- (2015) Volume 16, Issue 2
Guntars Pupelis*, Vladimir Fokin, Kaspars Zeiza, Ita Kazaka, Jelizaveta Pereca, Vita Skuja and Viesturs Boka
Department of General and Emergency Surgery, Riga East Clinical University Hospital 2Hipokrata St., LV 1038, Riga, Latvia
Received November 29th, 2014 – Accepted February 09th, 2015
Introduction The surgical treatment of necrotizing pancreatitis includes percutaneous drainage of acute necrotic collections and sequestrectomy in the late phase of the disease. The aim of the study was to compare the conventional open necrosectomy (CON) approach with the alternative focused open necrosectomy (FON) approach in patients with infected necrosis and progression of sepsis. Methods Patients with acute necrotizing pancreatitis were included in the study prospectively from January 2004 to July 2014. All patients had been admitted with the first or a new episode of disease. Symptomatic large fluid collections were drained percutaneously. The step-up approach was used in patients with several distant localizations of infected necrosis. The methods were analysed by comparing the individual severity according to the ASA, APACHE II and SOFA scores, infection rate, postoperative complication rate and mortality. Results A total of 31 patientswere included in the FON group and 39 in the CON group. The incidence of infection was similar in groups. More ASA III comorbid conditions, a higher APACHE II score, a more frequent need for renal replacement therapy was observed in the CON group. The postoperative complication rate was in the range of 32% to 44%; mortality reached 6.5% in the FON group and 12.8% in the CON group. Conclusions Comorbid conditions, organ failure, and infection are the main risk factors in patients with necrotizing pancreatitis. The step-up approach and perioperative ultrasonography navigation improves the clinical outcome and reduces the extent of invasive surgical intervention in patients unsuited to other minimally invasive procedures.
Intraoperative Care; Preoperative Care; Surgery; Ultrasonography
Sepsis control is the primary goal of surgical intervention in patients with infected necrosis. The conventional laparotomy approach is reliable when a differential diagnosis with other abdominal emergencies should be made or conservative treatment fails to manage the abdominal compartment syndrome or, in selected cases, when minimally invasive treatment (MIT) is not applicable. The development of endoscopic surgery, laparoscopy and combined approaches has enabled the application of MIT on a large scale [1]. Several types of MIT have been developed, including the endoscopic trans-gastric [2, 3], endoscopic lumbo-retroperitoneal [4], and laparoscopic approach [5]. However, based on the current experience, it is still difficult to conclude whether MIT is the best surgical approach for all patients with severe acute necrotizing pancreatitis who develop persistent organ dysfunction and severe sepsis [6]. In these cases necrosis often extends to a wide retroperitoneal area on both sides, especially in obese patients. Another limiting factor for the wider implementation of the MIT procedures is the necessity to organize a dedicated team of specialists, mostly available only in high volume centre and university hospitals. Therefore, simple surgical approaches that are easy to perform may improve treatment results in hospitals where endoscopic surgery or advanced laparoscopic surgery is not available. While postoperative mortality in patients with necrotizing pancreatitis does not exceed 14% to 20% in specialized centres of excellence, the overall post-operative mortality is reported to reach up to 39% and is associated with high post-operative morbidity [7]. The surgical strategy highly depends on the severity of sepsis and demarcation completeness [8]. Generally, a complete sequestrectomy and drainage can be achieved four weeks after the onset of the disease [9]. The most suitable surgical approach is defined by and depends on whether the surgeons have to face a well demarcated infected walled-off necrosis (WON) or poorly demarcated infected necrotic tissue [8]. After routine implementation of preoperative and intraoperative ultrasound navigation, the focused open necrosectomy (FON) method was developed in our clinic as a simplified and alternative surgical approach to MIT and the conventional open necrosectomy (CON) [10]. This surgical strategy is based on CECT, preoperative transabdominal ultrasonography mapping and percutaneous drainage of infected acute necrotic collections (ANC) with definitive surgical intervention, using small lumbo-retroperitoneal and subcostal approaches and intraoperative ultrasonography for navigation during the open intervention. The aim of this prospective pilot study was to compare the semi-open/ closed drainage laparotomy or CON with the alternative approach - FON when treating patients with infected necrosis and progression of sepsis and to prove the feasibility, safety and non-inferiority of the FON approach.
