What is known on this subject
• Women of South Asian origin struggle to gain access to appropriate advice on their genetic susceptibility
to cancer.
• Culturally insensitive service provision, in addition to the broader processes associated with institutional
racism, is responsible for such shortfalls. However, practitioners experience difficulties in overcoming
these shortfalls.
• There does appear to be interest in such advice among women, especially in the case of breast cancer, but
little is known about how best to offer support in a way that is acceptable to women.
What this paper adds
• Our findings demonstrate how services can offer care that is sensitive to the needs of women of South
Asian origin in a way that facilitates choice.
The cultural resources available to South Asian respondents when making sense of cancer genetics,
although similar to those for the majority of the white community, did demonstrate some differences.
Women of South Asian origin, for example, are more likely to associate cancer with death, and are generally
less knowledgeable about the origins of, causes of and outcomes associated with a diagnosis of cancer.
• Access to cancer genetics services remains a problem, despite its general appropriateness, from the
woman’s point of view. Women either had not heard of the service or else had not been referred to the
service by their general practitioner.
Key words
cancer genetics, ethnicity, service delivery,
social exclusion
Introduction
The UK, like other advanced industrial countries, struggles
to provide accessible and appropriate healthcare
to culturally diverse populations (Bhopal, 2007). Despite
an apparent willingness on the part of the health
agencies to challenge discriminatory practices, problems
remain (Ratcliffe, 2004). This paper explores
possible ways of engaging with these difficulties, by
discussing the policy and practice relevance of a research
project designed to evaluate a cancer genetics service
whose purpose was to make up for shortfalls in previous
provision. This empirical case study is used to
introduce a broader theoretical discussion about how
healthcare can respond successfully to the needs of
an ethnically diverse population. One key aim of the
paper, rather than offering a service evaluation per se,
is to reconcile what can be extremely abstract debates
within the specific dynamics of service delivery. We
are aware of how accounts of social inequalities can
seem complex and sometimes overwhelm more practically
orientated debates about how best to organise
and deliver service support. At the same time, by
ignoring the complexity of such debates, mainstream
provision can fall into the trap of ‘reinventing the
wheel’ and not learning from previous insights (Ahmad
and Bradby, 2007).
The context of service delivery
Healthcare provision for ethnically diverse populations
occurs against a backdrop of socio-economic
disadvantage, institutional racism and social exclusion
(Parekh, 2006). Despite increasing awareness of the
complex nature of culturally sensitive provision, various
discriminatory practices, which are revealed in professional
assumptions and organisational practices, either
ignore or misrepresent the needs of ethnically diverse
populations (Karlsen, 2007). Practitioners, for example,
still lack confidence when discussing cultural competent
practice (Peckover and Chidlaw, 2007), often reverting
to simplified generalisations, which they believe
enable them to ‘manage’ ethnic diversity (Atkin and
Chattoo, 2007). The pilot service was introduced in
response to these concerns. Cancer patients, irrespective
of ethnicity, want more information about their
condition and its consequences than they generally
receive (McPherson et al, 2001). South Asian populations
and patients from underprivileged backgrounds
appear to be particularly disadvantaged and receive
poor cancer care compared with the majority population
(Velikova et al, 2004). Cultural insensitivity on the part of service organisations emerged as particularly
relevant, for example, when making sense of the
experience of breast cancer (Randhawa and Owens,
2004). However, culturally competent care can be difficult
to realise in practice. Accessibility, for example, is
becoming increasingly confused with appropriateness,
and difference is sometimes emphasised at the expense
of potential similarities between different ethnic groups.
Current policy and practice can therefore appear to
lack an informed and pro-active strategy, and this
reflects the broader tensions of providing care within
multi-cultural settings.
The number of referrals of people with a family
history of cancer to the Regional Genetic Service,
where the pilot was introduced, increased from 800
in 1998 to over 2500 in 2006. A growing awareness of
the relationship between cancer and genetics helps to
account for this increase. However, when these referrals
were examined, a bias was found towards individuals
from higher socio-economic classes and from the
majority ethnic population. In the localities served
by the pilot, 5% of referrals were for people of South
Asian origin, even though the population classified as
‘South Asian’ represented 30% of the total population.
This could not necessarily be attributed to the younger
age profile of the South Asian population or, more
generally, to a lack of interest. A previous study demonstrated
how women of South Asian origin with breast
cancer worried about other family members, and
especially their children, developing the condition
(Karbani, 2002).
