- (2014) Volume 15, Issue 2
Eric Marks1, Muhammad Wasif Saif2, Yuxia Jia1
1Penn State Hershey Medical Center, Cancer Institute. Hershey, PA, USA.
2Hematology and Oncology, Tufts University School of Medicine. Boston, MA, USA
Pancreatic adenocarcinoma is the 10th most common malignancy in the United States but is responsible for the 4th mostcancer related deaths. This disease can only be potentially cured through early discovery and complete surgical resection.Unfortunately, nearly half of patients have metastatic spread at presentation. Combination chemotherapy with FOLFIRINOXor gemcitabine with nab-paclitaxel can prolong survival in selected patients, but at the cost of significant toxicity. In the 2014ASCO Gastrointestinal Cancers Symposium, several studies were presented that focus on the management of metastaticpancreatic cancer. A phase II trial by Le et al. (Abstract #177) found that the addition of CRS-207, a strain of Listeria modifiedto stimulate an anti-tumor immune response, improves survival in patients being treated with GVAX. Goldstein et al.(Abstract #178) presented a post-hoc survival analysis for the phase III MPACT trial that shows the addition of nab-paclitaxelto gemcitabine produces a persistent survival benefit. Ramanathan et al. (Abstract #224) demonstrated that, withappropriate dose adjustments and delays, induction nab-paclitaxel and gemcitabine followed by mFOLFIRINOX consolidationis a feasible treatment option for metastatic pancreatic cancer. Despite these advances, it is imperative that we continue towork towards developing additional treatment options that are better tolerated and further prolong survival for thesepatients. This highlight article focuses on the first-line therapy of metastatic pancreatic adenocarcinoma.
Adenocarcinoma; Drug Therapy; Immunotherapy; Neoplasm Metastasis; Pancreatic Neoplasms
ECOG: Eastern Cooperative Oncology Group; FOLFIRI: irinotecan, 5-fluorouracil and leucovorin; FOLFIRINOX: leucovorin, 5-FU, irinotecan, oxaliplatin; FOLFOX: 5-flouorouracil, leucovorin and oxaliplatin; mFOLFIRINOX: modified FOLFIRINOX; SPARC: secreted protein rich in cysteine
Pancreatic cancer is the 10th most common new cancer diagnosis in the United States, with approximately 45,220 new cases each year [1]. Pancreatic adenocarcinoma is a very lethal disease and is responsible for the 4th largest number of cancer related deaths in the country. This is due, in part, to its tendency to remain asymptomatic until the tumor is fairly advanced, limiting the likelihood of early diagnosis. At the time of initial presentation, roughly half of patients have distant metastatic spread [2]. The prognosis for these patients is poor, with overall survival being measured in months.
When determining treatment options for patients with metastatic pancreatic adenocarcinoma, first consideration must be given to the performance status. Patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0-1 are candidates to receive first-line combination chemotherapy. The most recent National Comprehensive Cancer Network (NCCN) guidelines recommend the combination of leucovorin, 5-FU, irinotecan, oxaliplatin (FOLFIRINOX) or gemcitabine in combination with either nabpaclitaxel, erlotinib, capecitabine or cisplatin [3]. As FOLFIRINOX is more toxic than gemcitabine based combination therapy, it is generally given only to those patients with the highest pre-treatment performance status of 0-1 and with no liver dysfunction. Other, less frequently used regimens, include combination of fixed dose rate gemcitabine, docetaxel, and capecitabine (GTX) or combination of capecitabine and oxaliplatin (Cape-Ox). Unfortunately, even the most effective of these regimens confer only a modest survival benefit, typically 6-10 months [4]. As this comes at the cost of adding significant toxicity, some patients opt to instead receive treatment with a single agent, typically gemcitabine, capecitabine, or continuous 5-FU infusion. These same single agent treatment options are offered to patients whose ECOG performance status is 2 or greater. All of these patients are also provided best supportive care, as the goals of their treatment are prolonged survival and palliation rather than cure.
