Abstract
Introduction: Patent ductus arteriosus has very diverse morphology and sometimes
it becomes challenging at times to occlude along with certain complications.
Transcatheter closure of PDA is the procedure of choice and is considered safe.
Various devices develop to occlude PDA because of diverse morphology. These
devices are usually designed according to the anatomical types of PDA.
Objective: The objective of this study is to observe the residual leak within 24
hours after device occlusion of PDA in the pediatric age group by using different
devices in diverse morphology of PDA.
Methods: A cross-sectional observational study with consecutive sampling
was conducted in the cardiology department to evaluate the results of PDA
device occlusion regarding residual leaks by using different devices at children's
hospital and institute of child health Lahore. The data was collected for 6 months
after approval of synopsis between 6 months to 16 years of age by developing
Performa. All the data was entered in SPSS version 25 software and then analyzed
for statistically significant outcomes. Descriptive analysis and the Chi-Square test
were applied to measure the association among the different categorical variables.
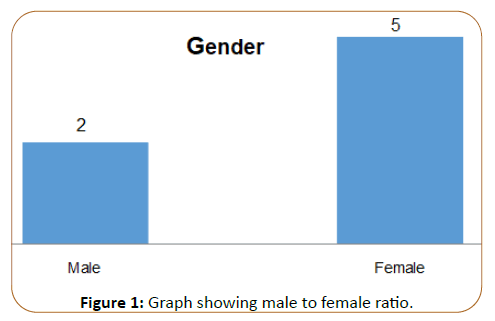
Results: A total of 79 patients with a male to female ratio of 1:2 selected in the
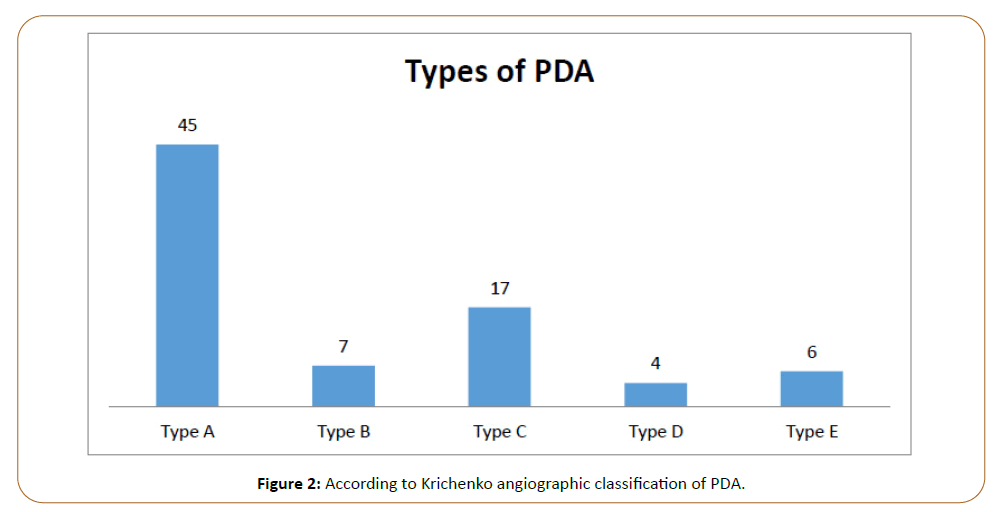
study were admitted for duct occlusion. According to Krinchenko classification,
45 patients had type A, 7 patients had type B, 17 patients had type C, Four
patients had type D, and 6 patients had type E PDA. In 50 patients regular shape
duct occluder was used. The result revealed 4 patients have a residual leak. In 29
patients reverse shank duct occluder was used, out of which 7 patients have a
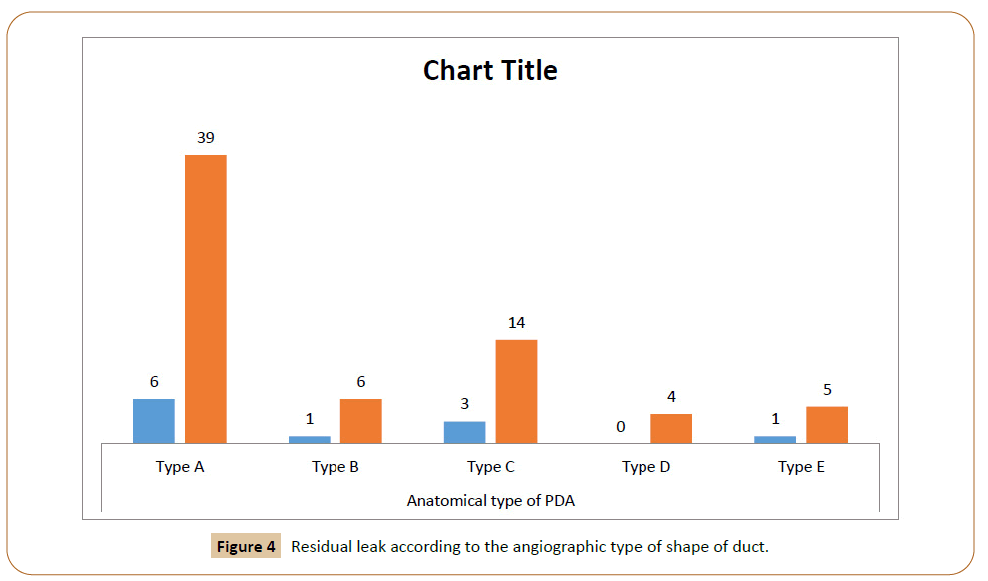
residual leak. As far as anatomical types of PDA were concerned versus residual
leak, in type A 6 patients have a residual leak, in type B and E 1 patient has a
residual leak, while in type C PDA 3 patients have a residual leak and in type D no
leak was observed.
Keywords
Patent ductus arteriosus; Duct occlude; Standard shank; Reverse
shank; Angiography
Introduction
Patent Ductus Arteriosus (PDA) is a common cardiac defect
with an incidence of 6%-11% [1] Symptomatic PDA requires
treatment in the form of medicine as well as an intervention
[2]. Transcatheter closure of PDA considers being safe and
preferable nowadays [3]. Cardiac catheterization was first used