A pilot service, funded by Macmillan Cancer Relief
and the Department of Health, was developed to offer
non-directive, trans-cultural genetic counselling as a
means of facilitating informed choice among previously
marginalised populations, through a discussion of risk,
screening, testing and risk-reducing strategies in a primary
care setting. This service, one of eight pilot services
based in primary and secondary care, was part of a
broader commitment on the part of policy makers to
explore the concerns of people with a family history of
cancer, and to provide them with information and
support, as away of developing provision for thosewhose
cancer might have a genetic cause (www. macmillan.
org.uk/About_Us/Specialist_healthcare/Cancer_genetics_
programme/Cancer_genetics_programme.aspx).
Details of the pilot service can be found elsewhere
(Srinivasa et al, 2007), and are not the focus of this
paper, except in its broadest sense. Of interest to us,
however, are the barriers to accessing the service for
South Asian communities, and the appropriateness
of provision from the perspective of the potential and
actual service user, which is used to explore how
ethnicity mediates the process of service delivery.
Conducting the research
A qualitative methodology is particularly effective for
obtaining an understanding of how people interpreted
what was happening to them, within the context of
their social relationships (Silverman, 2001). However,
it requires a particular form of justification. Our
immediate problem in defining a sample was how to
capture the experience of a diverse community, of
various faiths, cultures, languages and dialects, which
has become ‘labelled’ in the policy literature as ‘South
Asian.’ The practical responses which inform this
study tend to classify people according to their ethnic
origin and religious identity. There is some theoretical
justification for this, as for people of South Asian
origin, ethnicity and religious identity often reinforce
each other (Modood et al, 1997). Beyond this, our
sample largely reflected the demographic profile of the
locality covered by the pilot, in which Pakistani-
Muslims are numerically the largest ethnic-minority
group.
Another important consideration, when sampling,
is to avoid producing findings that essentialise ethnic
differences. When evaluating the pilot, we wished to
identify similarities and differences in experience among
various ethnic groups, including the majority white
population. We therefore included a sample of people
from the white community. We accept the problems
of defining ‘white’ in this context, but simply wished
to include a sample that would enable us to contextualise
the views of our South Asian sample, and in
particular to ensure that any differences identified
between our samples could be reasonably explained in
relation to a person’s ethnic origin, while also offering
an understanding of the more generic experience of
those at risk of developing cancer. We also have to
acknowledge that our sample is predominantly female. Finally, we needed to ensure that the comments of
those who used the service reflected tangible benefits
from the pilot project, rather than benefits that could
be gained by more generic (non-genetic) provision.
Our sample therefore includes the views of those with
a family history of cancer, who had not accessed the
pilot cancer service, in addition to the views of a sample
of people who had experience of the pilot cancer
genetics service.
We gained formal approval from an NHS local
ethics committee for our research, which meant that
we followed agreed principles of informed consent
and anonymity.
Potential respondents were contacted and interviews
were arranged. Those who were using the pilot
service were identified from practitioners’ records.
Those who were not using the service but potentially
had a family history of cancer were identified fromtwo
support groups for women with breast cancer, one
largely consisting of South Asian women and the other
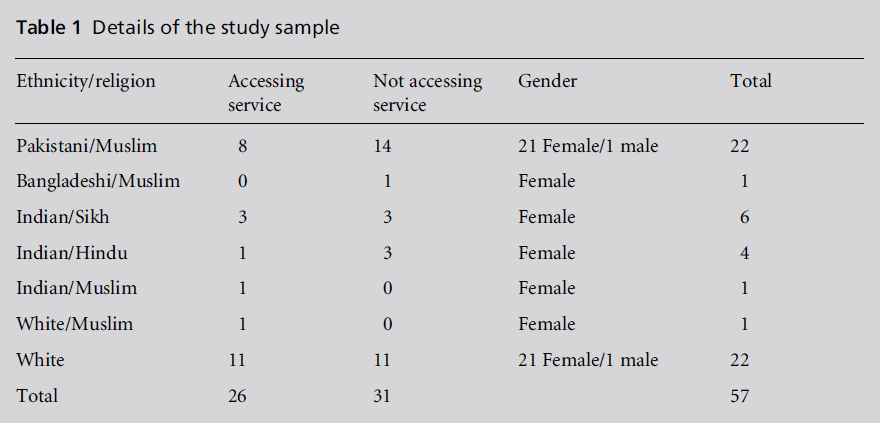
consisting of white women. Table 1 outlines the details
of the sample. Of those who were contacted, no one
refused to be interviewed.