In recent years, much effort has been put into further understanding and improving upon the treatment options available for this devastating disease. Survival data from pre-existing trials are being updated, and researchers are examining the utility of administering multiple first line regimens in an induction-consolidation sequence. Also, GVAX, an investigational immunostimulatory therapeutic derived from allogenic pancreatic cancer cells is being explored as a new treatment option [5]. This highlight article will discuss three abstracts presented at the 2014 American Society of Clinical Oncology (ASCO) Gastrointestinal Symposium that focus on the first-line therapy of metastatic pancreatic adenocarcinoma.
GVAX Pancreas and CRS-207 Immunotherapy Versus GVAX Alone (Abstract #177) [6]
Le et al. investigated the effect of administering CRS-207 with GVAX on overall survival in metastatic pancreatic cancer. GVAX consists of irradiated pancreatic cancer cells that have modified to elude granulocyte-macrophage colonystimulating factor (GM-CSF) and produce an antitumor immune response. Immunogenicity is further enhanced with low dose cyclophosphamide, which inhibits regulatory T-cells. CRS-207 contains liveattenuated Listeria monocytogenes that is modified to produce mesothelin, a protein that is overexpressed on pancreatic cancer cells. When given in conjunction with GVAX and cyclophosphamide, CRS-207 was shown to be synergistic in mouse models and phase I studies in humans subjects. They randomly assigned 90 patients with metastatic pancreatic adenocarcinoma and ECOG performance status 0-1 to receive either 2 doses of GVAX/ cyclophosphamide followed by 4 doses of CRS-207, or 6 doses of GVAX/cyclophosphamide. Survival was much improved in the arm receiving CRS-207, with median overall survival of 6.1 months compared with 3.9 months in the GVAX/ cyclophosphamide only arm. This disparity was widened to 9.7 months versus 4.6 months when comparing only patients who received at least 3 doses of treatment. Toxicity from this therapy was minimal in both arms.
Nab-Paclitaxel Plus Gemcitabine Versus Gemcitabine Alone (Abstract #178) [7]
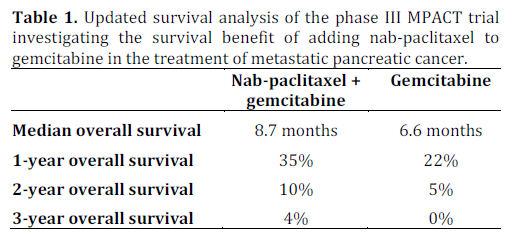
Goldstein et al. provided an updated survival analysis for the phase III MPACT trial, which previously found that the addition of nab-paclitaxel to gemcitabine treatment conferred a survival benefit (6.7 months vs. 8.5 months) to patients with metastatic pancreatic adenocarcinoma. This trial followed 861 patients who were randomly assigned to the two treatment arms. At the time of this update, 88% of patients in the nab-paclitaxel plus gemcitabine arm had died, compared to 92% in the gemcitabine-only arm. The estimated 1-, 2-, and 3- year overall survival rates for each treatment group are shown in Table 1, further demonstrating the persistent benefit of adding nab-paclitaxel.
Induction Gemcitabine and Nab-Paclitaxel Followed by mFOLFIRINOX Consolidation (Abstract #224) [8]
Ramanathan et al. studied the tolerability of sequential treatment with induction nab-paclitaxel plus gemcitabine followed by consolidation with modified FOLFIRINOX (mFOLFIRINOX) or a similar regimen. This phase II trial recruited 31 patients with untreated metastatic pancreatic cancer and ECOG performance status of 0-1. All patients received induction therapy with nab-paclitaxel and gemcitabine until either 6 cycles were complete or their disease progressed. Patients then received consolidation therapy with either FOLFIRINOX (22 patients), FOLFIRI (4 patients), or FOLFOX (1 patient). Significant (grade 3 or greater) treatmentrelated toxicity was common, with patients suffering neutropenia (39%), fatigue (32%), anemia (32%), thrombocytopenia (16%), thromboembolic events (3%), peripheral neuropathy (16%), leukopenia (16%), nausea (3%), vomiting (3%), diarrhea (7%), and neutropenic fever (3%). During induction alone, patients required 14 dose reductions and 4 dose delays. One-year overall survival is projected to be 50-60%. The authors conclude that this induction-consolidation strategy is plausible in selected patients and with careful attention to dose adjustments for managing cumulative side effects.