to treat PDAs in 1966 [4]. Recently various types of duct occluder
devices are available for PDA occlusion [5]. Ductus arteriosus persists in a wide variety of sizes and configurations. Krichenko
et al. angiographically classified duct into five types: Type A
‘‘conical’’ ductus, with ampulla at the aorta and narrow point at
the pulmonary end. Type B ‘‘window’’ ductus, with no ampulla
and a narrow end. Type C, ‘‘tubular’’ ductus. Type D, ‘‘complex’’
ductus, with several narrowing. Type E, “elongated” ductus, with
narrowing away from the anterior edge of the trachea [6]. The
sizes, shapes, and association to other cardiac defects are the
main aspect of interventional closure. Various types of devices for PDA closure are now available. These include ADO device,
Rashkind device, SHSMA occlude, and Gianturco coil [7]. A lot of
studies done on devices effectiveness and complications but few
studies done regarding observing normal versus reverse shank
outcome spatially focus on residual leak because residual leaks
some time challenging to treat because of hemolysis, volume
load, increase chance of infective endocarditis, and re-coiling or
re-devising.
Methods and Materials
A cross-sectional observational study with consecutive sampling
was conducted in the cardiology department to evaluate the
results of PDA device occlusion at children hospital and institute
of child health Lahore. The data was collected for 6 months
after approval of synopsis between 6 months to 16 years of age
by developing Performa. Only patients with isolated PDA seem
suitable for device occlusion in echocardiography by consultant
pediatric cardiologist were selected. Those patients having
associated coarctation of the aorta or other cardiac defects,
irreversible pulmonary hypertension, neonates, and premature
babies were excluded from the study.
Duct occluder classification
Proforma was designed to focus on the angiographic types of
PDA and residual leak between standard shank and reverse shank
duct occluder used for the different types of PDA. The reverse
shank duct occluder has a wider pulmonary end than the aortic
end while in normal shank aortic end is wider than the pulmonary
end. The devices used for standard shank were Life tech, Amplatzer
AGA and Shsma. While for the reverse shank, Occlutech was used.
Device size selection
To date, there is no clear guidance on how to select the size of
a duct occluder. Most operators elect to implant devices at
least 2 mm larger than the narrowest point of the duct [8,9].