All of those who were interviewed had a diagnosis
of cancer, and specifically a diagnosis of breast cancer
(n = 52). Of the five respondents who did not have
breast cancer, two had not accessed the pilot service,
and had what they described as ‘blood’ cancer. Of
those who had accessed the pilot service, one woman
had bowel cancer, of which there was a family history,
and two men had Hodgkin’s lymphoma.
All of the potential interviewees had access to an
information sheet, which was available in English, Urdu,
Hindi, Gujarati and Punjabi. In-depth interviews,
informed by a topic guide, explored the participants’
biographical details as a way of building rapport and
contextualising subsequent discussion, perceptions of
cancer and cancer genetics, access to services, and positive and negative experiences of service delivery.
Respondents were able to choose the language in which
they were interviewed, and we conducted 11 interviews
in languages other than English. These interviews
were back-translated, on the basis of conceptual
rather than literal meaning. In undertaking the research,
we were aware of other ethical issues raised by
our work. All of the respondents were aware of their
risk of cancer before they were approached by amember
of the research team. However, they might still be
uneasy and perhaps unclear about this risk. We had
the option, after seeking the respondent’s permission,
of arranging an appointment with a genetic counsellor.
Each interview was audio-taped, transcribed and
organised into themes. All of the participants’ names
that appear hereafter have been changed in order to
maintain anonymity.
Table 1: Details of the study sample
Our approach to analysiswas iterative, and it explored
concepts, established links between them, and offered
explanations for patterns or ranges of responses or
observations from different sources (Silverman, 2001).
We began by identifying themes relevant to an interview,
which were then interrogated in relation to each
individual account (as a means of understanding a
particular case), compared across cases by highlighting
potential similarities and differences, and finally
related to respondent characteristics that could be
reasonably justified as an explanation which mediated
experience. Our aim was to move beyond a semantic
and descriptive account of specific interviews towards
a level of analysis in which themes were explicated
within existing and emerging theory and debate
(Riessman, 2002).
Providing a cancer genetics
service
Inevitably, the respondents’ accounts blend both perceptions
of cancer and the cancer journey. However,
given the aims of the paper, in which our findings are
contextualised within broader debates on provision
of healthcare for multi-cultural societies, we did not
regard this as a problem.
For those participants who did not access the pilot
service, poor communication emerged as an important
barrier. Participants’ narratives, irrespective of ethnicity,
suggest that mainstream (non-genetic) practitioners
were not providing easily understood medical information
in a way that elicited the patient’s collaboration
in developing a future strategy of care. Many
respondents reflected on how the initial consultation
was professional-centred, and was aimed at collecting
information, rather than providing an explanation of
why such information might be useful. This is often a feature of both primary and secondary care consultations
(Robinson, 2001), especially when dealing with
more discursive issues, such as screening and risk
(Baile et al, 2000). These difficulties affect both those
who speak English as a first language and those who do
not, which highlights the fact that providing consultations
in a person’s first language does not obviate the
need to address broader communication issues.
However, communication difficulties were compounded
for those who did not speak English as their
first language. The problems of language support have
been a constant feature of the literature for at least
20 years (Ahmad and Bradby, 2007). For our respondents,
the use of interpreters simply enforced the
professional-centred nature of the consultation, and
some respondents felt that the interpreters struggled
to translate what is often extremely complex information.
This introduced uncertainty, which was made
worse for those who believed that the interpreters were
implicitly making decisions on their behalf and exercising
discretion about what information was passed
on. Despite this, people who had access to an interpreter
expressed more satisfaction with the consultation
process than those who had to rely on friends or
family members to interpret for them. Gaining access
to an interpreter was far from straightforward, and
many people felt under pressure to make their own
arrangements. In the following extract, Aisha illustrated
how such ad hoc strategies raise issues of
confidentiality:
‘I think she [nurse] said ‘‘have you got anyone you can
bring with you?’’ I didn’t know who to take. I didn’t want
anyone to know what was happening to me. I have small
children. In the end I took my friend’s daughter. They
should have given me someone.’
Many respondents felt that they had to balance the
need to understand what was happening to them with
the need to compromise their desire for confidentiality.
Using family members as interpreters could
also cause other tensions. Shamim described how her
daughter struggled emotionally to translate information
that could potentially affect her own well-being
(Gaff et al, 2007).
Following the initial consultation, irrespective of
whether the women had access to the pilot service or
not, those with or at risk of breast cancer felt uncomfortable
discussing their cancer and family history
with male acquaintances, which raises yet another
generic issue when making sense of communication
and family genetics (Forrest et al, 2003; Shaw, 2009).
