Genel H1, Hubinont C2, Baldin P3, Amant F4-6 and Mhallem M1*
1Department of Obstetrics, Cliniques Universitaires, Saint-Luc, Belgium
2Department of Urology, Cliniques Universitaires, Saint-Luc, Belgium
3Departement of Pathology, Cliniques Universitaires, Saint-Luc, Belgium
4Department of Oncology, Kuleuven, Belgium
5Center for Gynecological Oncology Amsterdam (CGOA), Anton Van Leeuwenhoek Cancer Institute, The Netherlands
6Center for Gynecological Oncology Amsterdam (CGOA), Amsterdam University, Medical Centers, The Netherlands
- Corresponding Author:
- Mhallem M
Department of Obstetrics
Cliniques Universitaires Saint-Luc, Belgium
Tel: 0032472394326
E-mail: mina.mhallem@uclouvain.be
Received Date: April 16, 2020; Accepted Date: June 01, 2020; Published Date: June 05, 2020
Citation: Genel H, Hubinont C, Baldin P, Amant F, Mhallem M (2020) Urachal Cancer in Pregnancy: A Case Report and Review of Literature. Gynecol Obstet Case Rep Vol.6 No.2:17 doi:10.36648/2471-8165.6.2.97
Keywords
Urachal cancer; Ultrasound; Pregnancy
Introduction
Urachal cancer is a form of cancer that arises in a structure called
the urachus. The urachus is a canal that exists when the fetus is
developing before birth. This canal runs from the bladder of the
fetus to the belly button (umbilicus). It drains the urinary bladder
of the fetus. Between the fourth and fifth month of pregnancy,
this canal breaks down (degenerates) into a fibrous band of
tissue called a ligament. A urachal cyst is a collection of tissue and
fluid between the bladder and the belly button (umbilicus). The
cyst forms in the remnants of the urachus, a structure normally
present in a fetus that usually closes up before birth. In some
infants, the closure doesn't occur. If this happens, a urachal
abnormality (such as a cyst or sinus) remains. Urachal cancer
will often extend into surrounding structures like the bladder,
and can potentially spread (metastasize) to other areas of the
body. The exact, underlying cause of urachal cancer is not fully
understood. Surgery is the most common treatment option.
Case Report
A 42-year-old, gravida 3 para 2, pregnant patient was referred at
38 weeks’ gestational age to our tertiary center for suspicion of
abnormal insertion of the placenta (PAS).
The previous medical history is marked by a vesico-ureteral reflux
surgery at age of 9 years The patient is an active smoker and
episodic cannabis user. The family history is marked by several
cancers. Her mother recently died of pancreatic cancer, her
father had a bladder cancer and her brother had a lung cancer.
In 2006, the patient delivered vaginally at 38 weeks. In 2011, a caesarean was performed for a breech position baby. As it was
an unplanned pregnancy, she had no medical follow-up until the
last trimester.
The patient was referred at 38 weeks for suspicion of placenta
accreta spectrum (PAS). She presented a macroscopic haematuria
associated with a urinary tract infection treated by antibiotics.
The obstetrical ultrasound showed at the level of the cesarean
scar a mass bulging inside the bladder.
We carried out a fetal monitoring showing a normal rhythm.
There was no significant uterine activity. The urinary test t returned positive and the culture showed an E. coli infection
resistant to ampicillin for which cefuroxime was prescribed.
Obstetrical level III ultrasound showed a cephalic foetus with
normal growth around the 50 percentile. The amniotic fluid
index was normal with an index of 15. The placenta was anterior, marginal type II. The placenta-bladder interface was well
visualized. We did not find bridging vessels in the myometrium.
No other signs of PAS such as placenta lacuna were observed [1].