Patients who were treated at Riga East Clinical University hospital “Gailezers” with acute necrotizing pancreatitis and were operated on due to infected necrosis were prospectively included in the study during the time period from January 2004 to July 2014. All patients were diagnosed with the first or a new episode of acute necrotizing pancreatitis, which was proved by CECT after the acute phase (first week) from the onset of the disease in order to determine the presence/localization of necrosis and acute necrotic collections (ANC) according to revised Atlanta classification. CTSI was calculated to categorize the amount of necrosis and the degree of exudation; however, it is not used in the daily practice as a severity criterion. Severity assessment was done by evaluating the amount of necrosis, the degree of exudation, the distribution of ANC, the development of intra-abdominal hypertension and organ failure in the early phase, and the development of sepsis in the late phase of the disease. Physiological response to the disease was evaluated starting from the day of admission by the assessment of comorbid conditions, calculating the American Society of Anaesthesiologists (ASA) Physical Status classification System grade and APACHE II score (maximal APACHE II score was calculated for a better comparison of the severity of the disease); presence of SIRS and organ failure defined as grade ≥3 according to the Sequential Organ Failure Assesment (SOFA) score. Levels of CRP as a biochemical marker of acute phase response and Procalcitonin as a marker of sepsis were tested on a daily basis during the treatment period. Sepsis was defined as evidence of new or persistent signs of SIRS, caused by bacterial contamination of the necrotic tissue or ANC. Diagnosis of sepsis was based on a sustained or a repeated evidence of SIRS, elevation of CRP, Procalcitonin and progression of organ failure. Positive blood cultures were defined as septicaemia. Diagnosis of primary infection was proved in cases when conservative treatment failed to prevent sepsis and positive bacterial cultures were obtained during the percutaneous drainage of infected ANC or during the first surgical intervention. Instances when the contamination of the necrotic tissue or ANC was a consequence of a previously performed surgical intervention or percutaneous drainage of non-infected ANC were considered as cases of secondary infection (drainagerelated infection). Drains were the main gateway for the commensal organism infection in this category of patients.
Management and Allocation of Patients
All patients received conservative treatment during the early phase of the disease. An ultrasound-guided drainage of symptomatic ANC was performed on patients who developed an increased intra-abdominal pressure that promoted organ failure, generally respiratory and kidney dysfunction. The selection of the approach in the late phase was based on the localization and the type of necrosis, the formation of WON or ANC, the evidence of infection, the presence of comorbid conditions, and the development of organ failure and the progression of sepsis. We did not provide randomization to avoid ethical violations, but rather used the clinical consensus strategy in doubtful cases. All enrolled patients required surgical treatment because the standardized conservative treatment provided in the early phase of the disease failed to prevent infection and the development of sepsis. The patients were divided into two groups according to the provided surgical treatment. The type of the surgical approach was determined by the general condition of the patient, the localization of infected necrosis or ANC and the surgical routine. Clinical consensus was the basis for the allocation of patients to each group. Patients with infected necrosis or infected ANC who underwent perioperative ultrasound navigation and on whom surgical intervention was done through small, focused lumbo-retroperitoneal or subcostal incisions were allocated to the focused open necrosectomy (FON) group. On the other hand, patients who underwent treatment using the conventional laparotomy approach due to infected necrosis or infected ANC were allocated to the conventional surgical necrosectomy (CON) group. The FON approach was favoured for patients with a successful temporary sepsis control after preoperative percutaneous drainage of infected walled-off necrosis (WON) or ANC. The final decision to use the FON or the CON approach was based on preoperative consensus regarding the safety and technical feasibility of each approach and the decision of the operating surgeon. Three patients were treated conservatively and after the inflammatory response regression and the absence of organ failure were discharged form hospital for outpatient treatment. Patients were rehospitalized when signs of infection developed and allocated to the FON group. This novel approach was defined as an in-hospitaloutpatient- in-hospital management and was considered as a single treatment episode. Due to the small number of patients, they were not allocated to a separate group. This individualized approach resulted in the clinical separation of cases unsuitable for the FON strategy. The comparative CON group was formed with the aim of demonstrating the non-inferiority of the FON approach.
