- (2010) Volume 11, Issue 6
Jai Dev Wig1, Vikas Gupta1, Rakesh Kochhar2, Rudra Prasad Doley1, Thakur Deen Yadav1, Kuchhangi S Poornachandra2, Kishore Gurumoorthy Subramanya Bharathy1, Naveen Kalra3
Departments of 1General Surgery, 2Gastroenterology and 3Radiodiagnosis, Postgraduate Institute of Medical Education and Research. Chandigarh, India
Received April 30th, 2010 - Accepted July 13th, 2010
Context Non-operative strategies are gaining preference in the management of patients with severe acute pancreatitis. Objective The present study was undertaken to evaluate the efficacy of a non-operative approach, including percutaneous drainage, in the management of severe acute pancreatitis. Design Prospective study. Setting Tertiary care centre in India. Patients Fifty consecutive patients with severe acute pancreatitis were managed in an intensive care unit. Interventions The patients were initially managed conservatively. Those with 5 cm, or more, of fluid collection having fever, leukocytosis or organ failure underwent percutaneous catheter drainage using a 10 Fr catheter. Those not responding underwent a necrosectomy. Depending on the outcome of their supportive care, the patients were divided into three groups: those responding to intensive care, those needing percutaneous catheter drainage and those requiring surgical intervention. Twelve patients were managed conservatively (Group 1) while 24 underwent percutaneous catheter drainage (Group 2), 9 of whom were not operated (Group 2a) and 15 of whom underwent necrosectomy (Group 2b). Fourteen patients were operated on directly (Group 3). Main outcome measures Hospital stay, intensive care unit stay, and mortality. Results Among patients requiring surgery, the patients in Group 2b had a shorter intensive care unit stay (22.1±11.1 days) as compared to the patients in Group 3 (25.0±15.6 days) and a longer interval to surgery, 30.7±8.9 days versus 25.4±8.5 days. However, these differences did not reach statistical significance (P=0.705 and P=0.133, respectively). The two groups did not differ in terms of mortality (5/15 versus 3/14; P=0.682). Conclusion The use of percutaneous catheter drainage helped avoid or delay surgery in two-fifths of the patients with severe acute pancreatitis.
Drainage; Pancreatitis, Acute Necrotizing
CECT: contrast-enhanced computed tomography; CRP: C-reactive protein; CTSI: CT severity index
Severe acute pancreatitis has high morbidity and mortality [1, 2] with multisystem organ failure being the main source of this substantial morbidity and mortality [3, 4]. The selection of optimal treatment strategy is a challenge [5] and early surgical intervention is associated with a poor outcome [6, 7, 8]. Current recommendations on the management of severe acute pancreatitis underscore the importance of non-operative strategies and delayed surgical intervention [9, 10, 11, 12, 13, 14]. Success with nonoperative management has led to it becoming a more acceptable practice even in patients with infected necrosis [5, 15]. Changes in management which have contributed to a decreased mortality rate include medical treatment aimed at reducing systemic inflammatory response and multisystem organ dysfunction (aggressive supportive intensive care, fluid replacement, enteral nutrition, antibiotics) [1, 5], image-guided percutaneous catheter drainage of collections [16] and delayed surgical intervention [17, 18]. In their prospective randomized controlled trial comparing early (within 72 hours) with late (at least 12 days after onset) surgery in patients with severe acute pancreatitis, Mier et al. [8] had a mortality rate of 56% and 27%, respectively. They observed a better outcome when surgery was delayed. In an analysis of 167 patients, Rodriguez et al. [19] reported that postponing surgery for more than 28 days after the onset of disease improved survival (5% vs. 20%). Dong et al. [20] reported a mortality of 41.7% in the early surgery group (within 3 days) and 9.8% in delayed surgery group (more than 2 weeks). De Waele et al. [21] have also observed a trend towards higher mortality in patients operated upon early in the course of the disease.
A high success rate with effective conservative treatment and a decreased number of surgical interventions has also been observed by other researchers [22, 23, 24]. In a study analyzing the success rates of conservative treatment and surgical intervention over two time periods (1999-2002 and 2003-2006), surgical intervention was performed in 19% in the second period (2003-2006) as compared to 41% in the first period (1999-2002) and the success rate was significantly better in the latter period [25]. Image-guided percutaneous catheter drainage has recently been used to supplement intensive conservative treatment and it has, in fact, led to avoiding surgical intervention in a substantial proportion of patients [16]. We hypothesized that the use of percutaneous drainage may decrease the need for surgery in some patients with severe acute pancreatitis.