For the selection of the size of duct occluder as standard, 2 mm
bigger than the narrow point was preferred in low pulmonary
artery pressure while more than 4 mm of the narrow point was
preferred in case of moderate to severe pulmonary hypertension
[10]. Similarly, duct length measurement from ampulla to narrow
point was measured [11]. We repeat angiography always after
crossing with the delivery system and re-measured narrow point
before selection of the size of the device.
Angiography
PDA device closure was done under universal aseptic condition
through the femoral artery and venous approach. Heparin with
100 u/kg was given before the start of the procedure. In children
below 7 months procedure was done under general anesthesia.
While children above 7 months the procedure is done in local
anesthesia with sedation. A full lateral view of Aortic angiogram
(90 LAO) was performed to determine the morphology and size
of the duct. Sometimes the shape was confirmed at 30 RAO view
also. The size of the ampulla, narrow point, and length of the duct
was measured at both 90 LAO and 30 RAO angiogram. Both aortic
and pulmonary artery pressure was measured before the selection
of the device. Device type and size were selected after reviewing
the aortogram and pulmonary artery pressure by consensus
of two consultant’s pediatric cardiologists. The position of the device was reconfirmed before releasing through angiography by
contrast media at both 90 LAO and 30 RAO views. The position of
the device was also confirmed through angiography by contrast
again at 90 LAO and if required then 30 RAO position. Immediate
complication like LPA or aortic partial obstruction was confirmed
by pullback gradient at ascending and descending aorta and LPA
distal to proximal gradient by Cather. The side leak not foaming
through the device was labeled as residual leak after 24 hours
post-procedure through echocardiography by a consultant
pediatric cardiologist. Hemolysis was rule out through clinical
status and urine examination before discharge.
Statistical analysis
All the data entered in SPSS version 25 softwares and then
analyzed for statistically significant outcomes. Descriptive analysis
and the Chi-Square test were applied to measure the association
among the different categorical variables.
Results
The male to female ratio was 1:2 Figure 1. The mean age of patients
in years was ± 4.05 years with a minimum age of 8 months, the
mean weight of patients was ± 13.72 kg. The standard deviation of
height was ± 27.01 cm. The mean narrow point of the duct was
3.27 mm with a range of ± 1.4 mm to 8.8 mm while the ampulla
was ± 1.4 mm to 20 mm. Regarding device selection, the average
aortic end diameter of the device to pulmonary end diameter of
the device found was ± 3 mm-16 mm to ± 3.5 mm-18 mm. The
mean of aortic end to PDA diameter ratio was 2.6 with an average
of ± 0.96 mm-7.14 mm. Similarly, the mean of the maximum
device to PDA diameter ratio found was ± 1.74 mm to 7.1 mm Table 1. Out of 79 patients, according to Krichenko angiographic
classification of PDA, 45 patients had Type A shape, 7 patients
had Type B, 17 patients had Type C, 4 patients had type D, and 6
patients had Type E angiographic shape Figure 2. Regarding the
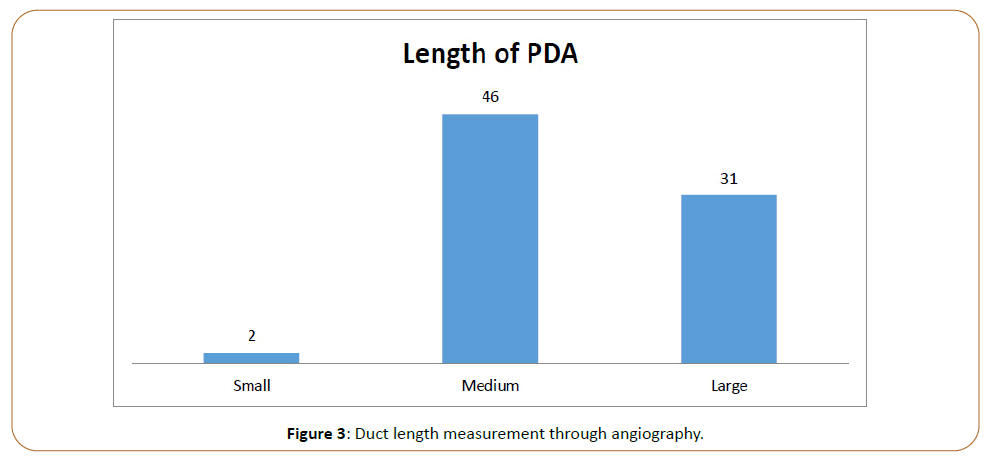
length of the duct, only two patients had a small length (≤ 4 mm)
while 46 patients had a medium length (7 mm), and 31 patients
had a long length (≥ 7 mm) Figure 3. Out of 50 patients in whom
regular shape duct occluder devices were used, 4 patients had
a residual leak in PDA. While from 29 patients in which reverse
shank device was used 7 patients had a residual leak. According
to Krinchenko angiographic classification of PDA, 6 patients had
a residual leak in type A, 1 patient had a residual leak in type-B, 3
patients had a residual leak in type C. No residual leak was seen in
type D shape of PDA and in type E shape 1 patient has a residual leak Figure 4. Regarding residual leak with reverse shank, the
maximum residual leak was seen in type A and type C PDA Table
2. Another complication like early embolization, hemolysis, aortic
or LPA obstruction was not seen in our case within 24 hours.