Ultrasound-Guided FON Approach
Perioperative repeated ultrasonography was used for a dynamic follow-up of local inflammatory processes and localization of fluid collections. Preoperative CECT, ultrasound mapping of incision and intraoperative ultrasound navigation were routine steps of the FON approach. Preoperative transabdominal ultrasound was performed on BK Medical (Herlev, Denmark) Pro Focus and BK Medical Viking 2400 systems with a convex probe (2-6 MHz). Ultrasound guided percutaneous ANC drainage was performed under local anaesthesia, using pig-tail catheters of 8.5-14 Fr (2.83 to 4.67 mm) inserted for temporary SIRS and sepsis control that helped to perform less traumatic surgical intervention later when it was indicated according to the step up approach principle. Intraoperative ultrasound was performed on Hawk 2102 EXL and BK Focus 800 systems with a transducer type convex probe (6.9-8.1 MHz), flexible linear probe (8.3-9.7 MHz) and micro convex probe (6.2-7.2 1 MHz). Ultrasoundguided surgery included a provision of intraoperative ultrasound and ultrasound-guided minimally invasive interventions. The main intraoperative ultrasound steps were as follows: stereotypical diagnostics ensuring the recognition of anatomical structures and its relation to ANC and necrotic tissue; intraoperative navigation – precise definition of the surgical access (Figure 1); intraoperative monitoring – ultrasonography in realtime during the surgical manipulation with the aim to provide precise surgical access and to evaluate the efficiency of the surgical manipulation in reaching deep collections through the avascular zone; controlled drain provision (Figure 1); precise definition of necroses and assistance in focused necrosectomy. Necrosectomy and drainage were performed through small focused 4-6 cm lumbo-retroperitoneal or subcostal incisions accessing the infected necrotic tissue and/or fluid collections. In patients with several distantly located infected necrosis or fluid collections, necrosectomy and drainage procedures were repeated during the treatment period upon necessity to achieve a full drainage and removal of sequesters. The FON approach eliminated the necessity to use a large laparotomy incision and to open the abdominal cavity below the transverse colon. Small focused subcostal or lumbo-retroperitoneal incisions provided the sinus tract for repeated necrosectomies when it was indicated.
Conventional Open Necrosectomy
CON was performed using the longitudinal midline or bilateral subcostal trans-peritoneal approach, adhering to the semi-opened or closed drainage principles. The laparotomy was executed providing examination of the abdominal cavity, peripancreatic and paracolic spaces and providing proper necrosectomy using blunt finger dissection combined with a suction and drainage. Once the necrosectomy was finished, two large-bore drains for postoperative lavage were inserted, and the abdomen was closed in cases when completeness of necrosectomy was achieved. Semi-open abdominal closure was used in cases when repeated necrosectomies were probable. Close collaboration between the intensive care unit specialists, radiology department specialists and surgeons formed the basis for the multidisciplinary approach.
Approval from the local institutional review board – independent ethics committee of Riga Stradins University was obtained before the study. A special patient informed consent form that differs from the standard surgery consent form was not required. The study protocol complies with the ethical guidelines of the "World Medical Association Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 and amended by the 59th WMA General Assembly, Seoul, South Korea, October 2008.
All variables, complication rate and mortality were analysed and compared between the groups. Continuous data were analysed using the Kolmagorov-Smirnov test. Non-normally distributed continuous data were presented in median values with IQR. Statistical comparison was done with a non-parametric method using the Mann–Whitney U-test. Categorical data were analysed with Pearson’s Chi-square and Fisher’s exact test. The difference was considered statistically significant at the p value level of 0.05, with a 95% confidence interval. Statistical analysis was done using SPSS 20.0 version statistical software (SPSS Inc., Chicago, IL, USA).