The present study is based on the prospectively collected data of 50 patients with severe acute pancreatitis managed at a tertiary care centre in North India between June 2006 and December 2007. Acute pancreatitis was diagnosed on the basis of clinical features, elevated serum amylase and/or lipase and raised serum C-reactive protein (CRP) levels. Severe acute pancreatitis was defined according to the Atlanta criteria [26] with a CT severity index (CTSI) greater than 7 [27]. Contrast-enhanced computed tomography (CECT) was used for documentation of the pancreatic necrosis, and severity scoring was done by calculating CTSI [27].
All the patients were initially managed with fluid resuscitation, organ system support, pain alleviation and prophylactic antibiotics (ciprofloxacin and metronidazole or imipenem/cilastatin). Nutritional support (enteral or parenteral) was instituted within 72 hours of admission. The route of administration was governed by the clinical condition of the patient. Enteral feeding was administered via a feeding tube inserted into the jejunum under endoscopic guidance. Additional antibacterial therapy was instituted according to the culture reports of percutaneous aspiration, drainage fluid, blood, urine or operative specimens. All the patients were closely monitored for organ failure and sepsis. Imaging (ultrasound and/or CT) was performed periodically to monitor the extent of the necrosis, spread of inflammation and fluid collection.
Patients who improved clinically with no fever or organ failure were continued on conservative management. Those who had persistent infection, infected necrosis, persistent organ failure or clinical deterioration were considered for radiologically-guided percutaneous catheter drainage or surgery. In patients with a pancreatic/peripancreatic collection of 5 cm, or more, in size, and having persistent fever, leukocytosis or organ failure, an ultrasound/CT-guided drainage was instituted with a 10 Fr catheter using the tandem trocar technique via the most direct transperitoneal route, avoiding involvement of the bowel and solid organs. Prior to the procedure, a transfusion of platelets and fresh frozen plasma, and an injection of vitamin K was given to correct coagulation deficiencies (if needed). Catheters were placed for gravity drainage and were routinely irrigated with 20 mL normal saline every 12 hours. After catheter placement, radiological assessment was carried out periodically to check the efficacy of the drainage, need for flushing and repositioning. Repeat CECT scans were performed when necessary, and clinical and laboratory markers were monitored to evaluate the need for surgical intervention. The catheters were removed when drainage was less than 10 mL for two consecutive days. The criteria for successful management were control of sepsis, resolution of collection, and no necessity of surgical intervention.
Surgical intervention was undertaken either when clinical deterioration or locoregional complications occurred, despite percutaneous catheter drainage (no. 15) or among patients not undergoing percutaneous catheter drainage, who had infected pancreatic necrosis or persistent/worsening organ failure (no. 14). The surgical procedure consisted of a blunt necrosectomy and closed lesser sac lavage. The timing of the intervention, intensive unit care stay, hospital stay and mortality rates were recorded.
The study was approved by the Ethics Committee on Research of the Institute. Oral informed consent was obtained from all patients. The study protocol conforms to the ethical guidelines of the “World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004.
The data were tabulated and the results were expressed as numbers and percentages of the totals for the categorical data, and mean ± standard deviation for the continuous data. The Kruskal-Wallis and the chisquared tests were used to compare the four different groups. Post hoc tests were used to study the differences between the individual groups whenever the differences between the four groups were significant. The Mann-Whitney and the Fisher’s exact tests were used for the post hoc analyses. A two-tailed P value of less than 0.05 was considered statistically significant.