Figure 1: Graph showing male to female ratio.
Figure 2: According to Krichenko angiographic classification of PDA.
Figure 3: Duct length measurement through angiography.
Figure 4: Residual leak according to the angiographic type of shape of duct.
| Demographics |
Mean |
Std. Deviation |
Range |
Minimum |
Maximum |
| Age (year) |
4.0544 |
2.88825 |
12.2 |
0.8 |
13 |
| Weight (kg) |
13.7215 |
7.62144 |
48.5 |
2.5 |
51 |
| Height (cm) |
93.0633 |
27.01156 |
149 |
11 |
160 |
| PDA narrow point (mm) |
3.2785 |
1.4128 |
7.4 |
1.4 |
8.8 |
| PDA ampulla (mm) |
11.1814 |
3.39878 |
19.4 |
1.4 |
20.8 |
| Aortic end diameter of device (mm) |
8.0506 |
2.79605 |
13 |
3 |
16 |
| Pulmonary end diameter of device (mm) |
7.6013 |
2.50305 |
14.5 |
3.5 |
18 |
| Device aortic end to PDA diameter ratio(mm) |
2.6484 |
0.93715 |
6.18 |
0.96 |
7.14 |
| Max device to PDA diameter ratio |
2.9119 |
0.86015 |
5.36 |
1.74 |
7.1 |
|
Table 1: Demographic data of Patients post-duct angiographic measurement (n-79).
| Type of Devices |
Type-A |
Type-B |
Type-C |
Type-D |
Type-E |
| Normal shank |
1 |
1 |
1 |
0 |
1 |
| Reverse shank |
5 |
0 |
2 |
0 |
0 |
| Total shank |
6 |
1 |
3 |
0 |
1 |
Table 2: Residual leak in normal versus reverse shank duct occluders in different shape of PDA.
Discussion
The reverse shank is designed to enhance the stability of the
device in the duct and decrease the risk of embolization. It is
present in two different lengths, the standard length and the long
shank device made for long ductal ampulla [11]. Residual shunt
through the reverse shank device as described in the literature.
Excellent occlusion rates have been reported at 1 day (82%-97%),
1 month (96%-100%) and 6 months (96%-100%) follow up [12].
Similarly, reverse shank showed a higher incidence of a residual
leak than standard shank devices in our study as 8% found in
standard shank device versus 24% in reverse shank device,
which was supported by Kudumula V study. It was also reported
immediate ductal occlusion did not occur by using the ODO [12].
Some studies revealed that there was only a 48.5% complete
occlusion rate at 10 minutes post-implant, but in large ducts,
complete occlusion occurred till 90 days [13]. But in our study, we
found immediate occlusion rate within 10 minutes with all types
of devices was 86% while with only ODO it was 76%. A study also
documented that immediate complete occlusion with ODO was
63% [14]. We had a better occlusion rate in our study with ODO as mention it was 76%. We have a better implant technique as it
may be due to repeat angiography always after crossing with the
delivery system and re-measured narrow point before selection
of the size of the device. Reyhan et al mentioned that especially
in type B and type C oversizing measurement of the device was a
better option [14]. We also noticed that in type B and type C only
14% of patients showed residual leak because of the oversizing
technique. Regarding complication as early embolization of
device, it was documented that chance of embolization in the
large duct was always high [15,16]. In our study, there was no
embolization seen.