Pancreatic adenocarcinoma is an exceedingly lethal malignancy that can only be potentially cured via complete surgical resection. Unfortunately, approximately 50% of patients have metastatic disease at the time of initial presentation and therefore do not have a chance of cure. Although several chemotherapy regimens have been found to prolong survival in these patients, they are often associated with significant toxicity. Patients with poor performance status are offered treatment with a single chemotherapeutic agent, typically gemcitabine or capecitabine. Those with better performance status are candidates for combination chemotherapy, most commonly FOLFIRINOX or gemcitabine plus nab-paclitaxel.
A summary of the studies presented at the 2014 ASCO Gastrointestinal Cancers Symposium is shown in Table 2.
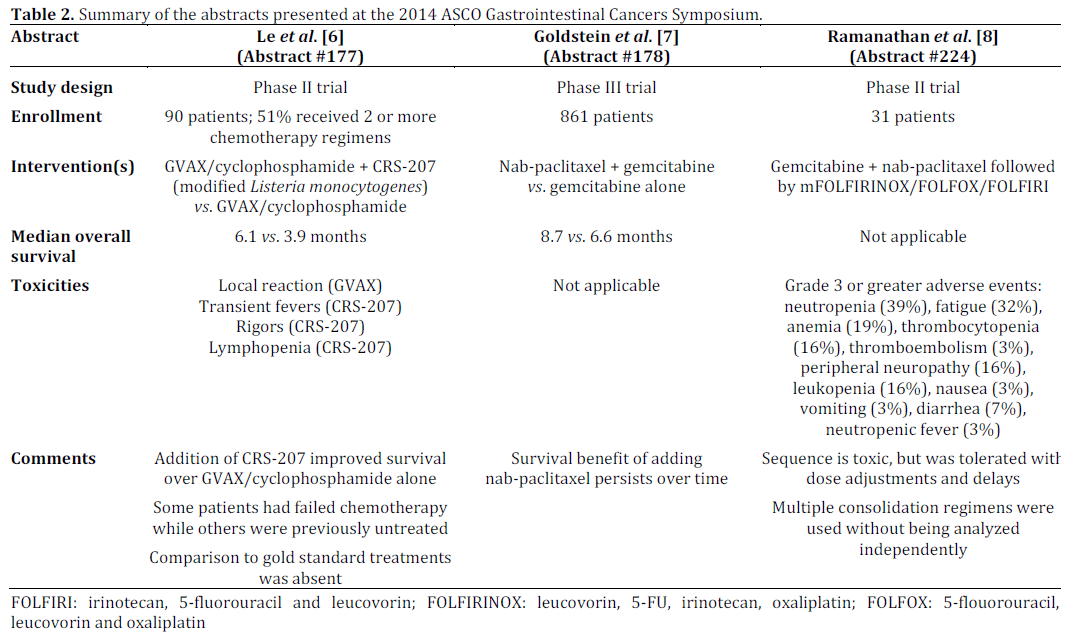
GVAX is an experimental therapeutic that contains highly immunogenic but unviable pancreatic cancer cells. Research by Le et al. (Abstract #177) [6] demonstrated a synergistic effect between GVAX and CRS-207, a genetically modified strain of Listeria that stimulates a strong anti-tumor immune response. Patients who received both agents survived 6.1 months, compared with 3.9 months for those who received only GVAX. Though promising, these findings were observed in a heterogeneous sample of patients, some of whom had failed multiple chemotherapy regimens while others had been previously untreated. Also, the absence of a “gold standard” treatment arm makes it difficult to assess the true extent of survival benefit conferred by treatment with these agents.
Goldstein et al. (Abstract #178) [7] updated survival data for the multi-center MPACT trial that investigated the addition of nab-paclitaxel to gemcitabine in treating metastatic pancreatic cancer. The updated analysis found that patients who received both drugs exhibited a significant survival benefit that persisted over time. At 3 years, the researchers project that no patients who received gemcitabine monotherapy will remain alive compared to 4% of patients treated with both nab-paclitaxel and gemcitabine.