A total of 50 patients with severe acute pancreatitis (27 males, 23 females; age range: 17-70 years, 39.7±12.6 years) were studied. The etiology was excessive ethanol use in 19 (38.0%), gallstones in 23 (46.0%), drug induced in 2 (4.0%, and idiopathic in 6 (12.0%). Serum amylase was elevated in 38 (76.0%) and serum lipase was elevated in 44 (88.0%) patients. All patients had CECT evidence of acute pancreatitis with a CTSI greater than 7. The patients were managed in the intensive care unit and, depending on the outcome of the supportive care, they were divided into three main groups: those responding to intensive care, those undergoing image-guided percutaneous intervention and those undergoing surgical intervention following failure of the non-surgical treatment as per the indications listed above. Out of 50 patients, 12 (24.0%) were managed with supportive intensive care management (Group 1) while 24 (48.0%) underwent image-guided percutaneous drainage (Group 2). Of the latter, 9 patients (37.5%) recovered and did not require surgery (Group 2a) while 15 (62.5%) were operated on (Group 2b). In 14 patients (28.0%), surgery was performed after the failure of conservative management (Group 3) (Figure 1).
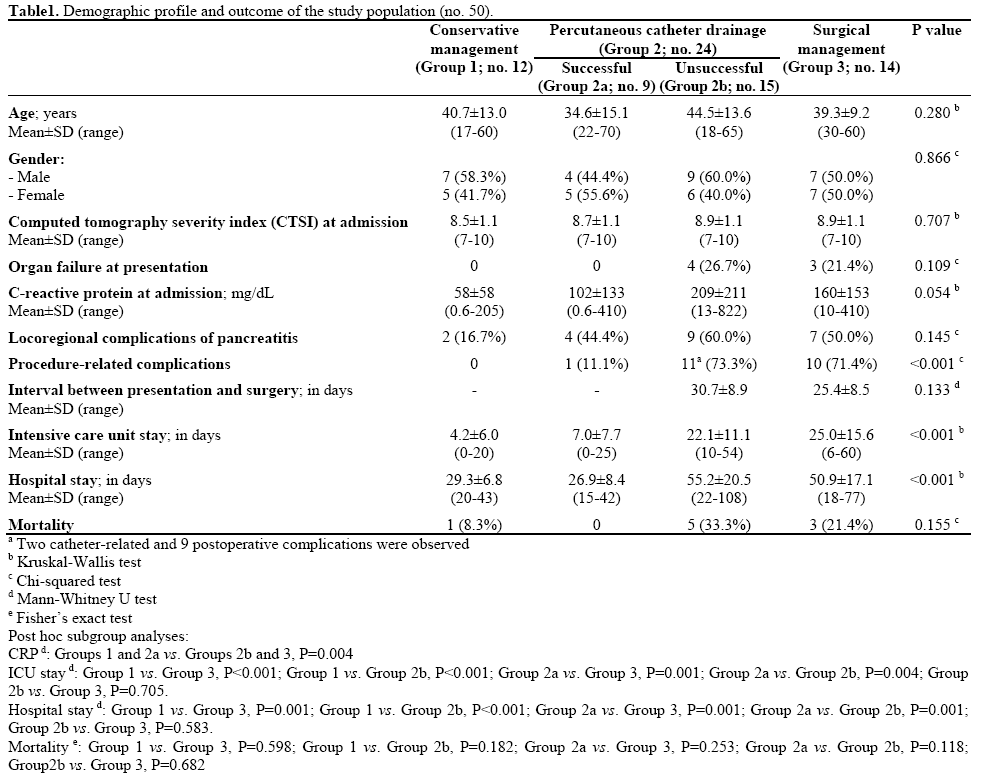
There was no significant difference in the demographic parameters and CTSI at admission in these groups (Table 1). Only Group 2b and Group 3 patients had organ failure at presentation with no differences between the two (P=1.000).
Patients Managed Non-Operatively
Non-operative strategy was first used in 36 patients (72.0%): 12 patients were managed with supportive treatment alone (Group 1) and 24 patients were managed with supportive treatment and image-guided percutaneous catheter drainage (Group 2). Only two patients in Group 1 had a locoregional complication (16.7%). Eleven patients in Group 1 made an uneventful recovery (91.7%) while one patient (a 46- year-old male) died from an acute coronary event after 21 days of hospital stay.
Image-Guided Percutaneous Intervention
Twenty-four patients (48.0%) underwent image-guided drainage of the pancreatic/peripancreatic collections. Nine of these patients (37.5%) were successfully managed by radiological intervention only (Figure 2) while 15 (62.50%) continued to have or developed infection, persistent organ failure or locoregional complications. These 15 patients were subsequently operated upon (Figure 3). There were a total of 11 procedure-related complications in these patients (73.3%) with two patients having catheter slippage which required repositioning (Table 1).
