveys, to qualitatively analyse impact of a patient liaison officer from the patient’s; carers’; GP’s, and provider organisations’ perspective to identify future potential and training needs, to enable refining and extension of the current training programme.
- A cost analysis of benefits to the health economy would help to support wider investment in this role.
The patient liaison officer: a new role in UK General Practice, describing the training programme, previously published in Quality in Primary Care in 2013.19
Ethics committee approval was not sought as this was a service design initiative rather than a research project
We would like to thank the Ballater Surgery practice team and patient cohort for their commitment and enthusiasm to implement this new role, and Bromley Clinical Commissioning Group for their support for the earlier training programme for patient liaison officers in general practice.