A study by Ramanathan et al. (Abstract #224) [8] investigated the feasibility of treating metastatic pancreatic cancer with induction nab-paclitaxel and gemcitabine followed by mFOLFIRINOX consolidation. Despite considerable toxicity (nearly half of patients suffered a grade 3 or greater adverse event) and dose reductions, patients did tolerate these treatments. Of note, some patients received the less toxic FOLFIRI or FOLFOX regimens as consolidation instead of mFOLFIRINOX. As a result, the treatment sequence proposed by these authors may be slightly less tolerable than this study indicates.
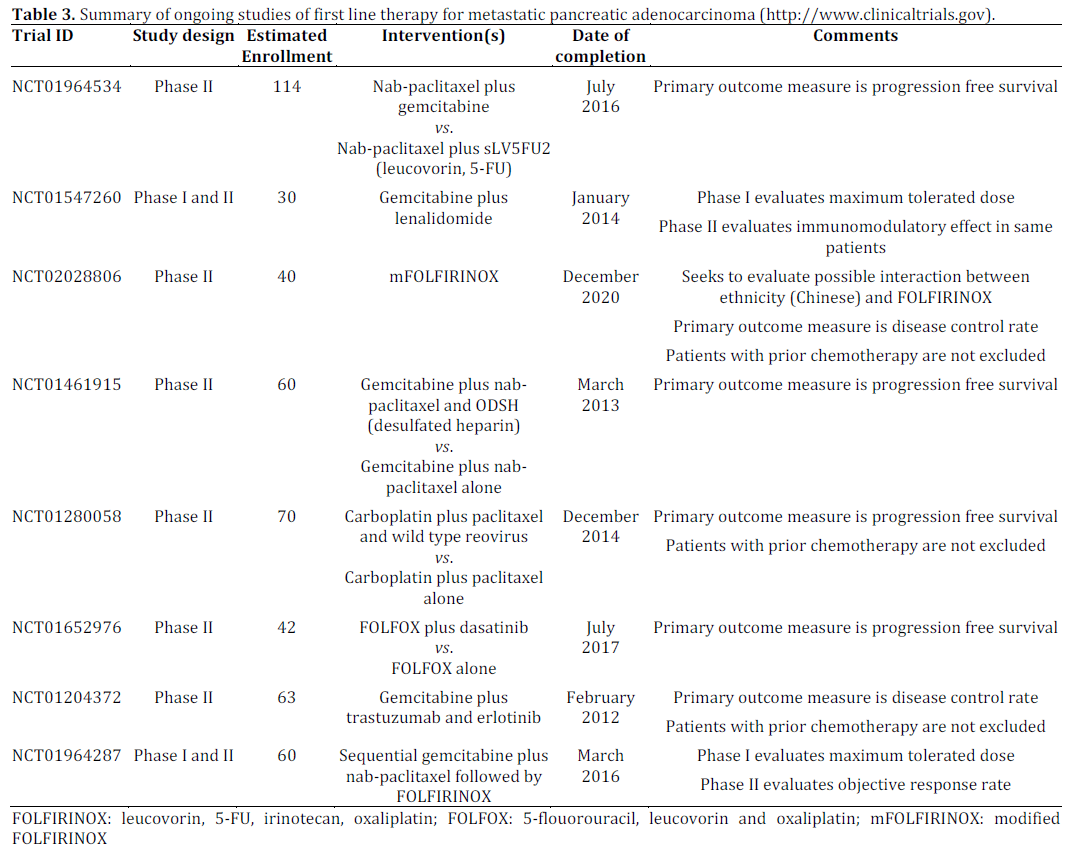
Despite these advances, it is important that we continue to work towards developing additional treatment options that are better tolerable and further prolong survival for patients. A summary of ongoing clinical trials investigating the first-line treatment of metastatic pancreatic adenocarcinoma is listed in Table 3. Targeting tumor stroma is emerging as a strategic approach for pancreatic cancer treatment. For instance, secreted protein rich in cysteine (SPARC) is overexpressed in pancreatic tumor stoma fibroblast and downregulated in tumor cells. This characteristic is associated with poor clinical outcome [9]. Several therapeutic strategies to deplete stromal tissue have been developed. A study (NCT01442974) on assessment of stromal response to nab-paclitaxel in combination with gemcitabine in patients with SPARC positive pancreatic cancer is ongoing.
The authors have no potential conflicts of interest