Discussions, especially in the case of breast cancer, were
seen to conflict with cultural norms in which women
are expected to maintain modesty when speaking to
men other than their husbands, although this viewwas
not exclusive to Muslim participants. Many women
talked about ‘reserve.’ Heema, an Indian-Hindu, remarked that ‘It is hard telling anyone because you
can’t really talk about the illness. It’s a bit like feeling
shame because it is in a private part.’ Annabel, a white
woman, similarly commented: ‘I mean having to talk
about it just makes me embarrassed.’
By employing workers who were multi-lingual and
culturally sensitive, the pilot service avoided some of
these difficulties. South Asian women were able to
discuss their situation with a skilled and knowledgeable
worker who often shared their linguistic background.
Overcoming language barriers was not the
only advantage of employing such workers. Women
who were fluent in English commented on the value of
having contact with a worker who had cultural insight
into the issues that they faced in their daily lives. Several
women, for example, expressed confidence that these
practitioners understood such issues as the working of
broader family relationships, as well as some of the
religious sensitivities associated with communicating
bad news, while having a more general respect for the
important role played by their faith in making sense of
health and illness. These women felt that they did not
have to justify their cultural difference in a way that is
often necessary in consultations with more mainstream
practitioners. They also felt that they could
speak more freely about their lives, without the risk of
being judged. The pilot service also wished to explicitly
avoid the professional-centred model of care by focusing
on the needs of the women. The experiences of
those who had accessed the service, irrespective of
ethnic origin, suggest that this objective was achieved.
Consequently, the women not only understood more
about the genetic risks of cancer, but were also more
confident about discussing these risks with other
family members. However, those who used the pilot
service did not always comprehend the problems of
confidentiality that a practitioner might face when
disseminating information within families, and interpreted
the caution of practitioners as frustrating rather
than helpful.
Cancer as metaphor
Capturing the meaning of cancer throughmetaphor is
an important feature of the literature (Sontag, 1978),
and reminds us that service practitioners need to
engage with lay perceptions which might seem to be
at odds with their own constructions about the origins
of cancer (Schou and Hewison, 1999). Discussing how
people make sense of cancer is especially valuable in
developing service support, particularly as it ensures
that practitioners can be sensitive to an individual’s
language and ways of understanding (Dein, 2004).
How people create their own understanding of cancer
is related to their use of language. This not only enables them to understand what is happening to
them, but also allows them to express this understanding
to others. However, as Sontag observed, this
language can create its own mythology, distorting the
‘truth’ about illness and isolating the patient from
broader cultural understandings which might empower
them. This is the practical context in which
practitioners have to work, and one that we shall now
explore.
White participants were generally better informed
about cancer outcomes. Our South Asian sample,
however, felt that unless cancer was detected and
treated in its early stages, it was an incurable disease
(Randhawa andOwens, 2004).Nira, aPakistani Muslim,
expressed the views of many when she said ‘That’s it.
It’s the beginning of the end.’ South Asian respondents
were more likely to associate negative taboos with
what they regularly called the ‘C-word.’ This raises
potential barriers when disseminating information
about cancer genetics among extended families, particularly
when the person has been diagnosed as
having cancer. Iqra, a Pakistani-Muslim, commented
on how she could not tell her family that she had
cancer because they would associate her diagnosis with
‘certain death.’ Achal, an Indian-Hindu, commented
that she would not discuss her cancer with anyone
because of the stigma associated with the disease.
However, it is difficult to know whether such assumptions
reflect ethnic or social class differences, particularly
since those from a working-class background
express similarly negative views about the outcomes of
cancer (Selby, 1996).
Nonetheless, many of the participants, irrespective
of ethnic origin, felt that cancer, although a consequence
of lifestyle, was something that ‘just happened’
and was a matter of ‘being unlucky’, which suggests
that fatalism is not solely the preserve of ethnicminority
populations. Furthermore, when the respondents
reflected on the possible causes of cancer, they
specifically discussed how the available public discourses
appeared to be contradictory, and that it was
difficult to make sense of them. This is why the
respondents had a natural scepticism about attributing
any cause to cancer. It was especially rare, irrespective
of their ethnic background, for them to associate
cancer with a genetic cause. The few who did so had
accessed the pilot cancer genetics service, but even
then therewas some doubt. For example,Amyremarked
that ‘You can never be 100% certain it is that. So I don’t
know.’ The idea that cancer might run in families
particularly troubled several respondents, as it seemed
to give cancer a kind of inevitability.