Figure 3. a. Well-defined collection within the pancreas in a patient with gallstone-induced pancreatitis on the 21st day (nasojejunal tube is seen in the duodenum). b. Percutaneous catheter inserted the next day. c. Sixteen days later, the collection showed regression but the inflammation persisted. The patient had deteriorated and was operated on.
Surgical Management
Twenty-nine patients were operated on as a result of unsuccessful supportive treatment (Group 3, no. 14) and percutaneous drainage (Group 2b, no. 15). Indications for surgery in Group 2b were infected necrosis (no. 10; 66.7%), organ failure (no. 4; 26.7%) and abdominal compartment syndrome (no. 4; 26.7%) (some patients had more than one indication). In Group 3, the indications for surgery were infected necrosis (no. 8; 57.1%), organ failure (no. 5; 35.7%) and abdominal compartment syndrome (no. 5; 35.7%) (some patients had more than one indication). There was no significant difference between those operated on without percutaneous drainage (Group 3) and those after unsuccessful percutaneous catheter drainage (Group 2b) in terms of organ failure at admission (P=1.000), locoregional complications (P=0.715) and total hospital stay (P=0.583). However, those with percutaneous catheter drainage had delayed surgical intervention (30.7±8.9) when compared to those directly operated upon (25.4±8.5 days) although this difference was not statistically significant (P=0.133). The intensive care unit stay (P=0.705) was similar between the two groups (Table 1).
The CTSI at admission was similar between the 21 patients who were first managed non-operatively (Groups 1 and 2a: 8.6±1.1) and the 29 patients who underwent surgery (Groups 2b and 3: 8.9±1.1) (P=0.279). CRP levels at admission were significantly higher (P=0.009) in the patients who required surgery (186±184 mg/dL) when compared to those who were managed conservatively (77±97 mg/dL). The ICU stay in patients managed non-operatively was 5.4±6.8 days (range: 0-25 days) and 23.5±13.3 days (range: 6-60 days) in those operated on. The hospital stay in nonoperated patients was 28.2±7.4 days (range: 15-43 days) while it was 53.1±18.7 days (range: 18-108 days) in those who were operated on. The patients who were managed non-operatively had a significantly lower ICU stay (P<0.001) as well as a significantly lower total hospital stay (P<0.001).
The overall mortality was 9 (18.0%), with 8 out of 9 deaths occurring after necrosectomy (8/29, 27.6%). Among those who were managed only conservatively (Group 1), one patient died from a cause unrelated to his basic disease while in the group managed successfully by radiological intervention (Group 2a), there were no mortalities. Among the operated patients, 5 (33.3%) of the 15 patients operated on after percutaneous catheter drainage (Group 2b) died while 3 (21.4%) of the 14 patients operated on after failure of conservative management (Group 3) died (P=0.682).
Image-guided drainage is reported to obviate not only the need for subsequent surgery but also decreases the severity of illness and improves organ dysfunction in these patients [16]. Our results show that percutaneous catheter drainage was helpful in 24 (48.0%) of our 50 patients, in 9 (18.0%) patients by avoiding surgery altogether and in the other 15 (30.0%) patients by delaying surgery and facilitating subsequent debridement. Freeny et al. [28] reported that 47% of their patients were cured with percutaneous catheter drainage alone and only 24% of the patients required surgical necrosectomy. Navalho et al. [29] reported a cure rate of 63% following percutaneous catheter drainage with 33% of their patients requiring surgery after failure to show clinical improvement following percutaneous catheter drainage. Moertle et al. [30] have shown that percutaneous catheter drainage could act as a bridge to surgery in 7 of their 13 patients with infected pancreatic necrosis. Our results are in accordance with the above observations. Fifteen of our 29 patients requiring surgery had undergone percutaneous catheter drainage and the interval between admission and surgery was approximately 4 days more as compared to those operated on directly. Bruennler et al. [11] observed that percutaneous therapy can stabilize patients long enough to be able to postpone surgery or even to avoid surgery. Olah et al. [31] had results similar to ours, with 20% of their patients recovering after percutaneous catheter drainage alone and, in the rest, percutaneous catheter drainage postponed surgery [31]. Two reports, including a review of 212 patients, have suggested that timely percutaneous catheter drainage can reduce mortality in patients with severe acute pancreatitis [16, 18]. However, a recent study has questioned the benefits of percutaneous catheter drainage [32]. They have reported that the use of percutaneous catheter drainage did not improve the mortality rate of necrotizing pancreatitis among patients with organ failure.