Patient Characteristics
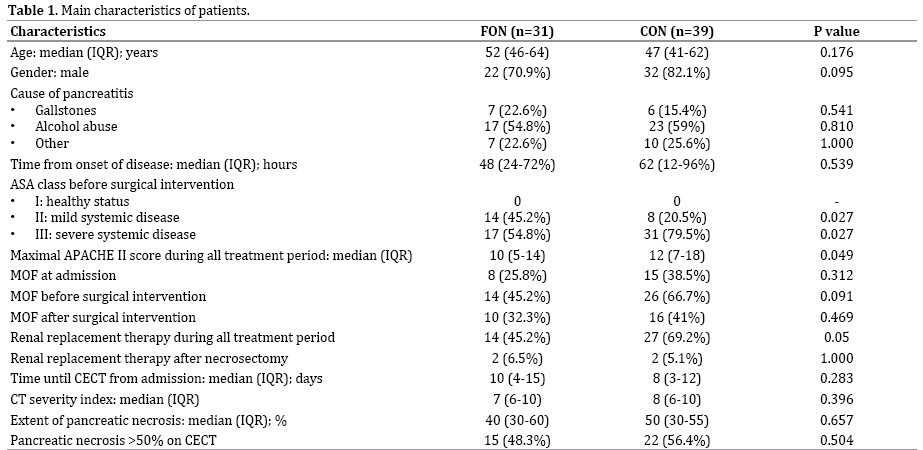
During the 10-year period a total of 151 patients with CECT proved necrotizing pancreatitis were treated in our institution, 65 patients were successfully treated conservatively without an invasive radiologic drainage of ANC and 16 underwent percutaneous drainage of ANC without surgical intervention. A total of 70 patients with acute pancreatitis and sepsis were operated on in our clinic during the period from January 2004 to July 2014; 31 patients in the FON group and 39 patients in the CON group. Although the age, gender, cause of the disease and median admission time after the onset of the disease did not differ between the patients in both groups, prevalence of ASA classification class II comorbid conditions was higher in the FON group, while patients in the CON group were diagnosed with ASA class III comorbidities more often, Table 1. Higher median maximal APACHE II score was observed in the CON group. Organ dysfunction on admission, before and after the surgical intervention was similar in both groups; however, renal replacement therapy during the treatment period was used in the CON group on a more frequent basis. Radiologic evidence of the extent of necrotizing process according to CECT did not differ between the FON and CON patients, Table 1.
Presence of Infection
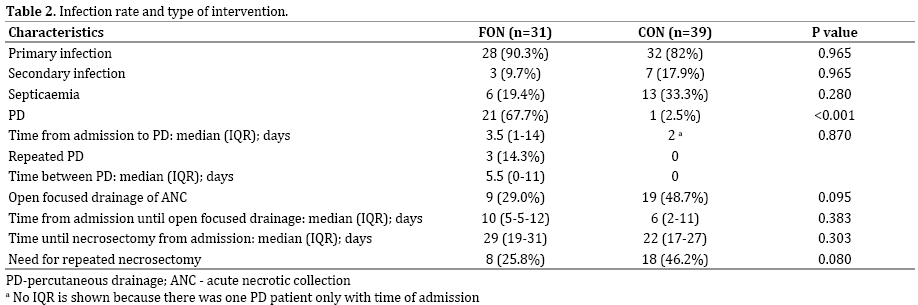
One of the main determinants of the outcome – presence of infection, had the same prevalence in both groups, varying from 82% to 90% in the cases when the infection was classified as primary and from 10% to 18% in the cases when the infection was classified as secondary. Percutaneous drainage was performed significantly more often in the FON group (68% of the cases) than in the CON group (2.5% of the cases), Table 2.
Treatment Strategy
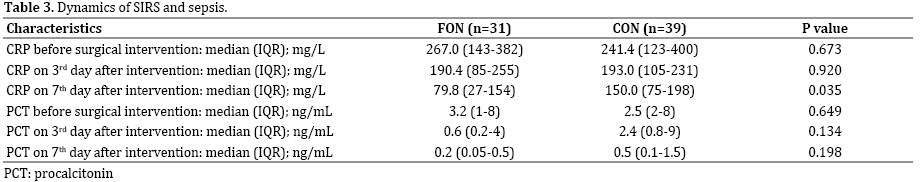
The FON treatment strategy had a positive effect on the clinical course of the disease, the dynamics of the systemic inflammatory response and the possibility to control sepsis. The CRP level decreased in a seven-day period in the majority of the patients from both groups and was significantly lower in the FON group. Procalcitonin (PCT) dynamics did not differ between the two patient groups, Table 3.