Conclusion
Reverse shank had a higher incidence of a residual leak in type A.
However, a regular shank device may be preferable in both Type
A and C shape ducts. The result was also comparable of both
types of devices in type A, and C patent ductus arteriosus.
Limitations
It was a single-center study. Follow-up was not included
regarding hemolysis, volume loaded, residual leak, and infective
endocarditis later on. The outcome of re-devising or coiling
results not mentions. The fate of pulmonary hypertension after
device and co-relation between residual leaks with pulmonary hypertension not assessed. Similarly, the type of device selection
was purely on the subject of availability.
Acknowledgement
Thanks to the support of our angiographer, and other staff
members of the angiography department.
References
- Mulyadi D, Dimas S, Sukman P. (2015) Transcatheter closure of patent ductus arteriosus: 11 years of clinical experience in cipto mangunkusumo hospital. Pediatr Cardiol 36:1070–1074.
- Jennifer L, Steven L, Irene Y. (2015) Treatment options for pediatric patent ductus arteriosus, systematic review and meta-analysis. Chest 148: 784- 793.
- Agnetti A, Carano N, Tchana B. (2009) Transcatheter Closure of Patent Ductus Arteriosus: Experience with a New Device. Clin. Cardiol 32: E71– E74.
- Alexi V, Böttcher W. (2010) The first closure of the persistent ductus arteriosus. Ann Thorac Surg 90 :349 - 356.
- Sheridan J, Ward J, Anderson W, Justo N. (2013) Transcatheter closure of the patent ductus arteriosus: an intentionto treat analysis. Heart Lung Circ 22: 428 – 432.
- Krichenko A, Benson N, Burrows P, Moes A, McLaughlin P, et al. (1989) Angiographic classification of the isolated, persistently patent ductus arteriosus and implications for percutaneous catheter occlusion. Am J Cardiol63: 877–879.
- Sun F, Dong F, Gong K, Zhang P, Cui T, et al. (2010) Transcatheter closure with use of the SHSMA occluder in 180 patients with congenital heart defects: preliminary results. Texas Heart Institute J 37: 531.
- Dedeoglu R, Bilici M, Demir F. (2016) Short-term outcomes of patent ductus arteriosus closure with new occlutech(R) duct occluder: A multicenter study. J Interv Cardiol 29: 325-331.
- Boudjemline Y. (2016) The new occlutech patent ductus arteriosus occluder: single centre experience. Arch Cardiovasc Dis 109: 384-389.
- Fischer G, Stieh J, Uebing A, Grabitz R, Kramer H. (2001) Transcatheter closure of persistent ductus arteriosus in infants using the Amplatzer duct occluder. Heart 86:444–447.
- Abdul S, Suhair S, Christopher D. (2019) The occlutech duct occluder :How to choose the correct device size and refine implantation technique to ensure optimal results in small and large arterial duct closure. Interv. Cardiol 11: 113–119.
- Kudumula V, Taliotis D, Duke C. (2015) The new occlutech duct occluder: immediate results, procedural challenges, and shortterm follow-up. J Invasive Cardiol 27:250-257.
- Abdelbasit A, Alwi M, Kandavello G. (2015) The new Occlutech PDA occluder: Initial human experience. Catheter Cardiovasc Interv 86:94–99.
- Reyhan D, Meki B, Fikri Z. (2016) Short-term outcomes of patent ductus arteriosus closure with new occlutechw duct occluder: a multicenter study. Journal of Interventional Cardiology 9999,1-7.
- Agrawal H, Waller R, Surendan S, Sathanandam S. (2019) New Patent Ductus Arteriosus Closure Devices and Techniques. Interv Cardiol Clin 8: 23-32.
- Sinha K, Razi M, Pandey N, Kumar P, Krishna V, et al. (2017) Prospective evaluation of the feasibility, safety, and efficacy of Cocoon Duct Occluder for transcatheter closure of large patent ductus arteriosus: A single-center study with short- and medium-term follow-up results. Anatol J Cardiol 18:321-327.