Percutaneous catheter drainage was carried out using 10 Fr pig-tail catheters in our study. Larger size catheters have been used by some researchers, but with an added risk of complications. The advantage of using larger catheters is that they can be used for percutaneous or sinus track necrosectomy. In a recent study from Germany, Bruennler et al. [33] reported their experience with percutaneous catheter drainage employing multiple larger bore drainage catheters to delay or avoid surgery. They combined percutaneous catheter drainage with percutaneous necrosectomy in 18 of their patients, although 10 of them required subsequent open necrosectomy. They used drainage catheters having a median cumulative diameter of 30 Fr. They observed that large bore drainage did not prove to be more effective in controlling the septic focus. Moertele et al. [30] used a mean catheter size of 12 Fr (range: 7-22 Fr), with the average number of catheters used per patient being 3.3. However, in a recent study, 13 patients received ultrasound-guided percutaneous catheter drainage treatment with a catheter size ranging from 8 to 10 Fr with no mortalities [16]. A chronological series of CT images showed that the necrotizing pancreatitis was completely cured and no catheter-related complications occurred [16].
The main complications of percutaneous catheter drainage are bleeding, perforation of the viscera and slippage of the catheter [33]. Hemorrhage is quite uncommon and may be due to the pancreatitis itself rather than the percutaneous catheter drainage [34, 35]. Arterial pseudoaneurysms or active hemorrhage due to vascular injury requires arterial embolization [34, 35]. Venous bleeding is usually self limiting [35]. Fistulization of the bowel could be due to the spread of peripancreatic inflammation or inadvertent bowel injury during catheter insertion [35]. We encountered catheter slippage in three of our patients and, in all of them, the catheter was able to be repositioned. Similar to Moertele et al. [30], we ensured a platelet count of at least 50,000 mm-3 and an international normalized ratio of 1.5 or less before the procedure was undertaken. We did not have hemorrhage in any of our patients.
Another strategy in the management of severe acute pancreatitis is the use of endoscopic drainage of infected acute fluid collections [36, 37, 38, 39, 40]. In a study of 31 patients, non surgical management was undertaken in 23 patients, 18 with percutaneous catheter drainage and 5 with endoscopic drainage [41]. The authors concluded that non-surgical drainage could be useful in avoiding surgery in some patients with infected pancreatic necrosis. A recent study has shown an initial success rate of transgastric endoscopic necrosectomy of 80% with a 26% complication rate and a 7.5% mortality rate at 30 days [14]. Endoscopic ultrasonographic-guided drainage techniques [40] and image-guided percutaneous drainage [16] have the potential of offering a safe and effective alternative treatment modality. The precise role of these techniques requires further evaluation.
Our study has a few limitations. The decision to allocate patients to percutaneous catheter drainage or surgery was subjective and there could be an element of bias in that. We did not undertake severity scoring using the APACHE score or the Ranson’s score. We restricted our drainage to a single 10 Fr catheter. Increasing the catheter size or the number of catheters might have benefited a few more patients. The number of patents in each group turned out to be small in which was not an ideal situation for statistical analysis.
In conclusion, our study evaluates the success of nonoperative management strategies in patients with severe acute pancreatitis. In this report, 40% of the patients were able to be successfully managed with a non-operative approach, thus avoiding surgical intervention in these critically ill patients. Surgical intervention could be delayed in nearly half of the remaining patients. Percutaneous drainage must be incorporated into a conservative therapeutic strategy. Surgical intervention is necessary in patients whose disease cannot be controlled with a conservative strategy. Thus, an interdisciplinary approach and timely aggressive intensive care may result in a significant reduction in mortality in patients with severe acute pancreatitis.
Financial disclosure Nil
Conflict of interest Nil for all authors
Grant support Nil