Case Report - (2022) Volume 8, Issue 6
Unique Piercing Site Drug Reaction
Margaret Kaszycki* and
Andreas Bub
Department of Internal Medicine, Stamford Hospital, Stamford, USA
*Correspondence:
Margaret Kaszycki, Department of Internal Medicine, Stamford Hospital, Stamford,
USA,
Email:
Received: 24-Mar-2022, Manuscript No. IPCPDR-22-12768;
Editor assigned: 26-Mar-2022, Pre QC No. IPCPDR-22-12768(PQ);
Reviewed: 11-Apr-2022, QC No. IPCPDR-22-12768;
Revised: 10-Oct-2022, Manuscript No. IPCPDR-22-12768(R);
Published:
17-Oct-2022, DOI: 10.36648/2472-0143.8.6.27
Abstract
Hyperhidrosis piercings of the body and ears is a popular practice amongst the US adolescent population. Localized infections and reactions are common, including allergic contact dermatitis, bleeding, scarring, and keloid formation. Piercing the skin serve as a site of trauma, thus predisposing patients to these complications. Enhancement of systemic reactions to localized regions is an uncommon phenomenon but has been reported in several cases such as chemotherapy-induced radiation dermatitis. We present a case of lamotrigine induced erythema multiform major in a 17 years old female, whose diagnosis was delayed due to initial presentation mimicking disseminated herpes simplex virus, Bechet’s, and an autoimmune condition due to unknown steroid use. In addition, the patient had enhancement of erythema and pain around multiple facial piercings. Although the cause of enhancement at the piercing sites is unclear, the bodily piercings may serve as an example of an enhanced immunologic reaction at Immuno Compromised Districts (ICD). ICDs are areas of skin that have experienced prior trauma resulting in chronic skin changes resulting in enhanced or weakened immunologic reactions. This case highlights a unique localized complication of body piercings as well as several important learning points including the complications of piercings, importance of medication reconciliations, atypical presentations of diseases secondary to patients concealing relevant medical information, the benefit of broad differentials, and overlapping disease presentations resulting in delay of correct diagnoses.
Keywords
Hyperhidrosis piercings; Erythema Multiform (EM); Leukocytosis neutrophil;
Predominance; Immuno compromised districts
Introduction
Piercings of the body and ears is a popular practice amongst
the US population localized infections and reactions are
common, including allergic contact dermatitis, bleeding,
scarring, and keloid formation. Piercing the skin serve as a site
of trauma, thus predisposing patients to these complications.
Depending on the piercing site and the reaction, treatments
vary [1,2]. Enhancement of systemic reactions to localized
regions is an uncommon phenomenon but has been reported in several cases such as chemotherapy induced radiation
dermatitis [3]. In this article, we report a patient with
Erythema Multiform (EM) major with enhancement of
erythema and pain around multiple bodily piercing sites.
Case Presentation
A 17 years old female was admitted to the gynecological service for what was assumed to be an initial presentation of oral and genital manifestations of Herpes Simplex Virus (HSV).
At the time of initial presentation, the patient had 6 small (1-3 mm) oral ulcerations and a single ulcer on the labia majora (3 mm). Medical history was significant for obsessive compulsive disorder and bipolar disorder and patient started lamotrigine 16 days prior. Over the next three days, ulcerations increased in number and size. The patient also began to develop conjunctivitis with watery discharge. Initial labs were most notable for: leukocytosis with a neutrophil predominance, elevated ESR and CRP, and ANA positivity with a titer of 1:640 in a homogenous pattern. Given this constellation of symptoms, physical exam findings, and laboratory data, the initial differential diagnosis included disseminated HSV vs. Behcet’s vs. autoimmune disease vs. drug reaction. Follow up studies were ordered, and lamotrigine was discontinued. Unbeknownst to the team, the patient had been taking oral prednisone for the past 5 days. Prednisone was tapered and discontinued for concerns for infectious etiology.