However, the participants were not entirely responsible
for their misconceptions. Zareena, like several
other women of South Asian origin, remarked that
until she was diagnosed with cancer she had believed
that cancer only occurred in white women: ‘When I went to the doctor’s he reassured me, saying that Asian
ladies don’t usually get cancer, or there’s not much.’
Such misinformation was not confined to women
of South Asian origin. Tina’s mother died of breast
cancer at only 40 years of age, and one of her aunts had
also had breast cancer. Yet still her GP did not take her
concerns seriously: ‘I went to my GP then, that’s when
I said look, it’s in my family, but I always got told it
skipped a generation, and that’s what you get told
every time.’
Ranjit, an Indian Sikh, explained how a wellmeaning
breast cancer nurse deterred her from further
investigation:
‘Yes but they say it is not true. I said to them check my
daughter, they said you should not think like this, just
because you have it does not mean that your daughter can
have it ... I was worried if I had it, I did not want my
children to have it and I wanted them checked.’
The role of a cancer genetics
service
As we have seen, the respondents who accessed the
cancer genetics service had some understanding about
the potential link between cancer and genetics and the
potential risk of cancer for their family. Being better
informed about cancer was not only important for the
individual, but also enhanced their ability to negotiate
with other family members, who might have a predisposition
to develop cancer. People did not want to
introduce the idea that other family members might
be at risk of cancer, if they could offer no hope. By
challenging long-standing assumptions about cancer,
the pilot service was available to encourage more
informed choice among those at risk.
However, the interviewees expressed disappointment
about the vagueness of the information that they
received from the pilot service. To this extent, negotiating
expectations emerged as an important aspect of
the communication process, particularly when interventions
seemed to be counter-intuitive, challenging
the respondents’ definitions of the nature of medicine,
as well as what constitutes family. The respondents
expected certainty, which the pilot service could not
give them. They wanted to be told whether or not they
and their family were at risk, rather than being given
an odds ratio, which they found difficult to interpret.
However, this perhaps reflects a more generic tension
facing modern medicine, with its increasing emphasis
on preventive interventions and informed choice, and
has little to do with ethnicity or cancer genetics (Bryant
et al, 2005; Calnan et al, 2006).
As further demonstration of their unrealised expectations,
the respondents were under the impression that their genetic risk could be determined by a simple
blood test. Zareena, a Pakistani Muslim, explained:
‘Our GP referred us to the service, saying that they would
test us for genetics ... but when we got there we had a
discussion and she asked us our family history and things.
... It was more of a counselling session ... she said that it
wasn’t genetic ... but I really thought that I would have a
test and definitely know that it wasn’t. I was just a bit
surprised that just from the history they can determine
that ... I don’t know it felt like something was missing
because they didn’t do anything.’
Nor were these responses exclusive to women of South
Asian origin. For example, Anne, a white woman,
commented that ‘I don’t see how they can know all
that from just talking to you.’ These responses reflected a
more general confidence in Western medicine and its
power to identify and diagnose conditions through
scientifically based clinical interventions, while also
introducing a sense of uncertainty about the value of
taking family histories when assessing a person’s risk
of cancer. The emphasis on taking a family history
particularly confused some people, as it seemed alien
to their ideas of scientific medicine. How could diagnosis
of such a serious condition depend on the
narrative accounts of family members?
The respondents also struggled with the idea that
their wider extended family might be at risk of cancer
in the same way as their more immediate family,
although definitions of who belonged to ‘immediate’
family depended on a person’s own sense of family
relationships, based on normative assumptions about
obligations, rather than ‘biological’ definitions. For
some, immediate family included aunts and uncles,
whereas for others it only extended as far as grandparents.
This finding occurred irrespective of ethnicity,
and it demonstrates some of the difficulties involved
when taking family histories, as definitions of who is
family and therefore at risk vary from one individual
to another. (For a more general discussion of the
implications of this for communicating genetic information,
see Armstrong et al, 1998 and Shaw, 2009.)
Accessing a cancer genetics
service
The appropriateness of the pilot service did not appear
to be a problem. However, access was an issue, especially
among South Asian respondents, as many who
had not been referred to the pilot service were unaware
of its existence. Kurshid, a Pakistani Muslim, whose
breast cancer was known to have a genetic cause,
remarked that ‘It is a great thing if I knew about it,
but no one has said anything to me.’ Once people did
find out about the existence of the service, they expressed disappointment that the practitioner
involved in their care had not told them about it.
Tina, for example, felt that her GP should have
informed her about the service, particularly since
there was a history of breast cancer in her family (see
above). Fiza, a Pakistani Muslim, and Palvi, an Indian
Hindu, both expressed similar concerns. Those who
had accessed the pilot service felt that their referral had
taken place by chance.
