Commentary Article - (2023) Volume 0, Issue 0
Received: 01-Dec-2023, Manuscript No. IPP-23-18495; Editor assigned: 04-Dec-2023, Pre QC No. IPP-23-18495 (PQ); Reviewed: 18-Dec-2023, QC No. IPP-23-18495; Revised: 25-Dec-2023, Manuscript No. IPP-23-18495 (R); Published: 31-Dec-2023, DOI: 10.51268/1590-8577-23.S9. 004
Although endoscopic treatment of symptomatic Post-Inflammatory Pancreatic and Peripancreatic Fluid Collections (PPPFCs) is a minimally invasive method of choice, some aspects of endoscopic treatment and periprocedural management remain matter of debate. Despite the state of current knowledge and data available in literature the use of antibiotics during interventional treatment of local consequences of pancreatitis is still a matter of debate.
Antibiotic therapy is a crucial element in the conservative treatment of acute pancreatitis [1-3]. The main indication for the antibiotic therapy in patients with acute pancreatitis is confirmed pancreatic or extrapancreatic infection [1-3]. In some cases antibiotic therapy may lead to complete regression of infected PPPFCs without need for interventional treatment [1]. Other indications for use of antibiotics in acute pancreatitis remain unclear.
The use of prophylactic antibiotics, in order to prevent infection of necrotic tissues, are not recommended in patients with acute pancreatitis [1-4]. Their general use in acute pancreatitis remains controversial despite many publications. Moreover, the best duration time of antibiotic therapy in pancreatitis remains unclear, despite international guidelines concerning treatment of pancreatitis. Similar controversies also regard the use of antibiotics in gastrointestinal interventional endoscopy. The importance of prophylactic antibiotics during interventional endoscopic procedures in the pancreatic diseases is still unknown. At the moment, there are no clear guidelines regarding the necessity for periprocedural antibiotic prophylaxis or duration time.
In our randomized trial an attempt was made to define the role of antibiotics in the endoscopic treatment of PPPFC [5]. 62 patients treated endoscopically for PPPFCs in our medical center were divided into two groups. Group 1 consisted of patients with symptomatic PPPFCs who had received empirical intravenous antibiotic therapy during endotherapy. On the contrary: group 2 consisted of patients who did not receive antibiotic therapy during endotherapy of symptomatic PPPFCs [5]. No differences were showed in the trial with regard to efficacy and safety of endoscopic treatment of PPPFCs [5]. Moreover, long-term success was comparable in both groups of patients [5].
Effective endoscopic transmural drainage of PPPFCs (Figure 1) provides means of controlling infection [5]. If the endoscopic drainage of infected PPPFCs is effective, no additional use of antibiotics is required [5]. Furthermore, if endoscopic drainage of primary sterile PPPFCs is efficient, there is no need for prophylactic or periprocedural use of antibiotics [5]. This study showed that effective endoscopic drainage of sterile PPPFCs requires no preventive or prophylactic use of antibiotics [5]. Infection control is a crucial element of successful treatment of contaminated or infected PPPFC. Antibiotic therapy is the basis of conservative treatment for infected PPPFCs and is responsible for controlling the infection [5]. When endoscopic (interventional) treatment of infected PPPFCs is initiated, effective transmural drainage determines the control of infection; thus, antibiotic treatment is no longer required [5]. If endoscopic transmural drainage of infected PPPFCs is effective, there is no need for antibiotic therapy.
Independently of minimally invasive technique used in interventional treatment of the local complications of acute pancreatitis, the base of interventional treatment relies on effective drainage of the liquid contents [6-10]. Successive drainage allows the free outflow of liquid content from the collection [6-10]. The adequate choice of drainage system is pivotal for the effective treatment of consequences of pancreatitis, such as PPPFCs [6-10]. That is why effective drainage prevents proliferation of microorganisms by continuously draining the liquid contents from the collection during interventional treatment. The antibiotic prophylaxis and antibiotic treatment are not necessary for sterile and infected collections during effective endoscopic treatment [5].
According to our knowledge, this is the first randomized trial to prove that the effective endoscopic drainage of sterile PPPFCs requires no preventive or prophylactic use of antibiotics [5]. In case of infected PPPFCs, antibiotic therapy is not necessary for successful endoscopic transmural drainage [5]. In summary the effective endoscopic drainage of PPPFCs reduces the use of antibiotics in everyday clinical practice, which is consistent with the principles of rational antibiotic therapy [5]. Nevertheless, issue still remains topic of discussion and future smulti-center studies with larger sample sizes are required to validate our results.
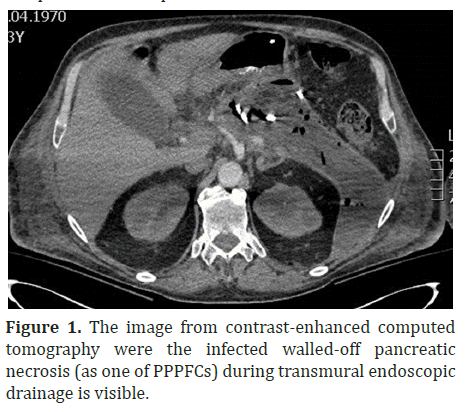
Figure 1: The image from contrast-enhanced computed tomography were the infected walled-off pancreatic necrosis (as one of PPPFCs) during transmural endoscopic drainage is visible.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.