Pathogens
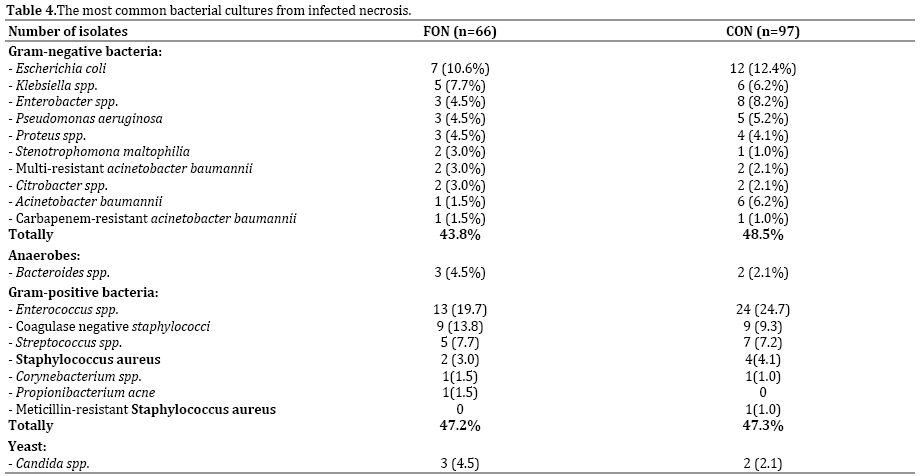
E.coli was isolated in 11% to 12% of the cases and was the most commonly isolated Gram-negative microorganism. Enterococcus spp. was isolated in 20% to 25% of the cases and was the most commonly isolated Gram-positive microorganisms, Table 4.
Surgical Outcome
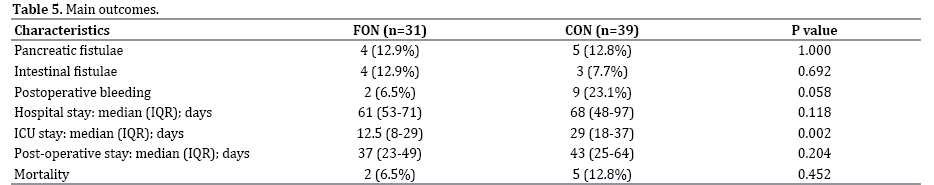
Surgical interventions resulted in an equal incidence of pancreatic fistulae between the two patient groups (13%). A similar prevalence of bowel fistulae and insignificant prevalence of bleeding from the operation site was observed in the CON group. Median hospital length of stay was 61 – 68 days and did not differ between the two patient groups. Median ICU stay was significantly shorter in the FON group while postoperative hospital length of stay did not vary between groups, Table 5. In two cases of biliary pancreatitis patients underwent early cholecystectomy and choledochostomy in the CON group.
Mortality Analysis
A total of 7 patients who were included in the study died during the study period. Two patients from the FON group died, reaching a 6.5% mortality rate, compared to five in the CON group, where mortality reached 12.8%, but it was not a statistically significant difference, Table 5. One of the patients in the FON group had alcohol-induced pancreatitis, the other – biliary pancreatitis. Both patients were admitted 96 hours after the onset of the disease with MOF on admission. The patient with alcohol-induced pancreatitis had 30% pancreonecrosis with localized retroperitoneal involvement, ASA classification class III comorbid conditions and maximal APACHE II score of 31. The patient developed grade II intra-abdominal hypertension, was operated on two times and died after 82 days of treatment due to the progression of MOF and sepsis. The patient with biliary pancreatitis had 100% pancreonecrosis with bilateral retroperitoneal involvement, ASA classification class III comorbid conditions, maximal APACHE II score of 15 and MOF on admission. The patient was operated on two times and died after 22 days of treatment due to massive pulmonary artery thromboembolism. Three patients in the CON group had biliary pancreatitis; one patient developed pancreatitis as a complication after ERCP and one had alcohol-induced pancreatitis. Three out of the five patients were admitted later than 96 hours after the onset of the disease. All patients had MOF on admission and ASA classification class III comorbid conditions, the extent of necrosis varied from 50% to 100%, with ANC collections involving retroperitoneal space in four cases. Three of the five patients underwent more than two surgical interventions. All patients in the CON group died from the progression of MOF and sepsis between 34 to 122 days after admission.