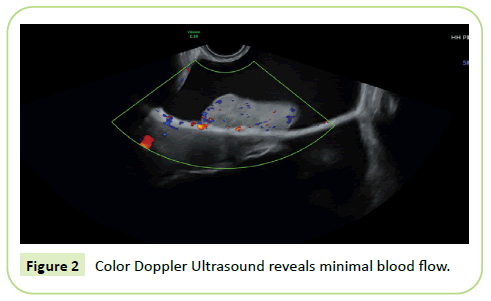
Ultrasonographically, a 9 cm mass in the bladder not connected
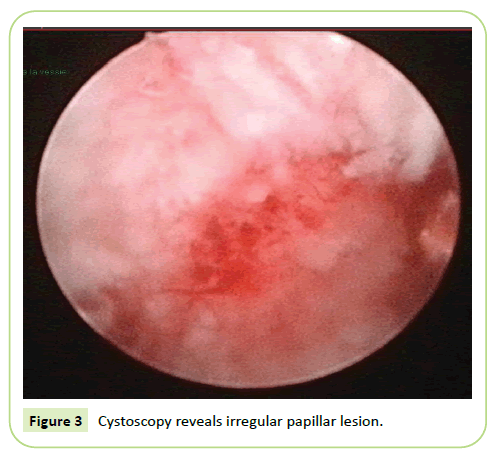
with the placenta was observed (Figures 1 and 2). A cystoscopy
revealed a suspicious mass developed on the anterior wall and
the dome of the bladder (Figure 3). No malignant cells were
found in the urine cytology. A magnetic resonance imaging (MRI)
was impossible due to claustrophobia.
Figure 1: Gray-scale ultrasound, suspicion bladder tumor.
Figure 2: Color Doppler Ultrasound reveals minimal blood flow.
Figure 3: Cystoscopy reveals irregular papillar lesion.
Vaginal examination showed a closed cervix with a mass palpable
in the retropubic wall. Because an undertermined large mass
behind the anterior wall of the vagina we choose to perform
a caesarean section. The patient delivered of a baby girl 2970
grams with an Apgar score of 8 at 5 minutes and 9 at 10 minutes.
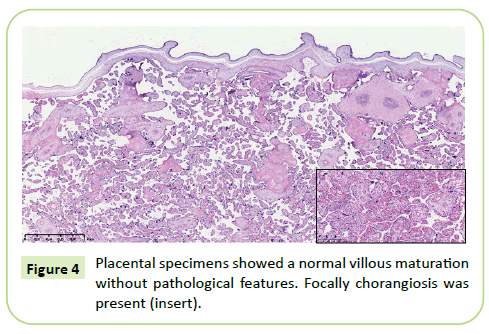
The cesarean section was uncomplicated. The placenta delivery
was uneventful and no sign of placenta accreta spectrum was
noted. The bladder digital exam confirmed the presence of a
hard intra-vesical mass. The posterior wall of the bladder was
normal. The pathological analysis of the placenta confirmed the
absence of PAS (Figure 4).
Figure 4: Placental specimens showed a normal villous maturation without pathological features. Focally chorangiosis was present (insert).
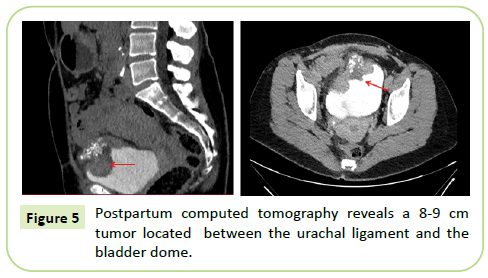
The postpartum computed tomography showed a neoplasic
thickening on the antero-superior side of the bladder in continuity
with the urachus (Figure 5). The first hypothesis was an urachal
tumor without expansion.
Figure 5: Postpartum computed tomography reveals a 8-9 cm tumor located between the urachal ligament and the bladder dome.
A transurethral resection of bladder tumor (TURBT) was Figure 2 Color Doppler Ultrasound reveals minimal blood flow. performed 3 weeks after the cesarean. The operation was incomplete. The samples from trans-urethral resection were
submitted for pathological evaluation. The fragments were
infiltrated by a neoplastic malignant proliferation composed of
glandular structures and signet-ring cells surrounded by mucin.
These cells infiltrated the detrusor muscle. Neoplastic cells
were diffusely positively stained for CK20, focally for STATB2
and negatives for the following stainings: GATA3, PAX8, betacatenine,
Cytokeratin 7, estrogen receptors and progesteron
receptors. The diagnosis of mucinous carcinoma with signet ring
differentiation (most) likely of urachal origin was made.
