- (2008) Volume 9, Issue 2
Cara Yvonne Jeppe, Martin Derrick Smith
Department of Surgery, Chris Hani Baragwanath Hospital, Gauteng Department of Health. Johannesburg, Republic of South Africa
Received July 4th, 2007 - Accepted December 12th, 2007
Diabetes Mellitus; Malabsorption Syndromes; Pancreatic Neoplasms; Pancreatitis; Xenobiotics
Dear Sir:
There have been a substantial number of reports in the literature linking pancreatitis and pancreatic cancer to certain xenobiotics and occupations. It has been hypothesized that exposure to volatile hydrocarbons and particularly petrochemicals increases susceptibility to pancreatitis. We performed a study aimed to enumerate occupational and environmental xenobiotics described in the literature as potential risk factors for pancreatitis and to document exposures to these in chronic pancreatitis patients presenting with chronic pain for surgery.
In their editorial on a life course approach to chronic disease epidemiology Ben-Shlomo and Kuh state “Life course epidemiology has challenged the complacency of the adult lifestyle model of chronic disease risk. It has particularly acted as a catalyst for new research in the area of social inequalities in health and has helped bridge biological, psychological and social models of disease causation.” The approach they say is intuitively obvious but empirically complex [1].
Chronic pancreatitis is an aggressive and progressive disease, usually presenting with abdominal pain although the condition may be painless. Progression includes inflammatory fibrosis, patchy acinar atrophy, intraductal calcium carbonate stones, and an increased risk of diabetes, malabsorption and pancreatic cancer Long-term alcohol abuse and smoking have been cited as the major causes of chronic pancreatitis with reduced intakes of antioxidants being a compounding factor. Less common causes in the South African environment include gallstones, drugs, infections, trauma, ischemia and genetic factors. Where alcohol is not implicated and there is no record of another recognized etiological agent the disease is generally classified idiopathic. In 1986 Braganza et al. suggested that “occupational exposure to aromatic or chlorinated hydrocarbons may be relevant not only in idiopathic pancreatitis but also in alcohol-related pancreatic disease”. They supported the suggestion with evidence of recurrent symptoms after reexposure to volatile chemicals despite abstinence from alcohol [2].
Causal associations between a number of occupational and environmental xenobiotics and pancreatitis have been suggested, most of which have been found in manual workers. A multicenter historical cohort study found “The risk of pancreatic cancer is significantly elevated in subjects with chronic pancreatitis and appears to be independent of sex, country and type of pancreatitis” [3]. According to Longnecker “Epidemiological studies indicate that chemical carcinogenesis is the cause of the increasing US exocrine cancer incidence” [4].
In August 1999 a website CCINFO (https:// ccinfoweb.ccohs.ca/) search was conducted in the NIOSHTIC® (https://www.ccohs.ca/ products/databases/nioshtic.html) and OSHLINE® (https://www.ccohs.ca/products/databases/ oshline.html) databases, in order to identify industries, occupations and xenobiotics suggested to be associated with pancreatitis and pancreatic cancer in humans. The databases are produced by the US National Institute for Occupational Safety and Health and the Canadian Centre for Occupational Health and Safety (CCOHS). A table of control limits for hazardous chemical substances under the Occupational Health and Safety Act 85 (OHSA) of 1993 (https://www.info.gov.za/acts/1993/a85-93.pdf) was obtained from the South African Department of Labour.
Approval for the study was obtained from the Human Research Ethics Committee (Medical) of the University of the Witwatersrand, protocol number M050425
All consecutive patients with chronic pancreatitis presenting for surgery at the Hepatopancreaticobiliary Units of the JG Strijdom/Helen Joseph Hospital in Auckland Park and the Chris Hani Baragwanath Hospital in Soweto, Johannesburg, South Africa between January 1991 and January 2006 answered a questionnaire after verbal or written consent was obtained. Their condition was diagnosed at endoscopic retrograde cholangiopancreatography and computed tomography scan, and, in the majority, confirmed at surgery with histopathology. The interviews were conducted by a single interviewer not engaged in treatment decisions. Questions relating to lifetime employment, occupations, exposure to commonly occurring xenobiotics, clinical details and psychosocial circumstances were included in the questionnaire. Self-reports of exposure to specific xenobiotics were obtained where possible and exposures to broad categories of agents (e.g. solvents, insecticides) were obtained when the chemical names of hazardous substances were unknown. Employers’ records were not sought as most jobs occurred prior to the study, many patients had been temporary/contract and self-employed workers, and many had been unregistered or employed in the informal sector. It was therefore not possible to ascertain exposure levels.
Twenty-nine industries and more than 40 xenobiotics linked to pancreatitis in the literature were identified in the database search (Table 1). All these xenobiotics were identified as hazardous chemical substances in the OHSA list. One-hundred and 12 patients answered the questionnaire, of which 14 were female. There was one patient that declined and was excluded. The mean (±SD) age of patients was 44.4±8.7 years. Ten patients were found at surgery to have pancreatic cancer and one developed it some time after a duodenal preserving resection of the pancreas and lateral pancreaticojejunostomy (Frey procedure). Since pancreatic cancer can develop many years after the onset of chronic pancreatitis when patients may be lost to follow-up, these eleven cancer cases do not reflect the incidence of progression to cancer in this population of chronic pancreatitis patients.