Discussion
Our case study demonstrates how services can offer
care that is sensitive to the needs of culturally diverse
populations. Those who accessed the pilot service,
irrespective of ethnic origin, valued the opportunity
to discuss their situations in a way that was relevant
to their experiences. This is perhaps not surprising,
given that the broader literature indicates that people,
irrespective of ethnic origin, value one-to-one, unhurried
communication with an informed practitioner
(Armstrong et al, 1998). Nonetheless, the pilot service
not only facilitated a greater sense of informed decision
making among respondents, but also led to
greater confidence when negotiating with other family
members.
Individuals whose families were at high risk of
developing cancer also commented on how the service
supported them in making decisions about preventive
measures, such as mastectomy, which were rarely taken
up, and making them more aware of the need for
regular health checks. People with families at low risk
spoke of how contact with the service helped to
alleviate some of the anxiety associated with inherited
disease. The South Asian respondents specifically
praised the cultural and religious sensitivity, friendliness
and flexibility of service provision. Respondents
were also turning to genetic counsellors for explanations
about treatment options and signposting to
other cancer services. This was an unintended consequence
of the pilot project, which perhaps highlights
some shortfalls in good practice on the part of GPs,
cancer consultants and nurses.
However, problems remained and, by exploring
these, our findings can contribute to current debates
about genetic counselling within families, by exploring
similarities and differences among diverse ethnic
groups. For example, the participants remained uncertain
about the link between cancer and genetics,
reflecting generic lay understandings about the potential
causes of cancer, irrespective of ethnic origin (Gaff
et al, 2007). The pilot service struggled to engage
successfully with these lay understandings, particularly
when information seemed to conflict with the respondents’
experience. For example, many of the respondents thought that the taking of family trees was a
rather ‘quaint’ practice, with little relevance to diagnosing
cancer. Expectations of the pilot service also
exceeded what it could deliver. Respondents expected
to be provided with specific information about their
risk, and also did not understand practitioners’ sensitivities
about potential breaches of confidentiality.
The cultural resources available to South Asian
respondents when making sense of cancer genetics,
although similar to the majority white community, did
demonstrate some differences. People of South Asian
origin were more likely to associate cancer with stigma
and death, which sometimes made them reluctant to
raise the issue with other family members. Such views
are not entirely absent from the accounts of people
from the majority ethnic population, but are less common.
More generally, people of South Asian origin
were less knowledgeable about cancer than the majority
white population, and were certainly less aware of the
support available, although in some cases this situation
was exacerbated by unhelpful contacts with
healthcare professionals. However, social class differences
could be as important as ethnicity in explaining
this.
Recognising the distinctive quality of these cultural
resources is a complex but important task for practitioners,
particularly since some of the issues raised
in our discussion reflect the more general process
of social exclusion. Ethnicity is not always a marker
of disadvantage, and although the experience of our
respondents demonstrates some differences, it also
illustrates similarities to the experience of the general
population. Successful healthcare that caters for a
diverse population must employ professionals who
are culturally literate and able to recognise the impact
of cultural resources without falling into the trap of
stereotyping their patients. In particular, they need to
understand when ethnicity makes a difference and
when it does not (Chattoo and Ahmad, 2008).
The pilot service offered ways of practically engaging
with difference in a way that is appropriate to a
linguistically and culturally diverse population, particularly
in working with individuals’ own definitions
of what is happening to them, rather than by imposing
the practitioner’s views, sanctioned through professional
practice (Dominelli, 2004). However, such reflexivity
is not simply about individual reflection on practice,
but also requires an engagement with the ways in
which institutional practices can sometimes make it
difficult for a practitioner to realise reflexive insights.
Practitioners associated with the pilot service worked
within culturally sensitive organisations, which helped
to support and sustain their work (Srinivasa et al,
2007). This should not be underestimated, particularly
in view of the fact that a common frustration
expressed by practitioners concerns the conflict between
their own willingness to offer sensitive care and their organisation’s ability, or inability, to support
them (Atkin and Chattoo, 2007).
Further tensions have emerged, relating to the
difficulties of offering screening in a way that facilitates
choice, while not causing unnecessary anxiety
(Scott et al, 2005). The question arises as to whether
information is always a good thing, particularly when
there is no treatment for some forms of cancer. Our
respondents also expressed concerns about raising the
issue of cancer within their families, particularly
because they did not want to be responsible for giving
other family members potentially distressing information
about their relatives (Walter et al, 2004;
Featherstone et al, 2006; Shaw, 2009). Weighing up
the advantages and drawbacks of disclosure, particularly
when the person to whom information is disclosed
might have cancer, or associate it with certain death, is
far from straightforward (Cox and McKellin, 1999;
Hallowell, 1999).