Considering the young age of the patient, the partial and the
radical cystectomy were discussed. The patient preferred a
radical treatment. A radical cystectomy followed by enteroplasty
and lymphadenectomy was performed to complete the surgery.
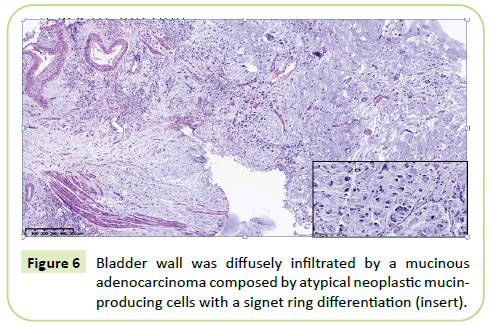
The pathological findings confirmed the urachal origin of lesion
(Figure 6). Lymph node analysis was negative.
Figure 6: Bladder wall was diffusely infiltrated by a mucinous adenocarcinoma composed by atypical neoplastic mucinproducing cells with a signet ring differentiation (insert).
Discussion
Cancer diagnosis during pregnancy is very rare condition but is
increasing over the years [2,3]. The most frequently encountered
cancers are breast and haematological cancers [4-6]. The
incidence for bladder cancer during pregnancy is estimated to 1.4
to 2.5% of all cancers during pregnancy [7]. The urachal cancer
represents 0.5% of all vesical cancers. The physiopathology of
this cancer is poorly understood but is developed from a remnant
structure, the urachus, connecting the embryological allantois
and the dome of the bladder existing during the fetal life. It is
mostly aggressive and discovered at advanced stages [8].
Only some cases reports of urachal cancers during pregnancy are
described in the literature. Investigations are recommended in
order to distinguish this tumor from a leiomyoma, endometriosis
or urachal diverticulum and from other types of bladder cancers
[9-15]. Frequent clinical signs are microscopic or macroscopic hematuria, recurrent urinary tract infections, dysuria, postcoital
bleeding and abdominal or back pain. These complaints
are frequent in normal pregnant patients and then can delay the
cancer diagnosis.
Abdominal ultrasound, cystoscopy and magnetic resonance
imaging are indicated for suspicious masses. These investigations
could be performed during the pregnancy in order to avoid
diagnostic delay and improve the prognosis.
The main predictor factor is the TNM classification initially
described by Sheldon and adapted by Molina in 2007-8 [16].
Multidisciplinary management is necessary to optimize the
maternal prognosis. For not pregnant patients, surgery,
chemotherapy and radiotherapy are proposed depending on the
tumor stage. Partial and/or radical cystectomy, umbilicotomy
and urachal resection are indicated for stage I and II stage with
good survival. Systemic therapy and irradiation are proposed
for advanced stages with bad prognosis [8]. Chemotherapies
as fluoropyrimidine, taxane, cisplatine and gemcitabine are
mostly proposed to treat metastatic cancers [17]. Hyperthermic
intraperitoneal chemotherapy associated to cytoreductive
surgery is also described for metastatic lesion of urachal cancers
[18]. Systemic therapy with monoclonal antibodies directed to
epidermal growth factor receptors may be used to treat urachal
cancers [19].
Urachal treatments during pregnancy are already described
as surgery and chemotherapy. During the first trimester of
pregnancy, termination of pregnancy is discussed with the
parents and can be indicated when the prognosis is poor.
Surgery can be performed during the three trimesters. The
urachal cancer has a high recurrence rate and particularly in case
of positive lymph nodes and surgical margins. Chemotherapy
may be proposed during the second and third trimester of
pregnancy. Intraperitoneal therapy and systemic treatment are
not authorized during pregnancy.
Conclusion
In conclusion, multidisciplinary management is highly
recommended in case of suspicious bladder cancer during
pregnancy. Cystoscopy, abdominal ultrasound and magnetic
resonance imaging are useful tools for evaluation of the tumor
during pregnancy. The treatment is adapted to each case given the
paucity of case reports published in the literature. Participation
in international registration as International Network of Cancer,
Infertility and Pregnancy (INCIP) is needed to collect more data
to draw conclusions and to standardize the pregnant patient
management.