Eighty-two (73.2%) of 112 patients had been employed in enumerated industries: 39 (34.8%) in one, 31 (27.7%) in two, 9 (8.0%) in three, and 3 (2.7%) in four. Forty-three (38.4%) had been employed in the automobile, engine and parts manufacture, maintenance and service, engine factories and machine operations, and the transport industries; 29 (25.9%) in the painting industry; 18 (16.1%) in agriculture and horticulture; 16 (14.3%) in the lithography and printing, and photoengraving industries, and 9 (8.0%) in wood furniture manufacture. There were between one and eight of the patients employed in each of the acetylene production, dispensing, dry cleaning, jewelry making, leather tanning, metallurgy, petrochemical, reinforced plastics, rubber, and steel milling industries (Table 1).
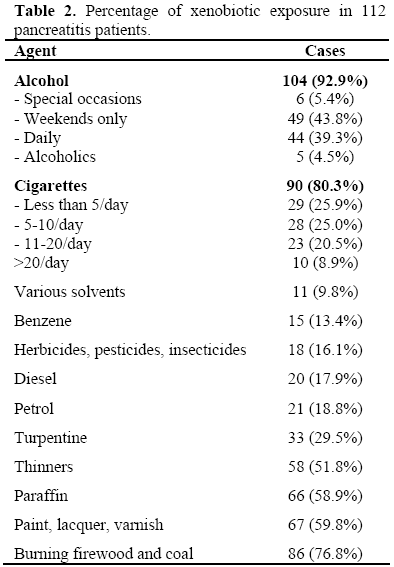
Apart from the high proportion of alcohol consumers and smokers, 11 (9.8%) of patients had been exposed to various solvents: 15 (13.4%) to benzene; 18 (16.1%) to herbicides, pesticides, insecticides; 20 (17.9%) to diesel; 21 (18.8%) to petrol; 33 (29.5%) to turpentine; 58 (51.8%) to thinners; 66 (58.9%) to paraffin; 67 (59.8%) to paint, lacquer, varnish; 86 (76.8%) to burning firewood and coal (Table 2).
Before surgery 71 (63.4%) expressed an inability to continue manual work as a result of their illness and 44 (39.3%) had been retrenched. Forty-three had diabetes (38.4%) of whom 29 (25.9%) were insulin dependent, 53 (47.3%) had steatorrhea, 96 (85.7%) loss of weight, and 57 (50.9%) expressed hopelessness prior to their surgery.
Chronic pancreatitis has been described as endemic in the township of Soweto [5] where exposure to environmental xenobiotics such as burning firewood and coal, and paraffin used in Primus stoves has historically been universal. Differentiation between occupational and confounding environmental agents would require comparison with a population of patients employed in “risk” occupations but not having been exposed to these environmental agents. In South Africa such a population does not yet exist. Furthermore since exposures may occur many years before the onset of chronic pancreatitis, and may be multifactorial but not continuous, such differentiation is impracticable
In South Africa many patients are treated empirically for epigastric pain, presumed to be due to peptic ulcer disease. Consequently the diagnosis of chronic pancreatitis tends to be made at advanced stages of the disease Diagnostic investigations such as magnetic resonance and endoscopic retrograde cholangiopancreatography, and computed tomography scan are not appropriate screening tools due to limited resources in many public health facilities, high costs, and their invasive nature. Thus exclusion of chronic pancreatitis in controls with these methods is neither practicable nor ethically acceptable.
In their case-referent study McNamee et al. identified “close exposure to volatile hydrocarbons, especially petrochemicals, as an independent risk factor in chronic pancreatitis” [6]. They attributed treatment failure partially to daily close exposure to occupational chemicals. Abstinence from alcohol would not therefore provide protection from further episodes of acute on chronic pancreatitis and progression of the disease to irreversible pancreatic insufficiency in those who continue to be exposed to such chemicals. Such evidence requires that diagnosticians routinely investigate life course exposures to volatile hydrocarbons.
In the study presented here, that was primarily designed to assess the effectiveness of painrelieving surgery for chronic pancreatitis, enthusiasm for the life course approach was frustrated by a number of obstacles that resulted in methodological weaknesses. No exposure levels for specific agents were obtainable as most patients were unable to identify them in poorly defined job categories with inadequate health and safety information. Individual exposure levels were also unavailable as employment records have been rare for manual workers and industry compliance with occupational health and safety controls has been traditionally poor. Therefore no attempt was made to access this information.
No dose-effect relationship could be determined in the study and thus only a suggested relationship between exposure and disease is postulated. The fact that the cumulation of exposures to occupational and environmental xenobiotics in this working class population of patients may reduce the effectiveness of preventive interventions (such as electrification of homes and improved compliance with workplace health and safety regulations) does not diminish the need for prevention. Joint exposure to a number of “risk” factors may not be interactive in which case the relative “risks” become multiplicative. Stringent measures to reduce “risk” exposure should be implemented to curtail the widespread incidence of a disease with such poor prognosis and grave personal and social consequences.
This audit suggests that people exposed to certain xenobiotics can develop chronic pancreatitis. However these particular agents will need to be tested in a future case-control study.
The authors have no potential conflicts of interest