Such tensions again occur irrespective of ethnic
origin, although they probably have a greater impact
among social excluded populations. Survival rates for
most cancers tend to be worse among ethnic-minority
populations. Many of the difficulties are attributed
to delays in diagnosis. A more pro-active screening
programme might therefore be of benefit, but since
the ability of secondary and tertiary services to respond
to cultural diversity is in doubt, it is questionable
whether this is a viable option. Access without
appropriateness is therefore a problem(Sedgwick et al,
2003; Fischbacher et al, 2009).
In the case of the pilot, the opposite problem
occurred, as appropriateness of delivery did not necessarily
improve access. This is manifested in two ways,
and although it was not exclusive to South Asian
respondents, the impact seemed more likely to deny
them access to support. First, those who were potential
clients of the genetics service, either directly as patients
or indirectly as family members, did not know that the
service existed, so could not initiate referral. Secondly,
there is an overall lack of knowledge among the general
population about the relationship between genetics
and cancer (Walter et al, 2004; Donelle et al, 2005).
The problems associated with access raise further
and more fundamental issues about how we come to
understand equality. The inverse care law appears to
be especially relevant when making sense of this
(Tudor Hart, 1971). The publicity surrounding the
pilot programme did lead to a rise in the number of
referrals, and specifically improved the referral rates
for people from lower socio-economic groups and
from a South Asian background. However, these referrals
were disproportionate to the rise in the number of
referrals from the white majority community, from
higher socio-economic groups (Srinivasa et al, 2007).
This is probably a generic problem facing those
responsible for developing health services, as it is difficult not to perpetuate existing disadvantage, particularly
since the middle classes have greater cultural
and social resources to take advantage of new forms of
service support. However, the role of service practitioners
is equally significant in creating the potential
for disadvantage. For example, referral to the pilot
service tended to be ad hoc and dependent on proactive
patients, who are more likely to be from the
middle classes, rather than on pro-active healthcare
professionals. Ironically, when healthcare professionals
were pro-active, they were more likely to be so on
behalf of middle-class people from the majority white
population.
Our account of access demonstrates, more generally,
how the pilot service existed within the context
of a healthcare system that struggles with diversity.
Healthcare professionals, especially those working in
primary care, have an important role in facilitating
improved access to service support, by helping people
to understand the potential relevance of the service to
their lives. This is why focusing on the dynamics of
service delivery is as important as exploring the experiences
of those who receive health and social care. This
requires theoretical reconciliation and practical intent,
especially since there is a long-standing and ongoing
disparity between our understanding of the issues and
our commitment to act (Taylor, 1994). By reconciling
this disparity, we can provide the foundations for
more successful interventions, in which the emerging
evidence can engage with and develop existing examples
of innovative practice.
ACKNOWLEDGEMENTS
We would like to thank the individuals who agreed to
be interviewed for this study, and the support groups
and healthcare professionals who helped us to gain
access to them. Last but not least, we would like to
thank Macmillan Cancer Relief and the Department of
Health for funding this research. The study received
UK ethical approval.
CONFLICTS OF INTEREST
None.
References
- Ahmad WIU and Bradby H (2007) Locating ethnicity and health: exploring concepts and contexts. Sociology of Health and Illness 29:793ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â811.
- Armstrong D, Michie S and Marteau T (1998) Revealed identity: a study of the process of genetic counselling. Social Science and Medicine 47:1653ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â8.
- Atkin K and Chattoo S (2007) The dilemmas of providing welfare in an ethnically diverse state: seeking reconciliation in the role of a ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âreflexive practitioner.ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Policy and Politics 35:379ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â95.
- Baile WF, Buckman R, Lenzi R et al (2000) SPIKESÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬ÃÂa sixstep protocol for delivering bad news: application to the patient with cancer. Oncologist 5:302ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â11.
- Bhopal R (2007) Ethnicity, Race and Health in Multi- Cultural Societies. Oxford: Oxford University Press.
- Bryant LD, Green J and Hewison J (2005) Attitudes towards prenatal diagnosis and termination in women who have a sibling with DownÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s syndrome. Journal of Reproductive and Infant Psychology 23:181ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Calnan M, Wainwright D, Clasner P et al (2006) MedicineÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s next goldmine? The implications of the new genetic health technologies for the health service. Medicine, Health Care and Philosophy 9:33ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â41.