The current consensus regarding the management of necrotizing pancreatitis includes recommendations for the conservative approach in the early phase of the disease and surgical intervention in the late phase when infection complicates the clinical course of the disease. A strong opinion exists regarding the surgical strategy with a recommendation to postpone the intervention and to perform it four weeks after the onset of the disease to ensure formation of WON and a partial or complete liquefaction of necrotic tissue for a better sepsis control after surgical intervention [11-13]. Recommendations how to access the infected necroses have changed over a long period of time and vary from the extended laparotomy approach with retroperitoneal exploration [14, 15] to the alternative, minimally invasive lumbo-retroperitoneal approach without the exploration of the abdominal cavity [16, 17], finally arriving to the minimally invasive treatment concept which is considered to be less traumatic [1, 18, 19]. The so-called step-up approach with percutaneous liquid component drainage has been proposed for a temporary sepsis control as a bridging procedure until definitive necrosectomy is performed [4, 20, 21, 22]. Regardless of whether the approach is endoscopic or laparoscopic, particularly adjusted equipment and a competent specialist team is required for a successful necrosectomy performance and a sufficient number of procedures should be performed while passing the learning curve [23]. The application of the endoscopic trans-gastric approach is limited to WON with a firm attachment to the stomach [24-27]. The efficiency of the endoscopic retroperitoneal approach is limited when peripancreatic necrosis develops in multiple and distant localizations [10, 19, 23]. Extended laparotomy, endoscopic or laparoscopic approaches are used to reach deep retroperitoneal necrosis, however, it is not difficult to reach Morison's pouch or the left retroperitoneal plane between the spleen and the left kidney or the lateral retroperitoneal flanks by open extra-peritoneal [16] or focused lumbotomy. It could be done even more easily by using perioperative ultrasonoscopy, including intraoperative navigation. Adding the perioperative ultrasonography technique to the operating surgeon’s arsenal gives the advantage of making rather small incisions to access deeper tissue layers in retroperitoneum and the peripancreatic area. As a less traumatic technique, FON does not violate the abdominal cavity below the transverse colon, therefore preserving small bowel and peritoneal homeostasis. FON gives the possibility to easily access low-localized necrosis of the retroperitoneal fatty tissue in both flanks. The majority of the patients in the FON group underwent PD before the surgery in accordance with the recently reported surgical step-up approach [4, 28]. Percutaneous drainage can be performed by the Invasive Radiologist; nevertheless, a Surgeon with such ultrasound skills, as in our case, has the advantage of combining the surgical and invasive radiology treatment methods in their daily practice. Until now, the application of intraoperative ultrasonography (IOUS) has not been explored sufficiently in the treatment of pancreatic necrosis. It has been noted in several studies that the main application field of IOUS is hepatobiliary and pancreatic surgery, mainly for the oncological diseases. Recognition of fine anatomical details, tumor extension range, relationship between the blood vessels and determination of the lesion nature, which cannot be detected with other preoperative imaging modalities, are the advantages of IOUS [29, 30]. IOUS is successfully used as an assistant technique in drainage of cysts and abscesses [31, 32]. A quite recent study recommends IOUS application for recognition of pancreatic malignancies and inflammatory changes, including cases with chronic pancreatitis, and distinguishing the extension of necrosis and the probable direction for drainage in acute cases [33]. Another study describes IOUS technique and analyses cases with liver deposits, cystic lesions and abscesses. IOUS is mentioned as a useful modality for detecting cystic lesions in the pancreas; however, it is done through the extended open access laparotomy [34]. Our current study contributes additional experience to the application of IOUS performed by a surgeon. This simple technique using focused 4-6 cm incisions provides the opportunity for an effective necrosectomy and drainage, at the same time avoiding injuries of large blood vessels and the surrounding organs. As a result, a better sepsis control is achieved, therefore reducing persistent organ dysfunction and late mortality, since sepsis is the determining factor of these complications [6, 11, 13, 35-38]. At this point, sufficient data is collected to confirm that the MIT and step-up approaches are the current standards of care for the treatment of necrotizing pancreatitis, but the patient selection and indications for each procedure are not well defined. The same inconsistency can be found in the grading of organ dysfunction and severity of sepsis [8, 12]. In our study organ dysfunction was defined as ≥3 grade dysfunction according to the SOFA score, reflecting the severity of sepsis and quality of the surgical intervention more precisely. Therefore, severity assessment of sepsis could vary in studies where precise grading of organ dysfunction is not mentioned. The overall infection rate, type of isolated microflora, incidence of bacteraemia and severity of sepsis in our cohort was similar to those previously reported in other studies, with a predominance of E.coli in Gram-negative and Staphylococcus in Grampositive isolates [37-44]. The analysis of the PCT level – a sensitive prognostic marker of pancreatic infection [40] demonstrates a strong relation between the severity of sepsis, the effectiveness of surgical treatment and outcome, presenting with a high PCT level in preoperative period, and the evident decrease after a successful intervention. The advantages of combined methods like PD, followed by minimally invasive interventions defined as a step-up approach are evident in cases with infected necrosis [4], however this should be proved by ongoing randomized multicenter clinical trials [44]. The method is effective in a selected group of patients and only part of the patients with infected necrosis could benefit from this approach [1, 13]. In our current study all patients presented with the first or a new episode of ANP (Figure 2). Part of the patients who underwent ultrasound-guided ANC drainage, after establishing a well localized process and attaining normalization of systemic inflammatory response, were discharged from the hospital and treated on an outpatient basis. Rehospitalisation for the definitive surgical treatment was done when the signs of secondary infection appeared. This combined strategy was considered as a single treatment episode including inpatient / outpatient management for carefully assessed patients based on stepup approach principles.