References
- Jauniaux E, Collins SL, Jurkovic D, Burton GJ (2016) Accreta placentation: A systematic review of prenatal ultrasound imaging and grading of villous invasiveness. Am J Obstet Gynecol 215 (6): 712-721.
- Gziri MM, Goffin F, Debieve F, Amant F (2013) Cancer diagnosis during pregnancy: importance of a national and European registration. Rev Med Liege 68 (10): 527-530.
- Maggen C, Van GM, Van CK, Vandenbroucke T, Amant F (2019) Management of cancer during pregnancy and current evidence of obstetric, neonatal and pediatric outcome: A review article. Int J Gynecol Cancer.
- Amant F, Deckers S, Van CK, Loibl S, Halaska M, et al. (2010) Breast cancer in pregnancy: recommendations of an international consensus meeting. Eur J Cancer 46 (18): 3158-3168.
- Amant F, Han SN, Gziri MM, Vandenbroucke T, Verheecke M, et al. (2015) Management of cancer in pregnancy. Best Pract Res Clin Obstet Gynaecol.
- Aviles A and Neri N (2001) Hematological malignancies and pregnancy: A final report of 84 children who received chemotherapy in utero. Clin Lymphoma 2 (3): 173-177.
- Lambrechts S, Van CK, Capoen A, Op de BK, Joniau S, et al. (2011) Polypoid endometriosis of the bladder during pregnancy mimicking urachal carcinoma. Ultrasound Obstet Gynecol 38 (4): 475-478.
- Molina JR, Quevedo JF, Furth AF, Richardson RL, Zincke H, et al. (2007) Predictors of survival from urachal cancer: a Mayo Clinic study of 49 cases. Cancer 110 (11): 2434-2440.
- Goldman H, Sowter S (2016) Urachal adenocarcinoma incidentally discovered in a young woman at elective caesarean section. BMJ Case Rep 2016.
- Church E, Dieh A (2013) A rare case of aggressive squamous cell carcinoma of the bladder in pregnancy. Obstet Med 6 (4): 182-183.
- McNally L, Osmundson S, Barth R, Chueh J (2013) Urachal duct carcinoma complicating pregnancy. Obstet Gynecol 122 (2 Pt 2): 469-472.
- Yeaton-Massey A, Brookfield KF, Aziz N, Mrazek-Pugh B, Chueh J (2013) Maternal bladder cancer diagnosed at routine first-trimester obstetric ultrasound examination. Obstet Gynecol 122 (2): 464-467.
- Lakmichi MA, Zehraoui R, Dahami Z, Moudouni SM, Bassir A, et al. (2012) Bladder cancer in the second trimester of pregnancy: tough decisions. A case report with review of the literature. Ther Adv Urol 4 (3): 139-142.
- Khochikar MV (2010) Management of urological cancers during pregnancy. Nat Rev Urol 7 (4): 195-205.
- Van CK, Van MK, Joniau S, Oyen R, Hanssens M, et al. (2006) Urachal carcinoma during pregnancy. Urology 67 (6): 1290-21.
- Sheldon CA, Clayman RV, Gonzalez R, Williams RD, Fraley EE (1984) Malignant urachal lesions. J Urol 131 (1): 1-8.
- Jung HA, Sun JM, Park SH, Kwon GY, Lim HY (2014) Treatment Outcome and Relevance of Palliative Chemotherapy in Urachal Cancer. Chemotherapy 60 (2): 73-80.
- Mertens LS, Behrendt MA, Mehta AM, Stokkel L, De JJ, et al. (2019) Long-term survival after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) for patients with peritoneal metastases of urachal cancer. Eur J Surg Oncol 45 (9): 1740-1744.
- Collazo-Lorduy A, Castillo-Martin M, Wang L, Patel V, Iyer G, et al. (2016) Urachal carcinoma shares genomic alterations with colorectal carcinoma and may respond to epidermal growth factor inhibition. Eur Urol 70 (5): 771-775.