- Chattoo S and Ahmad WIU (2008) The moral economy of selfhood and caring: negotiating boundaries of personal care as embodied moral practice. Sociology of Health and Illness 30:550ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â64.
- Cox S and McKellin W (1999) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âThereÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s this thing in our familyÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: predictive testing and the construction of risk for Huntington disease. Sociology of Health and Illness 21:622ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â46.
- Dein S (2004) Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncology 5:119ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â24.
- Dominelli L (2004) Social Work: theory and practice for a changing profession. Cambridge: Polity Press.
- Donelle L, Hoffman-Goetz L and Clarke JN (2005) Ethnicity, genetics and breast cancer: media portrayal of disease identities. Ethnicity and Health 10:185ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â98.
- Featherstone K, Atkinson P, Bharadwaj A et al (2006) Risky Relations: family, kinship and the new genetics. Oxford: Berg Publishers.
- Fischbacher CM, Bhopal R, Steiner M, Morris AD and Chalmers J (2009) Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. Journal of Public Health Medicine, Advance Access, published 5 February 2009.
- Forrest K, Simpson S, Wilson B et al (2003) To tell or not to tell: barriers and facilitators in family communication about genetic risk. Clinical Genetics 64:317ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â26.
- Gaff C, Clarke A, Atkinson P et al (2007) Process and outcome in communication of genetic information within families: a systematic review. European Journal of Human Genetics 15:999ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â1011.
- Hallowell N (1999) Doing the right thing: genetic risk and responsibility. Sociology of Health and Illness 21:597ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â621.
- Karbani GA (2002) Transcultural genetic counselling in the UK. Community Genetics 5:205ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Karlsen S (2007) Ethnic Inequalities in Health: the impact of racism. London: Race Equality Foundation.
- McPherson C, Higginson IJ and Hearn J (2001) Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. Journal of Public Health 23:227ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â34.
- Modood T, Betthould R, Lakey J et al (1997) Ethnic Minorities in Britain. London: Policy Studies Institute.
- Parekh B (2006) Rethinking Multiculturalism: cultural diversity and political theory. Basingstoke: Palgrave Macmillan.
- Peckover S and Chidlaw G (2007) The (un)certainties of district nurses in the context of cultural diversity. Journal of Advanced Nursing 58:377ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â85.
- Randhawa G and Owens A (2004) The meanings of cancer and perceptions of cancer services among South Asians in Luton, UK. British Journal of Cancer 91:62ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â8.
- Ratcliffe P (2004) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âRaceÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢, Ethnicity and Difference: imagining the inclusive society. Maidenhead: Open University Press.
- Riessman CK (2002) Narrative analysis. In: Huberman AM and Miles BM (eds) The Qualitative ResearcherÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Companion. Thousand Oaks, CA: Sage Publications, pp. 217ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 70.
- Robinson M (2001) Communication and Health in a Multi- Ethnic Society. Bristol: Policy Press.
- Schou KC and Hewison J (1999) Experiencing Cancer: quality of life in treatment. Buckingham: Open University Press.
- Scott S, Prior L, Wood F et al (2005) Repositioning the patient: the implications of being ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âat risk.ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Social Science and Medicine 60:1869ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â79.
- Sedgwick JEC, Pearce AJ and GullifordM (2003) Evaluation of equity in diabetes health care in relation to African and Caribbean ethnicity. Ethnicity and Health 8:121ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â34.
- Selby P (1996) Cancer clinical outcomes for minority ethnic groups. British Journal of Cancer 29(Suppl.):S54ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â60.
- Shaw A (2009) Negotiating Risk: British Pakistani Experiences of Genetics. Oxford: Berghahn Books.
- Silverman D (2001) Interpreting Qualitative Data: methods for analysing talk, text and interaction. London: Sage Publications.
- Sontag S (1978) Illness asMetaphor.Harmondsworth:Penguin.
- Srinivasa J, Rowett E, Dharni N et al (2007) Improving access to cancer genetics services in primary care: socioeconomic data from North Kirklees. Familial Cancer 6: 197ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â203.
- Taylor C (1994) Multiculturalism: examining the politics of recognition. Princeton, NJ: Princeton University Press.
- Tudor Hart J (1971) The inverse care law. Lancet 1:405ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â12.
- Velikova G, Booth L, Johnston C et al (2004) Breast cancer outcomes in South Asian population of West Yorkshire. British Journal of Cancer 90:1926ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â32.
- Walter FM, Emery J, Braithwaite D et al (2004) Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Annals of Family Medicine 2:583ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â94.