Results
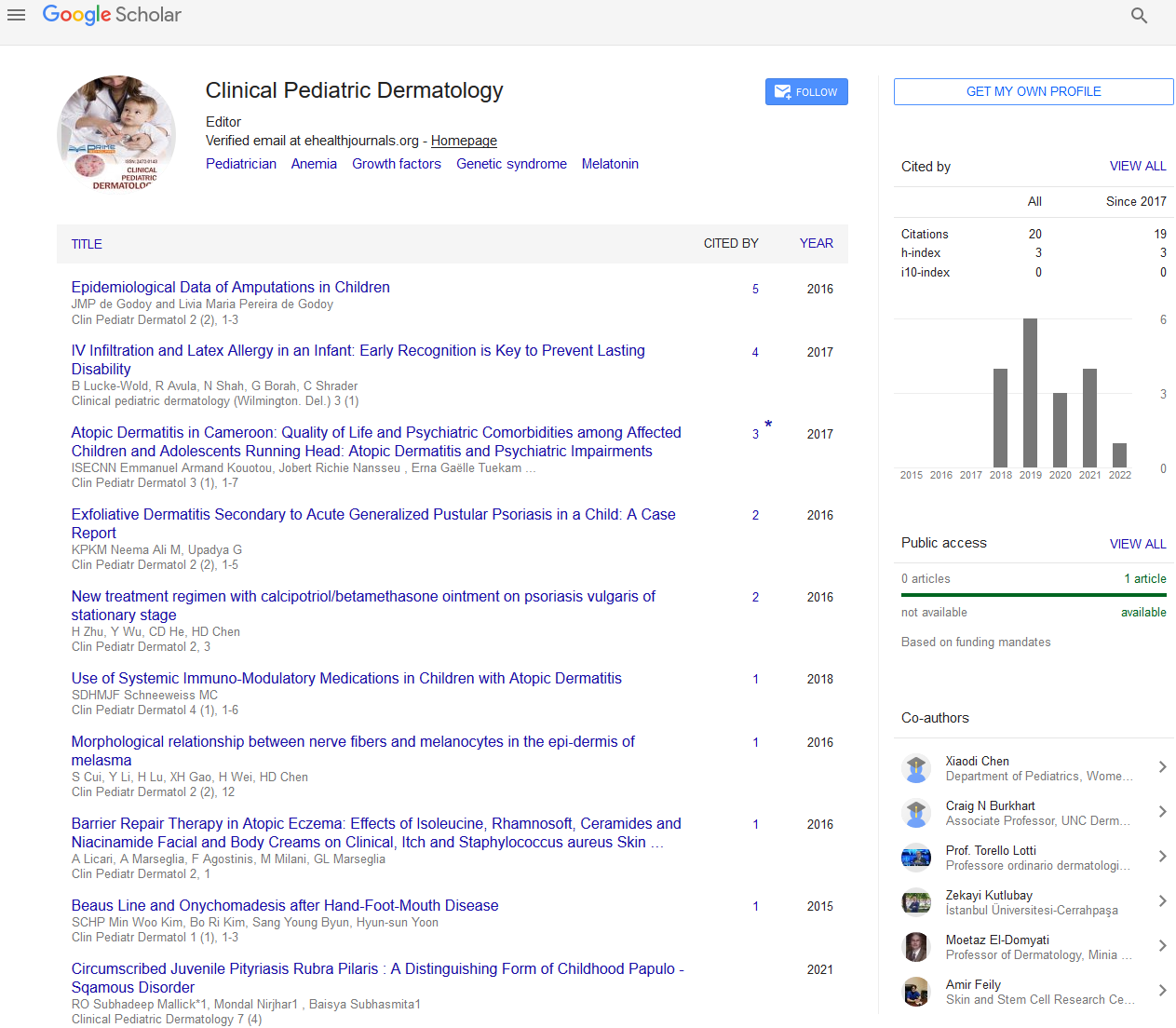
The following day the patient developed an acute worsening
of cutaneous symptoms. The patient's oral and genital
ulcerations became confluent. The oral mucosa now
appeared raw with cheilitis and dried blood. The patient also
developed new painful cutaneous manifestations on their
face with focal areas of erythema around sites of bodily
piercings as shown in Figure 1 including the umbilicus
(not pictured). Follow up laboratory results demonstrated an
acute eosinophilia, worsening leukocytosis, HSV PCR
returned negative, along with negative rheumatologic
makers and normal complement levels. Patient was started
on high dose IV steroids and the differential was narrowed to
autoimmune disease vs. drug reaction. Skin biopsy
demonstrated interface dermatitis with necrotic
keratinocytes and melanin pigment incontinence in the
superficial dermis.