The main disadvantage for all types of MIT approaches is the necessity to repeat the MIT procedures and a relatively high complication rate. The current study demonstrates surgical intervention based on a wider use of ultrasonography as a navigation tool in ultrasoundassisted surgery. The unique aspect of this strategy is the application of the ultrasonography method used by the Surgeon who specializes in the field of ultrasonography and may use the full potential of this method – starting from a percutaneous ANC drainage, control of the complete drainage and intraoperative ultrasound navigation through small 4-6 cm incisions in the abdominal wall to find the right anatomical plane and localize the fluid collections or necrosis, and following with necrosectomy and drainage. Our strategy allows the use of the sinus tract created during the first intervention for repeated debridement in the ICU, similarly to what has been recently reported [45]. The important experience is the combination of the stepup approach and ultrasound-assisted surgery to provide open necrosectomy but with minimal access elements or FON. This strategy gives the opportunity to provide surgical treatment to patients with wide peripancreatic and bilateral retroperitoneal involvement as well [10]. Simple criteria give the possibility to select the patient for FON. These include: previous PD of ANC, localized process confirmed by CECT and transabdominal ultrasound before intervention in patients with evidence of the progression of sepsis and organ dysfunction, despite conservative treatment. The use of these criteria is supported by a number of other studies [4, 19, 28, 46]. We did not use fine needle aspiration for bacterial culture assessment, which has been recently recognized as an inapplicable diagnostic tool [4, 28, 41]. Finally, the main outcomes of our study comply with the study results reported by different authors. The postoperative complication rate [24, 47-49] and mortality is similar to other reports concerning the MIT approaches [19, 24, 25, 50] and the conventional approach [15, 36, 48]. The rate of preoperative infection which is the main determinant of the late mortality is in the same range as reported by a number of other studies. Nevertheless, a higher prevalence of bacteraemia was observed in patients who underwent conventional surgery, probably indicating poorly localized infected necrosis (Figure 3).
Prevalence of ASA class III comorbid conditions in the CON group could be linked to a higher rate of bacteraemia. The analysis of the patient mortality revealed that the late hospitalization might be associated with the poor response to conservative treatment. Despite these facts, postoperative mortality in both groups did not exceed 13% and the main outcomes are compatible with the results reported by other authors. The weak point of our study is the lack of randomization due to the nature of the intervention and the slight difference in the preoperative condition of the patients in the FON and the CON group (Figure 4). The preoperative status of inflammatory response, however, was not different, analysing levels of CRP and PCT, and incidence of organ failure and postoperative complication rate was similar. Due to the insufficient number of patients at this point of the study we do not have strong statistically significant evidence that mortality is significantly reduced using the FON approach. The aim of study was to demonstrate the feasibility, safety and non-inferiority of the FON approach, and the results of the study confirm this statement.
Individual assessment of the comorbid condition severity, presence of organ failure, localization of ANC and early recognition of the infection are crucial steps in the management of infected pancreatic necrosis that complies with the currently evolved step-up approach. A broader implementation of the preoperative and intraoperative ultrasonography could be an additional improvement of the open surgical approach, when performance of the minimally invasive procedure is not feasible.
Authors declare to have no conflict of interest.