No eosinophils were noted in the biopsy. The final diagnosis
of lamotrigine induced erythema multiform major was
made. The piercings were removed, and the patient was
treated with IV steroids, moxifloxacin eye drops to prevent
ocular infection, mupirocin ointment to apply on the oral/
vaginal mucosa to prevent infection, and an intravaginal
steroid ointment to prevent the development of adhesions
as the labial/vaginal ulcerations healed. The patient had
a complete recovery including piercing sites, and was
discharged within a week.

Figure 1: Erythema multiforme major with periocular
erythema, circular erythematous patches on the cheek and
nose, targetoid lesions on the lower check and forehead.
enhanced erythema surrounding nose piercings.
Discussion
The patient’s initial presentation resulted in mimicry of HSV
and Behest’s delaying the diagnosis of EM major. However,
the unique observation in this case is the enhancement of
erythema at sites of bodily piercings. Although the cause is
unclear, the bodily piercings may serve as an example of an
enhanced immunologic reaction at Immuno Compromised
Districts (ICD). ICDs are areas of skin that have experienced
prior trauma resulting in chronic skin changes resulting in
enhanced or weakened immunologic reactions [4,5].
Erythema multiform is an immune mediated disorder,
therefore it is possible an immunological reaction was
exaggerated at the sites of bodily piercings [6].
Conclusion
Therefore, rococo’s theory of ICD can provide an explanation
as to why enhancement of was observed around the patients’
sites of bodily piercings. This case highlights a unique localized
complication of body piercings in a pediatric patient with
several important learning points including the importance of
piercings, medication reconciliations, and atypical
presentations of diseases secondary to patients concealing
relevant medical information, the benefit of broad
differentials, and overlapping disease presentations resulting
in delay of correct diagnosis.
Conflict of Interest
Authors declare no conflicts of interest.
References
- Holbrook J, Minocha J, Laumann A. Body piercing. Am J Clin Dermatol. 13:1–17
[Google Scholar][Indexed]
- Meltzer DI (2005) Complications of body piercing. American family physician. 72: 2029–2034.
[Google Scholar][Indexed]
- Kaszycki MA, Leventhal J (2021) Review of immune checkpoint inhibitors and radiotherapy related skin toxicities. J Dermatol and Skin Sci. 3:10-19
[Google Scholar][Indexed]
- Piccolo V, Baroni A, Russo T, Schwartz RA (2015) Ruocco's immunocompromised cutaneous district. Int J Dermatol. 55:135-141.
[Crossref][Google Scholar][Indexed]
- Ruocco V, Ruocco E, Brunetti G (2013) Recall phenomena: another facet of the immunocompromised district. Int J Dermatol. 52(2):252-253.
[Crossref][Google Scholar][Indexed]
- Huff JC, Weston WL, Tonnesen MG (1983) Erythema multiform: a critical review of characteristics, diagnostic criteria, and causes. J Am Acad Dermatol. 8:763–775.
[Crossref] [Indexed]
Citation: Kaszycki M, Bub A (2022) Unique Piercing Site Drug Reaction. Clin Pediatr Dermatol. 8:27
Copyright: © 2022 Kaszycki M, et al. This is an open-access article distributed under the terms of the Creative Commons
Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author
and source are credited.